
Introduction: AI as a Clinical Partner, Not a Replacement
Artificial Intelligence (AI) has moved from buzzword to bedside. What began as experimental algorithms in research labs is now embedded in electronic health records, imaging platforms, and even patients’ smartphones. For medical students, residents, and practicing clinicians, understanding AI is no longer optional—it is becoming a core component of modern patient management and Healthcare Innovation.
In medicine, AI refers to computational systems that can learn from data, recognize patterns, and support decision-making in ways that augment human expertise. From boosting Diagnostic Accuracy in radiology to enabling Personalized Medicine in oncology and improving operational efficiency in hospitals, AI is steadily reshaping how care is delivered.
This enhanced overview will walk through:
- How AI emerged and matured in healthcare
- Key clinical applications, with emphasis on diagnostics and patient management
- The role of AI in personalized and precision medicine
- Impact on clinical decision-making and workflow
- Ethical, regulatory, and implementation challenges
- What the near future likely holds for trainees and clinicians
Throughout, the emphasis is practical: how these tools affect your day-to-day work with patients and how to engage with them critically and safely.
The Emergence of AI in Healthcare: From Concept to Clinical Tool
AI in healthcare is not brand-new, but its capabilities and reach have expanded dramatically in the last decade.
From Rule-Based Systems to Data-Driven Intelligence
Early “AI” systems in healthcare (1970s–1990s) were primarily rule-based expert systems. They encoded clinical logic using manually crafted “if-then” rules:
- Example: Early diagnostic decision aids such as MYCIN and INTERNIST-1
- Limitation: Difficult to maintain, struggled with real-world complexity, and required continuous manual updating
The modern AI revolution has been driven by:
- Machine learning (ML): Algorithms that improve with exposure to data
- Deep learning (DL): Neural networks with multiple layers that excel at pattern recognition (especially in images, waveforms, and unstructured text)
- Natural language processing (NLP): Systems that can interpret and generate human language (e.g., reading free-text clinical notes)
- Reinforcement learning: Algorithms that learn by trial and error with feedback, increasingly relevant in resource allocation and treatment optimization
Three major enablers pushed AI from theory to practice:
Explosion of digital healthcare data
- Widespread EHR adoption
- High-resolution imaging
- Genomics and multi-omics
- Wearables and remote monitoring devices
Affordable computing power
- GPUs and cloud computing capable of training massive models
Improved algorithms and open-source tools
- Frameworks like TensorFlow and PyTorch lowered the barrier to building and deploying AI solutions
