
Introduction: Why Blockchain Matters for the Future of Healthcare
The digital transformation of healthcare has created unprecedented opportunities—and equally unprecedented risks. Electronic health records, telehealth platforms, wearable devices, and genomics all generate massive amounts of sensitive data. When this data is poorly protected or fragmented across systems, it undermines patient trust, exposes organizations to cyberattacks, and hinders coordinated care.
Blockchain technology has emerged as a serious contender to address these issues. Beyond its association with cryptocurrencies, blockchain offers a new way to manage healthcare data security, interoperability, and Patient Empowerment at scale. Properly implemented, it can help ensure that critical health information is accurate, tamper-evident, and available to the right people at the right time—while still respecting privacy and regulatory requirements.
This article provides a deeper, clinically relevant overview for medical students, residents, and early-career clinicians. We will explore:
- What blockchain is and how it actually works in a healthcare context
- Key benefits for Data Security, Interoperability, and patient-centered care
- Real-world use cases and pilot projects
- Major challenges, including regulatory and technical barriers
- Strategic directions for the future of blockchain in healthcare
Understanding these concepts will help you critically evaluate future systems you’ll use as a clinician, participate in innovation projects, and advocate for solutions that keep patients and providers at the center.
Understanding Blockchain Technology in a Clinical Context
Blockchain is often described in technical jargon, but its core idea is straightforward: it is a shared, tamper-resistant database maintained by multiple parties who may not fully trust one another.
How Blockchain Works: Core Concepts for Healthcare
At its core, blockchain is a type of distributed ledger technology (DLT) with three foundational concepts:
Blocks and Chains
- Data (such as transactions, events, or access logs) is grouped into blocks.
- Each block contains:
- A list of transactions
- A timestamp
- A cryptographic hash of the previous block
- The hash links blocks together into a “chain,” making any alteration to historical data easily detectable.
Decentralization
- Instead of a single central database (e.g., one hospital’s server), copies of the ledger are stored on multiple nodes (computers) across a network.
- Each node has a synchronized copy of the ledger, reducing single points of failure and making it harder for attackers to corrupt the data.
Consensus Mechanisms
- Nodes must agree on which new blocks are valid.
- In healthcare, this usually involves permissioned (private or consortium) blockchains where only approved organizations (hospitals, payers, regulators) can validate transactions, using efficient consensus protocols (e.g., Proof of Authority, Practical Byzantine Fault Tolerance).
Features That Map Directly to Healthcare Needs
Several properties of blockchain align closely with long-standing healthcare pain points:
Immutability and Auditability
Once a transaction is added to the blockchain, it cannot be modified without leaving a clear trace. For healthcare, this supports:- Reliable medication and allergy histories
- Tamper-evident research data
- Robust audit trails for regulatory compliance (e.g., HIPAA)
Cryptographic Security
Blockchain uses public-key cryptography so that:- Data can be encrypted such that only authorized parties with the correct keys can decrypt it.
- Digital signatures verify who created or approved a transaction, supporting non-repudiation (e.g., confirming which clinician signed a note).
Programmability via Smart Contracts
Smart contracts are self-executing code stored on the blockchain that runs when predefined conditions are met. In healthcare, they can:- Automate insurance pre-authorization rules
- Enforce consent directives for data sharing
- Trigger reimbursement when clinical or quality criteria are satisfied
Public vs. Private Blockchains in Healthcare
For clinical applications, it is crucial to distinguish:
Public Blockchains (e.g., Bitcoin, Ethereum mainnet)
- Open to anyone; fully transparent.
- Typically not suitable for directly storing protected health information (PHI).
Private/Permissioned Blockchains
- Access restricted to vetted participants (e.g., specific health systems, labs, payers).
- Better suited for regulatory compliance and PHI-related workflows.
- Offer more control over governance, access rights, and performance.
Most current healthcare projects use permissioned blockchains because they combine the advantages of DLT with the governance and privacy controls required by healthcare regulations.
Key Benefits of Blockchain in Healthcare
Blockchain is not a magic fix for all IT problems, but it offers distinct advantages when the goals are secure data sharing, trustworthy records, and cross-organizational collaboration.
1. Enhanced Data Security and Integrity
Healthcare is a prime target for cyberattacks because medical records are valuable on the black market and often stored in fragmented, poorly protected systems.
Blockchain supports Data Security in several ways:
Distributed Storage Reduces Single Points of Failure
In traditional systems, a compromised central server can expose millions of records. In blockchain-based designs:- The ledger is replicated across multiple nodes.
- Compromising one node does not compromise the entire network.
