Introduction: The DO Pathway in an ACGME World
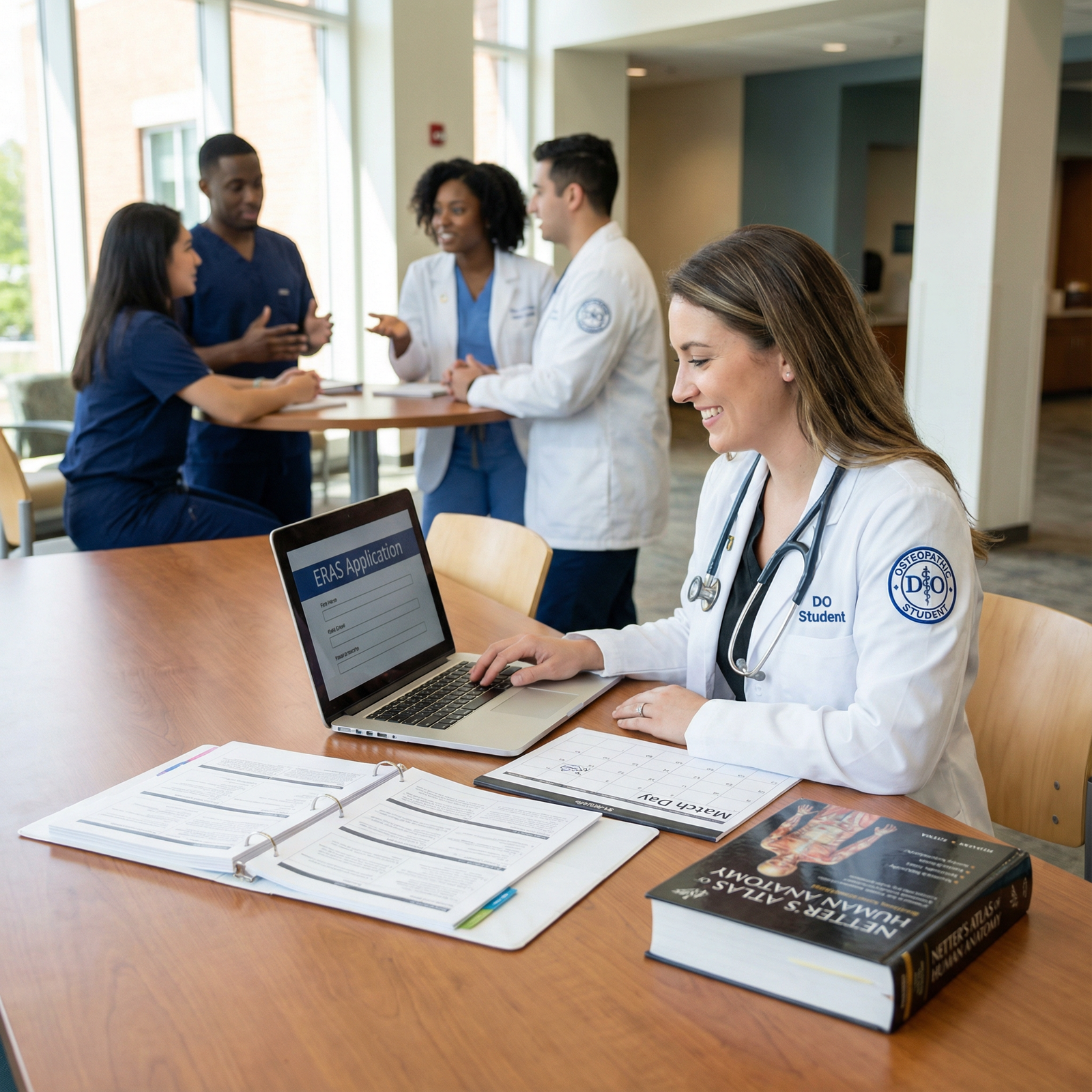
Transitioning from medical school to residency is one of the most high‑stakes phases of your career. For a Doctor of Osteopathic Medicine (DO), the landscape has evolved dramatically with the single Accreditation Council for Graduate Medical Education (ACGME) accreditation system. Today, DO and MD graduates compete side‑by‑side for the same ACGME Residency positions—offering more opportunity, but also more complexity and competition.