Today, AI is woven into many clinical systems—often invisibly. Understanding where it is and how it works at a conceptual level is crucial for safe, effective use.
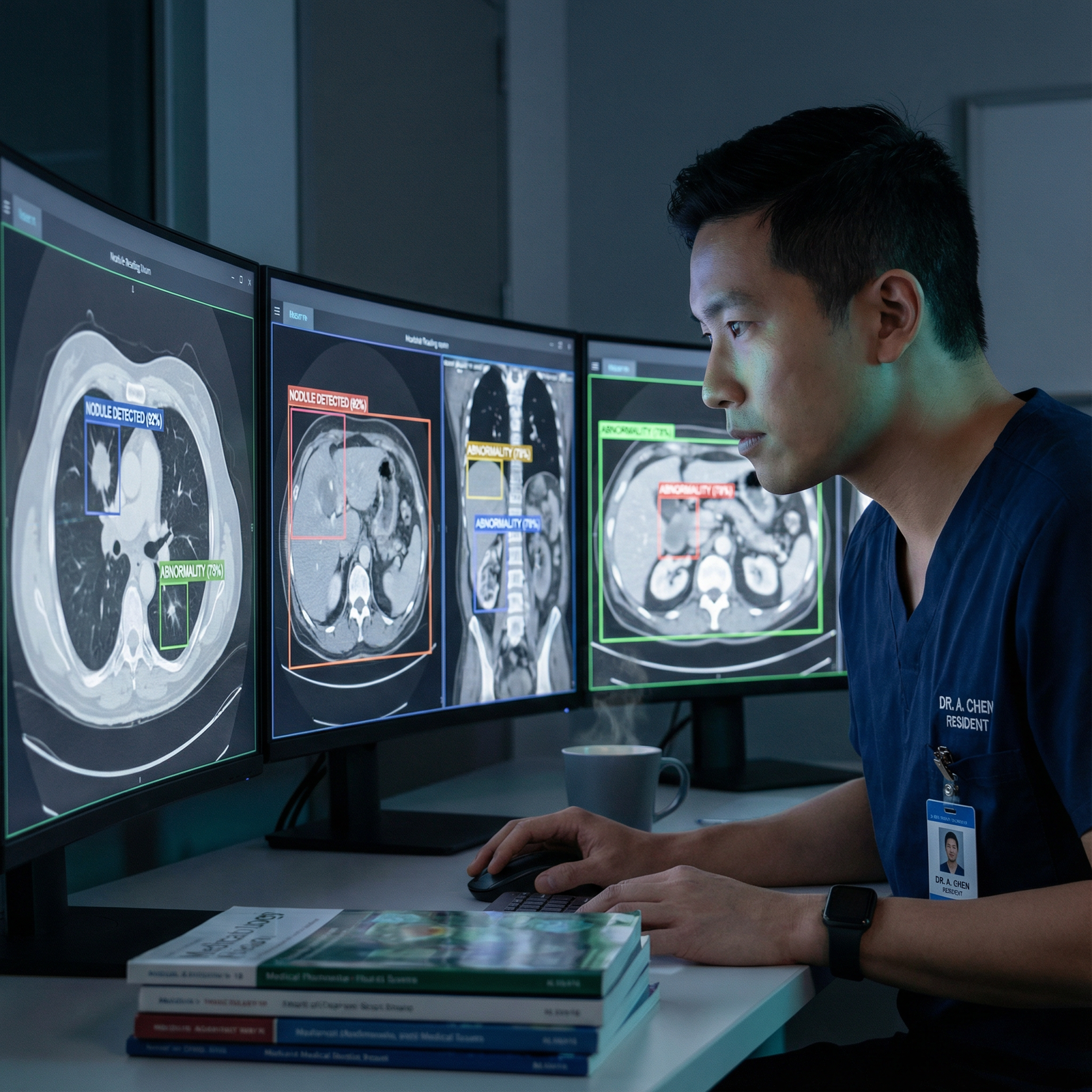
Enhancing Diagnostic Accuracy: AI as a Second Reader
One of the most prominent and mature domains for AI in healthcare is diagnosis, especially in imaging and pattern-based recognition. AI does not replace the clinician; it serves as a highly attentive, reproducible “second reader” that improves Diagnostic Accuracy and consistency.
AI-Powered Radiology and Medical Imaging
Radiology has been at the forefront of AI adoption for several reasons:
- Massive labeled datasets (e.g., chest X-rays, CT scans, MRIs)
- Clearly defined tasks, such as nodule detection or fracture identification
- High variability in human interpretation, especially under time and workload pressures
Key examples and applications:
- Breast imaging: Deep learning systems that detect breast cancer on mammograms and tomosynthesis, rivaling or even surpassing average radiologist performance in some studies
- Chest imaging: AI tools that flag potential pneumonia, pulmonary embolism, pneumothorax, or lung nodules, helping prioritize emergent findings
- Neuroimaging: Automated detection of hemorrhage, infarcts, and mass effect on CT/MRI, often integrated into stroke-alert workflows for rapid triage
For residents, this means:
- Emerging workflows where AI “pre-screens” studies and flags abnormalities
- AI-generated preliminary labels or segmentations that you must still verify
- Opportunities to focus more on complex cases and integrated reporting rather than routine normal studies
Importantly, AI can reduce intra- and inter-reader variability, offering a level of consistency that can be particularly valuable in high-volume settings.
Beyond Imaging: Multimodal Disease Detection
AI’s diagnostic power extends beyond imaging into other data types:
ECG and waveform analysis:
- Detection of arrhythmias, QT-prolongation, and subclinical atrial fibrillation
- Early detection of cardiomyopathy or heart failure risk from standard ECGs using deep learning
Dermatology:
- Smartphone-based applications that classify skin lesions with accuracy approaching dermatologists, assisting in triage and early detection of melanoma
Pathology and digital slides:
- Algorithms that identify cancerous regions, quantify tumor burden, and detect subtle histologic features, aiding pathologists in complex cases
Sepsis and deterioration prediction:
- EHR-based models that signal early warning of sepsis, acute kidney injury, or ICU transfer risk hours before traditional criteria
AI excels at identifying patterns in high-dimensional data (e.g., labs, vitals, notes) that humans might miss—especially when signals are subtle or distributed across multiple domains.