Tamper-Evident Logs
Attempts to alter historical records (e.g., to hide inappropriate chart access or research misconduct) would require modifying numerous blocks across many nodes—a prohibitive task in a properly designed system.Strong Access Controls
When combined with modern encryption and access-control layers:- Patient data can be tokenized or referenced by hashes rather than stored in plaintext.
- Access rights (who can see what and when) can be codified and enforced via smart contracts.
For residents and clinicians, this could mean greater confidence in the integrity of medication lists, lab histories, and clinical documentation—particularly when caring for patients seen at multiple institutions.
2. Improved Interoperability Across the Care Continuum
Interoperability—getting systems to “talk to each other”—remains one of healthcare’s biggest challenges. Different EHR vendors, incompatible standards, and siloed data often mean:
- Duplicated imaging and lab tests
- Delayed or incomplete referrals
- Poor care coordination for patients with complex, multi-system disease
Blockchain can serve as a shared, neutral infrastructure layer that:
Links Records Across Organizations
Instead of storing PHI directly, the blockchain can store:- Pointers (hashes) to off-chain records
- Metadata describing where data lives and what type it is
- Access permissions and consent directives
This allows different systems to discover and retrieve records securely, even when they use different vendors or architectures.
Standardizes Transactions Rather Than Databases
Blockchain does not need to replace every EHR. Instead, it can:- Standardize how events (e.g., new lab result, medication change, discharge summary) are recorded and signaled.
- Enable EHRs, pharmacy systems, and payer systems to subscribe to and act on shared events reliably.
The result is more complete, longitudinal patient records accessible at the point of care, regardless of where prior events occurred.
3. Patient Empowerment and Data Ownership
Traditional healthcare IT often treats patients as passive data subjects rather than active managers of their own information. Blockchain offers tools for meaningful Patient Empowerment:
Granular Consent Management
Patients can:- Grant or revoke access for specific providers or organizations.
- Allow limited-time access (e.g., for a pre-op consultation).
- Permit data use for research under clearly defined conditions.
Unified View of Health Data
Using blockchain-based identity and metadata, patients could access:- EHR data from multiple health systems
- Wearable and home monitoring data
- Genomic reports and imaging summaries
in a single personal health record app, with cryptographic proof of authenticity.
Data-Sharing for Research and Public Health
Patients may choose to share de-identified or tokenized data for:- Clinical research
- AI model development
- Public health surveillance
while: - Receiving transparency about how data is used
- Potentially gaining incentives (e.g., digital tokens, reduced premiums)
For clinicians, patient-controlled access can increase trust and improve history-taking when patients know exactly who can see their data and why.
4. Streamlined Administrative and Financial Workflows
Administrative complexity is a major source of healthcare waste and clinician frustration. Blockchain can simplify many workflows:
Identity and Credential Verification
A blockchain-based identity layer can:- Verify clinician credentials across institutions (licenses, board certifications).
- Speed up onboarding and reduce repetitive paperwork.
- Support secure single sign-on across multiple systems.
Claims Processing and Prior Authorization
Smart contracts can:- Automatically verify coverage rules.
- Trigger payments when claim data meets predefined criteria.
- Reduce disputes and manual reviews.
Supply Chain Management
End-to-end tracking of medications, biologics, and devices can:- Reduce counterfeit or diverted products.
- Improve recall management.
- Provide real-time inventory visibility across sites.
These efficiencies can lower administrative burden and costs, potentially freeing resources for direct patient care.
5. More Trustworthy Clinical Trials and Research
Research depends on high-quality, trustworthy data. Blockchain supports:
Immutable Study Records
Time-stamped, tamper-evident logging of:- Patient enrollment and consent
- Protocol amendments
- Adverse events
- Data analyses and outputs
Transparent Data Sharing and Provenance
Researchers and regulators can:- Trace data lineage (where it came from, who touched it).
- Verify that endpoints and analytic methods match pre-registered protocols.
This improves the credibility of results and can facilitate multi-center collaborations.
For trainees involved in research, blockchain-based tools could make it easier to document study workflows, manage multi-institutional data, and support reproducible science.
Current Real-World Applications of Blockchain in Healthcare
While full-scale nationwide implementations are still emerging, numerous pilots and early deployments illustrate how blockchain is being tested in healthcare systems today.
1. MedRec (MIT Media Lab)
Focus: Decentralized management of medical records metadata
- MedRec uses blockchain to manage permissions and pointers to medical data rather than storing PHI directly on-chain.
- Patients can:
- See which providers hold their data
- Grant or revoke access
- Providers can access a distributed index of records, improving continuity of care and Interoperability across systems.
MedRec’s approach demonstrates how blockchain can function as a coordination and consent layer atop existing EHRs.