This Residency Application Guide is designed specifically for DO students navigating:
- ACGME Residency programs
- Choices about USMLE vs COMLEX (or both)
- Strategic Clinical Rotations and audition electives
- Strong networking in medicine and mentorship
- The full ERAS and Match process, including SOAP
Whether you are a first‑year student planning ahead or a fourth‑year finalizing applications, this expanded guide will help you understand the system, avoid pitfalls, and position yourself as a standout osteopathic applicant.
Understanding ACGME Residency Programs as a DO
What Is ACGME and the Single Accreditation System?
The Accreditation Council for Graduate Medical Education (ACGME) sets standards and accredits residency and fellowship programs in the U.S. Historically, there were separate accreditation systems for MD (ACGME) and DO (AOA) programs. With the transition to a single accreditation system (fully implemented by 2020):
- Former AOA programs converted to ACGME accreditation or closed.
- DOs and MDs now apply through the same Match and ERAS system.
- DO graduates are explicitly recognized as eligible trainees in all ACGME programs.
This integration has increased transparency and widened access for DOs but has also intensified competition, especially in highly sought‑after specialties (e.g., dermatology, orthopedic surgery, radiology, ENT).
Why ACGME Residency Is Important for DO Graduates
Pursuing an ACGME Residency as a Doctor of Osteopathic Medicine offers several key advantages:
Broader Specialty Options
- Access to virtually all U.S. residency specialties and subspecialties.
- Easier progression into ACGME‑accredited fellowships (e.g., cardiology, GI, critical care).
Standardized Recognition
- Many employers, hospitals, and academic centers are most familiar with ACGME standards.
- ACGME training can smooth credentialing, hospital privileges, and interstate mobility.
Interprofessional Training Environment
- Training alongside MD colleagues fosters collaboration and mutual respect.
- Lets you model and advocate for the osteopathic philosophy within diverse teams.
Future Career Flexibility
- ACGME training is often expected for competitive fellowships, academic medicine, and leadership roles.
- For DOs interested in research‑heavy careers, ACGME academic centers can provide stronger infrastructure.
DO vs MD in the ACGME Context
DOs and MDs are both fully licensed physicians, but DO training weaves in:
- Osteopathic manipulative medicine (OMM/OMT)
- A holistic, patient‑centered, and preventive care focus
- Emphasis on musculoskeletal and biomechanical health
In an ACGME Residency, your DO background is an asset if you can clearly articulate:
- How osteopathic training enhances your clinical reasoning and patient care
- When and how you use OMT (if relevant to your specialty)
- Your commitment to evidence‑based, team‑based medicine
Laying the Groundwork: Preclinical and Early Clinical Years

Academic Performance and Class Rank
For ACGME Residency programs, your transcript and Medical Student Performance Evaluation (MSPE) matter more than many students realize.
Action steps:
- Prioritize Foundations: Strong preclinical grades help your MSPE narrative and demonstrate discipline.
- Know Your School’s Metrics: Understand whether your school uses pass/fail, tiered grades, or ranking. Tailor your strategy accordingly.
- Address Weakness Early: If you struggle in a course, seek tutoring, faculty support, or study groups early rather than after an exam failure.
Programs often look for upward trends. If you had a rough first semester or year, a sustained improvement curve, plus honest reflection in your application, can mitigate early struggles.
Board Exams: USMLE, COMLEX, or Both?
As a DO, you must pass COMLEX to graduate and become licensed. The question is whether to also take USMLE.
Key considerations:
Program Preferences Vary:
- Some competitive specialties and academic programs strongly prefer or “require” USMLE scores.
- Many programs now openly accept COMLEX alone, but some still struggle to interpret it.
USMLE Step 1 and Step 2 CK:
- Step 1 is now pass/fail—but a pass from a DO student may still be scrutinized differently if Step 2 CK is weak.
- Step 2 CK has become a major numeric differentiator.
COMLEX Level 1 and Level 2‑CE:
- Ensure you understand conversion tools and percentile data.
- Programs increasingly receive conversion guidelines but not all use them consistently.