Transforming Patient Management and Clinical Operations
AI is not only about diagnosis; it is fundamentally changing how we manage patients across the continuum of care—from admission and triage to discharge and follow-up. For trainees, this increasingly affects daily workflow, handoffs, and care coordination.
Predictive Analytics for Proactive Patient Management
Predictive analytics use historical and real-time data to estimate the probability of future events, such as:
- Hospital readmission
- Clinical deterioration
- ICU transfer or need for mechanical ventilation
- Emergency department (ED) crowding and bed shortages
Concrete clinical examples:
Readmission risk scores: AI-enhanced models integrate comorbidities, prior utilization patterns, social determinants, and medication profiles to flag patients at high risk of 30-day readmission. This can trigger early involvement of case management, social work, and outpatient follow-up planning.
Deterioration and rapid response triggers: Instead of relying solely on traditional early warning scores, AI systems can continuously analyze vital signs, lab trends, nursing notes, and orders, and send alerts to rapid response teams before a patient crashes.
ED triage support: Machine learning models help prioritize which patients need immediate attention, imaging, or isolation, potentially reducing wait times and improving flow.
For residents and hospitalists, these tools can:
- Support risk stratification during rounds and sign-out
- Highlight which patients might benefit most from closer monitoring or early intervention
- Aid in resource allocation, particularly in high census or surge situations
However, clinicians must remain alert to alert fatigue and understand model limitations to avoid over-reliance or distrust based on poorly tuned implementations.
Virtual Health Assistants and Automation in Patient Engagement
AI-powered virtual health assistants, chatbots, and automated workflows are increasingly used to:
- Answer routine patient questions (e.g., medication instructions, pre-op prep)
- Assist with scheduling and appointment reminders
- Conduct symptom triage and guide patients to appropriate care settings
- Support chronic disease management (e.g., diabetes, hypertension) with educational content and behavior nudges
Examples:
- A chatbot that screens patients with respiratory symptoms, advising those with mild issues to manage at home and prompting high-risk patients to seek urgent care
- Automated text-message follow-up after ED discharge, tracking pain scores or wound healing and escalating concerning responses to clinicians
From a clinician’s perspective, well-designed AI tools in this space:
- Offload repetitive, low-complexity interactions
- Allow focus on high-acuity, high-complexity encounters
- Provide structured data on patient-reported outcomes between visits
At the same time, ensuring that these tools are culturally sensitive, accessible across languages, and designed with equity in mind is critical to avoid widening disparities.
AI and Personalized Medicine: Toward Truly Individualized Care
Personalized Medicine—often overlapping with precision medicine—seeks to match the right intervention to the right patient at the right time, based on their unique biology and context. AI is a core engine of this shift, enabling clinically useful insight from data that would otherwise be overwhelming.
Genomics, Multi-Omics, and Precision Oncology
High-throughput sequencing generates vast amounts of genomic and transcriptomic data. AI methods help convert these data into clinically actionable insights:
- Variant classification: AI models can help distinguish pathogenic from benign variants, aiding geneticists and clinicians in interpreting complex panels and whole-exome/genome sequencing.
- Molecular tumor boards: In oncology, AI can analyze tumor genomics, prior treatments, and literature to propose targeted therapies, clinical trials, or combination regimens.
- Prognostic and predictive modeling: AI can integrate clinical, imaging, and molecular data to predict treatment response, survival, or risk of recurrence.
For trainees in oncology and genetics clinics, this often appears as:
- Decision-support reports attached to genomic test results
- AI-curated literature summaries linking specific mutations to drugs or trials
- Risk calculators incorporating genetic and clinical features
AI in Drug Discovery and Therapeutic Optimization
Traditional drug development is expensive and slow. AI is streamlining multiple steps:
- Target identification: Mining biological and clinical datasets to identify novel therapeutic targets
- Molecular design: Generative models propose new compounds with desired properties, narrowing candidates for lab testing
- Drug repurposing: Identifying existing drugs that may work for new indications based on mechanistic or phenotypic data
- Trial design and patient selection: Predicting which patients are most likely to benefit (or experience toxicity), leading to more efficient, targeted trials
In clinical practice, AI can also personalize treatment regimens:
- Dose optimization: Adjusting doses based on patient-specific pharmacokinetic and pharmacodynamic predictions
- Polypharmacy management: Detecting high-risk drug–drug interactions and suggesting safer alternatives
This convergence of AI and Personalized Medicine is particularly relevant in oncology, cardiology, and rare disease, with growing relevance in nearly every specialty as data availability expands.