2. Chronicled and Pharmaceutical Supply Chain Security
Focus: Securing the drug supply chain
- Chronicled uses blockchain to:
- Track prescription drugs from manufacturer to wholesaler, pharmacy, and ultimately to patients.
- Create a shared, tamper-evident log of product movements and ownership changes.
- This helps:
- Combat counterfeit drugs—a major global safety issue.
- Ensure cold-chain integrity for temperature-sensitive medications.
- Support regulatory compliance (e.g., DSCSA in the U.S.).
Residents prescribing expensive biologics or controlled substances could benefit from knowing that medications reaching patients are authentic and traceable.
3. MyCo: Decentralized Patient Identity and Data Access
Focus: Patient-centric identity and data sharing
- MyCo (representative of similar initiatives) uses blockchain-based identity systems to:
- Assign unique, verifiable digital identities to patients.
- Facilitate secure linking of clinical, payer, and personal data.
- Patients can:
- Log in to multiple healthcare services with a single, verified identity.
- Control which organizations can pull their records.
This model supports Patient Empowerment and reduces fragmentation caused by multiple, inconsistent patient identifiers.
4. VeChain: Transparency in Pharmaceutical and Medical Device Supply Chains
Focus: Supply chain transparency and product lifecycle management
- VeChain provides blockchain-based tools for:
- Tracking manufacturing details, shipping routes, and distribution channels for drugs and devices.
- Storing quality control data and certificates.
- Healthcare organizations can:
- Verify authenticity and batch history at the point of care.
- Quickly trace and isolate affected lots in recalls.
This level of transparency enhances safety and trust, especially for high-risk products like implantable devices.
5. Guardtime and Estonia’s National Health Records
Focus: National-level health data integrity
- Estonia has implemented a blockchain-like infrastructure (via Guardtime) to:
- Secure national health records, among other public services.
- Provide cryptographic proof that records have not been altered improperly.
- Benefits include:
- Strong assurance of data integrity for clinicians and patients.
- Central visibility for regulators and auditors without direct access to PHI.
Estonia’s experience illustrates what a national-scale, blockchain-backed health data ecosystem might look like in practice.
Challenges and Limitations in Adopting Blockchain in Healthcare
Despite its potential, blockchain adoption in healthcare faces substantial barriers. For clinicians and future leaders, understanding these constraints is crucial for realistic planning and advocacy.
1. Integration with Legacy Health IT Systems
Healthcare IT environments are notoriously complex:
- Multiple EHR vendors within the same health system
- Legacy systems that predate modern standards
- Custom workflows deeply embedded in clinician practice
Adopting blockchain often requires:
- Building interfaces (APIs) between EHRs and the blockchain layer
- Migrating or mapping existing identifiers and data semantics
- Training IT staff, clinicians, and administrators on new workflows
These integration efforts require significant capital, time, and change management, which can be challenging for resource-constrained institutions.
2. Regulatory and Legal Uncertainty
Healthcare is heavily regulated, and blockchain raises novel questions for:
HIPAA, GDPR, and Similar Regulations
- How do “right to be forgotten” or data erasure requirements apply to immutable ledgers?
- Who is the data controller or custodian in a decentralized network?
Liability and Governance
- When multiple organizations share a blockchain, who is responsible if something goes wrong?
- How are disputes about incorrect or harmful data resolved?
Regulators worldwide are still refining guidance. Until clearer frameworks are established, many organizations will remain cautious, especially with PHI-heavy applications.
3. Balancing Transparency with Privacy
Blockchain’s transparency is a double-edged sword:
Pros:
- Easier auditing and verification
- Improved accountability
Cons:
- Risk of exposing sensitive metadata (e.g., that a patient has visited an oncology clinic) even if the content is encrypted
- Complex key management for patients and providers
Emerging strategies include:
- Storing only hashes and metadata on-chain, with actual PHI kept off-chain in secure data stores.
- Using advanced cryptography (e.g., zero-knowledge proofs) to validate transactions without revealing underlying data.
Designing systems that truly protect privacy while still enabling meaningful data use is an ongoing research and policy challenge.
4. Scalability and Energy Consumption
Early public blockchains (e.g., Bitcoin) are rightly criticized for high energy use and limited throughput. While healthcare projects typically use more efficient, permissioned networks, concerns remain:
- Can the network handle millions of patient events per day?
- How will performance scale as more organizations join?
- What is the environmental impact, and how does it align with healthcare’s sustainability goals?
New consensus mechanisms and side-chain architectures are addressing these issues, but careful design and piloting are essential before widespread deployment.