Actionable advice:
If aiming for a highly competitive specialty or academic center:
Strongly consider taking both COMLEX and USMLE (at least Step 2 CK) if your school permits and preparation time allows.If focused on primary care or community programs:
COMLEX alone can be sufficient, especially if you perform well and choose programs that explicitly welcome COMLEX‑only applicants.Avoid underprepared attempts:
A poor USMLE attempt can hurt far more than no score at all. Discuss strategy with advisors experienced in ACGME Residency placements for DOs.
Strategic Clinical Rotations for DO Students
Clinical Rotations are where your application truly comes to life. They influence:
- MSPE narrative
- Letters of Recommendation (LORs)
- Your specialty choice and competitiveness
- Networking in medicine with attendings and residents
Choosing Core Rotations
Your third‑year core Clinical Rotations (IM, surgery, peds, OB/GYN, psych, FM) are crucial:
- Aim for honors or top evaluations, especially in specialties you’re considering.
- Treat every rotation as a 4‑week interview—residents and attendings remember standout students.
- Ask for mid‑rotation feedback and actively correct any identified issues.
Audition and Away Rotations
For many specialties, “auditions” (sub‑internships or away rotations) at ACGME Residency programs can be game‑changers:
Timing:
- Typically done late third year or early fourth year.
- Apply early through VSLO or program‑specific portals.
Targets:
- Prioritize programs and geographic regions where you would truly be happy matching.
- Include at least one rotation at a program where your metrics are clearly competitive.
Goals of an away rotation:
- Demonstrate your clinical skills, work ethic, and professionalism.
- Build relationships to secure strong LORs.
- Assess whether the program culture fits you.
Securing Strong Letters of Recommendation (LORs)
High‑quality LORs often differentiate applicants with similar metrics.
Recommendations:
Who to Ask:
- Attendings in your chosen specialty who have directly supervised you.
- Faculty with ACGME affiliation or fellowship training, especially if they are known in the specialty.
- A department chair or program director when possible.
How to Ask Effectively:
- Request a “strong, enthusiastic letter of recommendation”—this phrasing gives faculty an out if they can’t be enthusiastic.
- Provide your CV, draft personal statement, and a brief bullet list of cases or contributions they observed from you.
Building a Competitive Residency Application Portfolio
Research, Scholarly Activity, and Quality Improvement
Not all applicants need first‑author publications in high‑impact journals. However, some level of scholarly work is increasingly expected, even for less competitive fields.
Options include:
- Clinical research projects
- Case reports or case series
- Quality improvement (QI) projects
- Educational posters or presentations
- Osteopathic‑focused research or OMT studies (especially helpful if applying to programs that value your DO identity)
Practical tips:
- Join projects early—ideally during preclinical or early clinical years.
- Start simple: case reports, retrospective chart reviews, or QI are often more accessible.
- Present at local/regional conferences if national meetings feel out of reach initially.
- Document everything: abstracts, posters, oral presentations, student research awards.
Research also provides natural networking in medicine: your mentors may advocate for you, introduce you to colleagues, or alert you to upcoming openings.
Networking in Medicine and Mentorship
Networking in medicine is not superficial—it’s about creating genuine, professional relationships that can guide and support your path.
Key strategies:
Join Specialty Societies:
- E.g., ACOFP, ACOI, AOAO, or the MD‑side equivalents (AAFP, ACP, AAOS).
- Attend sessions specifically for medical students.
Conferences and Local Meetings:
- Ask research mentors if you can attend or present with them.
- Introduce yourself to program directors and residents, but be respectful of their time.
Mentorship Structure:
- Seek at least one DO mentor and one mentor within your desired specialty (DO or MD).
- Schedule periodic check‑ins and ask pointed questions about your competitiveness and application strategy.
Strong mentors can:
- Help refine your specialty choice
- Give honest feedback on your application
- Advocate for you with colleagues and ACGME programs
Crafting a High‑Impact Personal Statement
Your personal statement should complement—not duplicate—your CV and experiences.
Content suggestions:
Your Origin Story:
- Why medicine, and why the DO path specifically?
- How your osteopathic education has shaped your view of patient care.