Elevating Clinical Decision-Making and Reducing Cognitive Load
Clinicians are inundated with data: labs, imaging, consult notes, guidelines, and patient-generated information. AI-powered systems can help transform this deluge into meaningful, context-specific guidance.
Clinical Decision Support Systems (CDSS) Enhanced by AI
Modern CDSS goes beyond static alerts and guideline reminders:
- Context-aware recommendations: EHR-integrated AI models that propose diagnostic tests or treatments based on the specific patient’s presentation, comorbidities, and prior responses.
- Evidence synthesis: Systems that automatically surface the most recent, high-quality evidence applicable to the current patient scenario, potentially including guideline updates or key trials.
- Care pathways: AI-assisted pathways embedded in order sets, dynamically adapted based on lab results and clinical response.
Common platforms such as Epic and Cerner are increasingly embedding these capabilities, often behind the scenes. For residents:
- You may see AI-generated “best next test” prompts or medication suggestions
- You might receive risk scores or guideline-based recommendations pre-populated in notes or order panels
- Your interaction with AI tools will shape how they evolve—including which alerts are overridden, which suggestions are accepted, and how pathways are refined
Reducing Administrative Burden with Automation and NLP
Administrative tasks contribute significantly to clinician burnout. AI offers practical relief:
- Automated documentation: NLP systems can convert clinician–patient conversations into structured notes, problem lists, and billing codes for clinician review.
- Coding and billing support: Algorithms suggest appropriate CPT and ICD codes, reducing time spent on chart abstraction.
- Inbox triage: Automated prioritization of results and messages, highlighting abnormal labs or high-risk communications.
These tools, when well implemented:
- Free up time for direct patient interaction
- Reduce after-hours “pajama time” documentation
- Help maintain more consistent and complete records
However, clinicians must verify outputs, correct errors, and maintain ultimate responsibility for the chart. Understanding AI’s strengths and failure modes is key to using it safely.
Challenges and Risks: Ethical, Practical, and Educational Considerations
AI’s promise is enormous, but so are its challenges. Responsible adopters—especially residents and early-career clinicians—should be prepared to ask critical questions and advocate for safe, equitable deployment.
Data Privacy, Security, and Ethical Use
AI depends on large amounts of data, raising serious concerns:
- Privacy and confidentiality: Ensuring compliance with HIPAA and other regulations; limiting unnecessary data access; secure storage and transmission
- Data breaches and cyberattacks: Healthcare systems are prime targets; AI-related data pipelines add complexity to security operations
- Secondary use of data: Transparent policies on how patient data is used for model development, commercialization, or cross-institutional research
Ethical deployment requires:
- Clear patient communication and, when appropriate, consent regarding AI use
- Governance structures that include clinicians, ethicists, patient representatives, and data scientists
- Mechanisms for auditing and challenging AI-driven decisions
Bias, Fairness, and Health Equity
AI models can perpetuate or deepen existing inequities if trained on biased data:
- Underrepresentation of certain racial, ethnic, or socioeconomic groups can lead to poorer performance for those populations.
- Historic disparities embedded in healthcare utilization data (e.g., lower spending on certain groups) can mislead algorithms that equate cost with need.
Clinicians should:
- Ask whether AI tools have been validated in populations similar to their patients
- Monitor for disparities in performance or outcomes across subgroups
- Advocate for diverse, representative training data and transparent model performance reporting
Integration with Legacy Systems and Clinician Training
Practical hurdles include:
- Technical integration: Many hospitals still rely on fragmented, legacy systems. Seamlessly inserting AI into these environments is non-trivial.
- Usability and workflow alignment: Poorly designed interfaces or excessive alerts can reduce adoption and even harm care.
- Education and digital literacy: Clinicians require training not to become data scientists, but to understand concepts like sensitivity/specificity, calibration, and model limitations.
For residency programs and medical schools, this means:
- Incorporating basic AI literacy, data science concepts, and digital professionalism into curricula
- Teaching how to critically appraise AI tools similarly to how we appraise clinical trials
- Encouraging participation in quality improvement projects that involve AI-driven workflows

The Future of AI in Healthcare: What Trainees Should Expect
Looking ahead, AI will be increasingly embedded in the fabric of everyday care. For medical students and residents, this will shape training, assessment, and practice patterns.
Decentralized and Connected Care
AI, combined with telemedicine and wearable technology, is pushing care beyond the hospital walls:
- Remote monitoring: Wearables and home sensors sending continuous data (e.g., heart rate, oxygen saturation, glucose) to AI systems that detect early signs of decompensation.