5. Limited Awareness and Technical Expertise
Many clinicians, administrators, and even IT leaders:
- Have only a vague understanding of blockchain, often conflated with cryptocurrency hype.
- Lack clear use cases or implementation roadmaps.
- Are already overloaded with other priorities (EHR optimization, quality reporting, telehealth).
Overcoming this requires:
- Targeted education for healthcare professionals
- Interdisciplinary teams (clinical + technical + legal)
- Realistic pilot projects that solve concrete problems rather than chasing buzzwords

The Future of Blockchain in Healthcare: Emerging Directions
As the technology and regulatory landscape mature, several trends are likely to shape blockchain’s role in the FUTURE_OF_HEALTHCARE.
1. From Pilots to Scaled, Collaborative Networks
Expect to see:
- Expansion of regional and national blockchain consortia involving:
- Hospitals and health systems
- Payers and pharmacy benefit managers
- Public health agencies and regulators
- More standardized frameworks for:
- Participant onboarding and governance
- Data formats and transaction types
- Dispute resolution and oversight
For trainees, this means the systems you use daily may gradually shift from institution-specific silos to interconnected health ecosystems.
2. Clearer Standards and Regulatory Guidance
Standards bodies and regulators are working on:
- Technical standards for:
- Blockchain-based identity and consent
- Clinical data pointers and hashes
- Policy guidelines that:
- Clarify how Data Security, privacy, and immutability fit with existing laws
- Define roles and responsibilities in decentralized networks
As these frameworks solidify, healthcare organizations will be more comfortable deploying mission-critical, blockchain-enabled systems.
3. Deepening Patient-Centered and Value-Based Care
Blockchain can support emerging care models by:
- Enabling patient-controlled health data wallets that travel with the individual across providers and borders.
- Facilitating value-based reimbursement:
- Smart contracts tying payment to verified outcomes or quality metrics.
- Transparent tracking of care pathways and interventions.
This infrastructure aligns with a shift toward continuous, personalized care rather than episodic, facility-centered encounters.
4. Integration with AI, Analytics, and Real-Time Monitoring
Combining blockchain with AI and advanced analytics opens new possibilities:
Trusted Data Pipelines for AI
- Immutable data trails improve the reliability of AI training datasets.
- Provenance information aids bias detection and model auditing.
Real-Time and Predictive Analytics
- Secure streaming of de-identified, aggregated data to analytics engines.
- Earlier detection of disease patterns, outbreaks, or safety signals.
Clinically, this could support personalized alerts, decision support, and more proactive population health management—while maintaining strong Data Security and auditability.
5. Toward Truly Interoperable Health Ecosystems
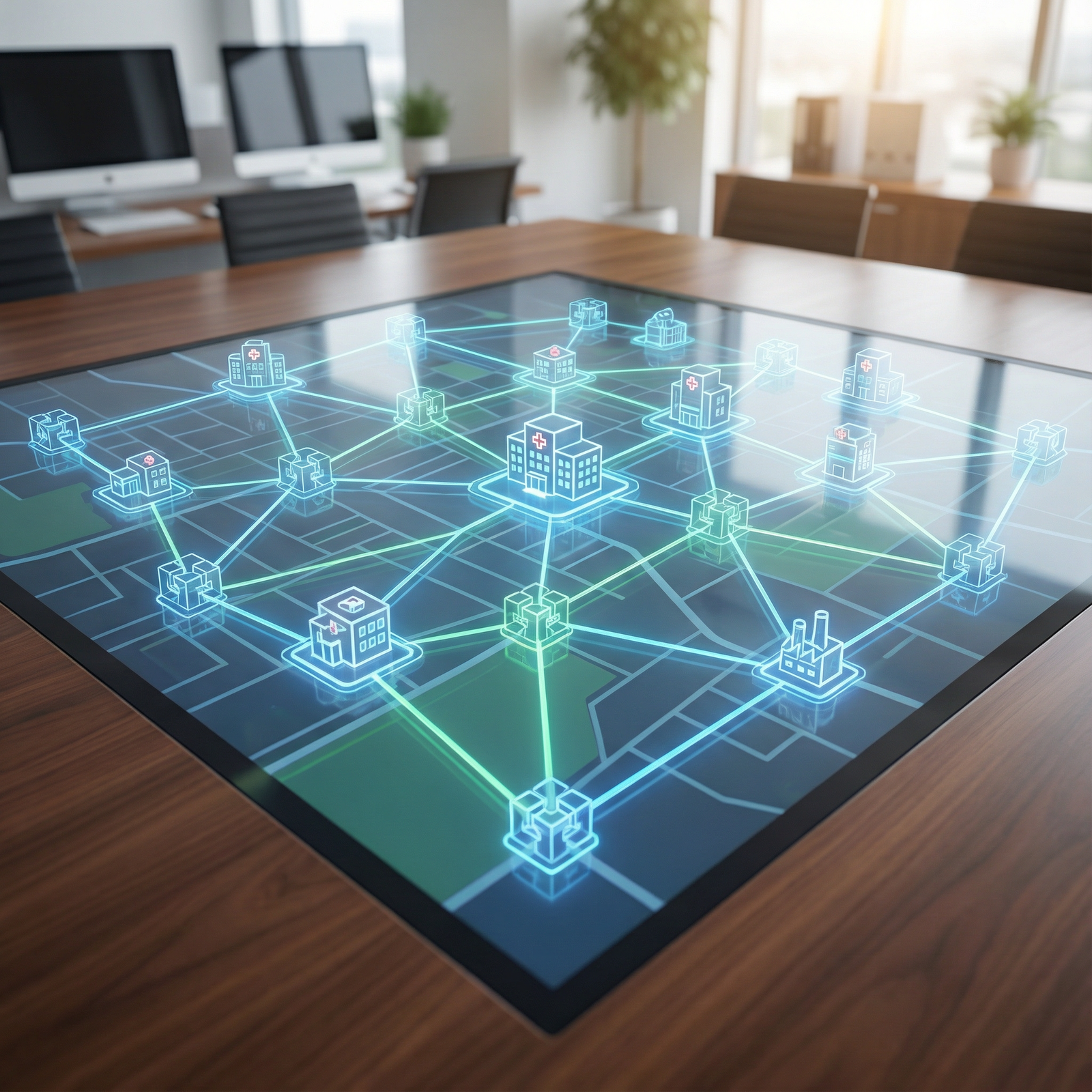
Ultimately, blockchain may function as the coordination backbone of a highly Interoperable healthcare environment:
- Cross-border health information exchange for travelers, migrants, and telehealth consults
- Integration of:
- Hospital and clinic EHRs