Your Specialty Fit:
- Concrete examples from Clinical Rotations that sparked or confirmed your interest.
- Traits you bring to the specialty (e.g., manual skills in OMT for sports med, holistic focus in family medicine).
Alignment with ACGME Residency Training:
- Show that you understand the demands of residency (long hours, team‑based care, responsibility for acutely ill patients).
- Emphasize resilience, teachability, and commitment to evidence‑based practice.
Osteopathic Values Without Stereotypes:
- Move beyond generic phrases like “holistic care.”
- Use real stories where you considered the whole person—social context, mental health, lifestyle, and biomechanics.
Tailoring:
- You can create one “core” statement per specialty, then lightly customize for specific programs (e.g., mention community focus, academic strengths, or osteopathic track if present).
Interview Preparation and Mock Interviews
Residency interviews are where programs decide whether they can see themselves working with you for the next 3–7 years.
Preparation strategy:
Mock Interviews:
- Practice with faculty, mentors, your school’s career office, or peers.
- Record sessions (with permission) to evaluate your tone, pace, and body language.
Common Question Types:
- “Tell me about yourself” / “Walk me through your CV.”
- “Why this specialty?” / “Why our program?”
- Ethical scenarios and conflict resolution.
- Questions about failures (e.g., low exam score, leave of absence).
Program‑Specific Preparation:
- Review the program’s website, mission, patient population, and curriculum.
- Identify unique features you genuinely value (e.g., osteopathic track, strong OMT clinic, global health opportunities).
During the interview:
- Be ready to explain your DO training and how OMT fits into your future practice—no matter the specialty.
- Display curiosity and humility: ask thoughtful questions, not just about prestige or fellowship match lists.
- Be professional and kind to everyone—from coordinators to residents. Many programs heavily weigh resident feedback.
Navigating ERAS, The Match, and SOAP as a DO

Submitting Your Application via ERAS
The Electronic Residency Application Service (ERAS) is the standard portal for ACGME Residency applications.
Key components:
- ERAS Common Application Form (CAF)
- Personal statement(s)
- Curriculum vitae (within CAF)
- Letters of recommendation (uploaded by writers)
- Medical school transcript
- MSPE (Dean’s letter)
- USMLE/COMLEX score reports
- Photo (professional, head‑and‑shoulders)
Timeline considerations:
- Start drafting your CV and personal statement at least 3–4 months before ERAS opens for submission.
- Request LORs early; faculty are often busiest during the same months you need letters.
- Double‑check that your application clearly denotes your Doctor of Osteopathic Medicine degree and board exams taken.
Specialty and Program Selection Strategy
Choosing where to apply is just as important as what you submit.
Guidelines:
- Use tools like NRMP Charting Outcomes, FREIDA, and your school’s match data to benchmark your competitiveness.
- Apply broadly if:
- Your board scores or grades are below average for your specialty.
- You’re targeting competitive fields or desirable geographic areas.
- Include a balanced mix of:
- Reach programs (highly competitive)
- Reasonable targets (aligned with your stats)
- Safety programs (where your metrics are clearly above their typical range)
Pay attention to:
- Whether programs explicitly welcome DOs / COMLEX
- Presence of DO faculty or an osteopathic recognition track
- Program’s past history of matching DO graduates
The Match and Rank Order List (ROL)
After interviews, you will submit a Rank Order List through NRMP.
Tips:
- Rank programs in true order of preference, not where you think you’re most likely to match. The algorithm is applicant‑favoring.
- Don’t rank a program you would not actually want to attend.
- Discuss your list with trusted mentors; they can help you weigh program strengths vs your goals.
SOAP: A Safety Net, Not a Plan A
If you remain unmatched after the initial Match algorithm, you may be eligible for the Supplemental Offer and Acceptance Program (SOAP).
Preparation:
- Before Match Week, identify programs that historically participate in SOAP and could be a good fit if needed.
- Keep updated versions of:
- A brief, SOAP‑ready personal statement
- A condensed list of experiences and strengths
- Stay in touch with advisors who can help you pivot quickly if SOAP becomes necessary.
During SOAP:
- Be flexible about specialty and geography; many applicants pivot to preliminary or transitional year positions, or to a different but related specialty.