- Home-based acute care: “Hospital at home” models supported by AI-guided protocols and virtual rounds.
- Rural and underserved settings: AI-enabled diagnostic tools (e.g., smartphone ophthalmoscopy or ultrasound with AI guidance) supporting clinicians where subspecialty expertise is scarce.
For trainees, this could mean:
- Participating in virtual multidisciplinary rounds for remote patients
- Interpreting AI-generated summaries from home monitoring devices
- Gaining exposure to hybrid care models that blend in-person and digital care
Evolving Role of AI Symptom Checkers and Patient-Facing Tools
Consumer-facing tools will keep growing more sophisticated:
- Symptom checkers that provide triage advice and possible diagnoses
- AI health coaches that deliver behavior change interventions for lifestyle diseases
- Patient portals that provide AI-generated explanations of lab results and imaging reports
Clinicians will need to:
- Understand what patients may have encountered online before seeing you
- Correct misinformation while acknowledging when tools provided helpful guidance
- Collaborate with, rather than compete against, reputable digital health tools
Continuous Education and Lifelong Learning in AI
AI itself is evolving rapidly. To remain current:
- Expect CME and faculty development programs on AI, data literacy, and digital health
- Engage with institutional AI committees or digital innovation groups
- Consider elective rotations or research within informatics, data science, or quality improvement teams
Ultimately, the most effective clinicians will be those who can:
- Integrate AI outputs with nuanced clinical judgment
- Maintain empathy and human connection at the center of care
- Advocate for responsible, equitable Healthcare Innovation that truly benefits patients
FAQ: AI in Healthcare for Clinicians and Trainees
1. What exactly is Artificial Intelligence in healthcare?
Artificial Intelligence in healthcare refers to computational methods that mimic aspects of human cognition—such as learning, pattern recognition, and decision-making—to support clinical and operational tasks. This includes:
- Machine learning models that predict risk or classify disease
- Deep learning for image, signal, and text analysis
- Natural language processing (NLP) that interprets clinical notes or patient messages
- Rule-based and hybrid decision support tools integrated into EHRs
The goal is not to replace clinicians, but to augment their capabilities and improve quality, safety, and efficiency.
2. How does AI improve Diagnostic Accuracy in everyday practice?
AI enhances Diagnostic Accuracy by:
- Detecting subtle patterns on imaging (e.g., small lung nodules, early ischemia) that may be difficult for the human eye, especially under time pressure
- Continuously scanning EHR data to flag evolving risk of conditions like sepsis or acute kidney injury
- Offering a consistent “second read” that reduces variability between clinicians
Importantly, clinicians remain responsible for confirming findings, interpreting them in context, and making final decisions. AI suggestions should always be weighed alongside clinical history, exam findings, and patient preferences.
3. Is AI safe for patient data and privacy?
AI can be used safely with patient data provided that:
- Data are stored and transmitted securely, following regulations like HIPAA
- Access is restricted to authorized users and clearly logged
- De-identification or anonymization is applied when appropriate for research or model development
- Institutions maintain robust cybersecurity and incident response plans
Clinicians can advocate for transparent policies on how patient data are used and ask how vendors handle data privacy, model training, and potential commercialization.
4. Will AI replace doctors or other healthcare professionals?
AI is unlikely to replace clinicians, especially in the foreseeable future. Instead, it will:
- Automate specific tasks (e.g., screening, documentation, image pre-reading)
- Change the mix of skills and competencies needed
- Elevate the importance of human strengths such as clinical reasoning in complex, ambiguous cases; communication; empathy; and ethical judgment
The clinicians who thrive will be those who learn to collaborate effectively with AI tools—understanding their capabilities, limitations, and appropriate use cases.
5. How can medical students and residents prepare for an AI-enabled future?
Practical steps include:
- Building foundational literacy in statistics, evidence-based medicine, and basic AI/ML concepts (e.g., sensitivity, specificity, calibration, bias)
- Asking critical questions about AI tools you encounter: How were they validated? In what populations? What are their error modes?
- Participating in quality improvement or informatics projects involving EHR optimization, clinical decision support, or digital health interventions
- Staying engaged with professional societies, which increasingly offer resources and guidelines on AI in your specialty
By engaging thoughtfully with AI and Personalized Medicine, you can help shape a future where Healthcare Innovation genuinely improves patient outcomes and preserves the humanity at the heart of medicine.


