- Pharmacies and labs
- Wearables, home diagnostics, and remote monitoring tools
- Social determinants and community resources
For clinicians, this could mean far more complete, current, and trustworthy information at the point of care—reducing errors, duplication, and frustration.
FAQ: Blockchain, Healthcare, and Your Future Practice
1. Does blockchain mean all patient data will be public or on the internet?
No. In healthcare, most implementations use permissioned blockchains and store only encrypted references, hashes, or metadata on-chain. Actual PHI generally remains in secure, off-chain databases controlled by healthcare organizations. Blockchain’s role is to coordinate access, verify integrity, and maintain audit trails—not to broadcast PHI.
2. How could blockchain affect my day-to-day work as a clinician or resident?
If implemented well, you might see:
- Faster access to outside records when patients arrive from other systems
- Fewer repeated tests and more complete histories
- More transparent medication and device histories
- Reduced administrative delays (e.g., prior authorizations, credentialing)
Ideally, blockchain would operate “under the hood,” improving reliability and interoperability without adding clicks or complexity.
3. Is blockchain required for Interoperability, or can we solve it with existing standards alone?
Existing standards (e.g., HL7 FHIR) are crucial and will remain so. Blockchain is complementary, not a replacement. It provides:
- A trusted, shared ledger of events and permissions across organizations
- Stronger tamper-evidence and auditability
- A neutral governance layer for multi-party data exchange
In some cases, traditional databases and APIs suffice; blockchain is best used where shared trust and verifiable integrity across many stakeholders are critical.
4. What are the biggest risks of using blockchain for healthcare data?
Key risks include:
- Poorly designed systems that expose sensitive metadata or mishandle encryption keys
- Regulatory non-compliance if immutable records conflict with data deletion requirements
- Overhyped implementations that focus on technology rather than clinical value
Mitigating these requires rigorous security design, legal review, and close collaboration between clinicians, IT, and compliance teams.
5. How can medical students and residents get involved in blockchain and digital health?
Practical steps include:
- Learning core concepts of blockchain, Interoperability (e.g., FHIR), and Data Security
- Joining or starting digital health interest groups or hackathons at your institution
- Collaborating with informatics, computer science, or engineering departments on projects
- Participating in pilot studies or quality improvement initiatives that test new technologies
As future leaders, your input is vital to ensure these tools truly support—not hinder—patient care.
Blockchain is not a cure-all, but it offers a powerful set of tools for building a safer, more transparent, and genuinely patient-centered digital health ecosystem. As technology, policy, and clinical practice evolve together, clinicians who understand these foundations will be better equipped to shape systems that uphold trust, enhance care quality, and protect the patients we serve.


