- Maintain professionalism—SOAP moves quickly, and program impressions still matter for future opportunities.
Maximizing Your Competitiveness as a DO Applicant
Highlighting Your Unique Osteopathic Identity
Your DO training is not something to hide; it’s a differentiator.
Ways to emphasize it constructively:
- Discuss OMT cases where you meaningfully impacted patient outcomes (even if your future specialty won’t involve frequent OMT).
- Show how osteopathic principles guide your approach to complex patients with overlapping physical, mental, and social issues.
- If your school or rotations include osteopathic recognition tracks, mention your participation and what you learned.
Demonstrating Professionalism and Resilience
Residency programs value applicants who:
- Handle stress and setbacks with maturity
- Learn from mistakes
- Communicate honestly and professionally
Examples to highlight:
- Overcoming a board exam failure or low score (with a documented pattern of improvement)
- Balancing personal challenges with academic responsibilities
- Leadership roles in student organizations, clinics, or QI projects
Service, Leadership, and Community Engagement
Service work aligns particularly well with the DO mission and can be a strong asset:
- Free clinics, rural outreach, mobile health units
- Health education, public health initiatives, advocacy work
- Leadership roles in osteopathic or specialty societies
Describe not only what you did, but:
- What you learned about your patients and communities
- How the experience changed your clinical approach
- How you’ll continue similar work during residency
FAQ: Common Questions About ACGME Residency for DO Students
1. Do I need to take USMLE in addition to COMLEX to match into an ACGME Residency?
Not always, but it can help. Many ACGME programs now accept COMLEX alone and are increasingly familiar with interpreting it. However:
- Competitive specialties and academic centers may still prefer or expect USMLE scores.
- If your target programs explicitly state they require or strongly recommend USMLE, you should plan to take it—but only if you can prepare adequately.
Talk with mentors and review target program requirements before deciding.
2. How many ACGME Residency programs should I apply to as a DO?
It depends on your specialty, competitiveness, and geographic flexibility. As a rough guide:
- Less competitive specialties (e.g., family medicine, internal medicine, pediatrics):
15–30 well‑chosen programs may be sufficient for strong applicants; others may apply to 30–50+. - More competitive specialties (e.g., ortho, derm, ENT, radiology):
Many DO applicants apply to 60–100+ programs, balancing reach, target, and safety.
Use your school’s match data and NRMP resources to tailor your application scope.
3. How can I identify ACGME Residency programs that are DO‑friendly?
Look for:
- Programs that list DO graduates or faculty on their websites.
- NRMP match lists or program statistics showing a history of matching DOs.
- Explicit statements in program descriptions welcoming Doctor of Osteopathic Medicine applicants.
- Osteopathic recognition tracks or clinics incorporating OMT.
You can also ask residents or mentors who know the specialty which programs are particularly supportive of DOs.
4. What if my COMLEX or USMLE scores are below average?
You can still match, but you’ll need a more strategic approach:
- Strengthen other components: LORs, clinical evaluations, research, and service.
- Consider slightly less competitive specialties or more geographically diverse programs.
- Use away rotations to prove your clinical skills and secure strong letters.
- Be transparent (when asked) about what you learned from the setback and how you improved your study strategies.
Work closely with advisors to create a realistic, data‑driven application plan.
5. Can I still use OMT during an ACGME Residency?
Yes, though how often depends on your specialty and program culture:
- Primary care specialties (FM, IM, pediatrics) may offer more natural opportunities for OMT.
- Some ACGME programs have osteopathic recognition, OMT clinics, or faculty who actively practice OMT.
- Even in procedure‑heavy or hospital‑based specialties, OMT skills can be useful for specific cases and patient comfort.
During interviews, ask programs about their openness to OMT and whether they have DO faculty mentors.
By understanding the structure of ACGME Residency training, planning early, and leveraging the strengths of your Doctor of Osteopathic Medicine education, you can build a compelling application and successfully navigate the Match. Your osteopathic background is not simply a credential—it’s a clinical perspective and a philosophy that can enrich any ACGME program you join.




















