The pass/fail change to Step 1 did not relax the game. It just moved the target.
If you are in the six months after Step 1, you are in a brutally important window that most students waste. They drift. They “recover.” Meanwhile your future residency program is being decided quietly by your habits right now.
I am going to walk you month by month, then zoom down to week-by-week priorities, through this six‑month window:
- You just passed Step 1 (or soon will).
- Step 2 is now king.
- Clerkship grades are no longer “nice to have.” They are currency.
- Research, mentorship, and letters either start now or you pay for it later.
Use this like an operations manual: “At this point you should…” and then do the thing.
Big Picture: What the 6-Month Window Actually Controls
At this point you should understand what is on the line. Not vibes. Not “general career development.” Concrete levers:
| Lever | Impact on Match Competitiveness |
|---|---|
| Step 2 CK score | Very High |
| Core clerkship grades | Very High |
| Early research | Medium–High |
| Mentorship & letters | High |
| Study & work habits | Long-term High |
Program directors are already shifting weight from Step 1 to Step 2 CK and clinical performance.

| Category | Value |
|---|---|
| Step 1 | 20 |
| Step 2 CK | 90 |
| Clerkships | 80 |
| Letters | 70 |
| Research | 50 |
Those numbers are obviously approximate, but the pattern is real. You passed Step 1. Good. The scoreboard just reset.
Now we build the next six months.
Month 0: The Week You Get Your Step 1 Result
At this point you should resist the urge to completely shut your brain off for a month.
Week 0 (Result Week)
48 hours: decompress on purpose, not by accident.
- Take 1–2 days off: sleep in, see actual humans, move your body.
- Hard stop: after 48 hours, you are back on a loose plan.
Day 3–4: Post‑mortem while it is fresh.
- Write down:
- What study strategies actually worked.
- Where you were weakest conceptually.
- What burned you out.
- You will reuse this when planning Step 2. Do not rely on memory later; you will overestimate how well you “studied.”
- Write down:
Day 5–7: Reconnect with the real curriculum.
- If you are between pre‑clinicals and clerkships:
- Skim the upcoming block or clerkship handbook.
- Re‑orient from multiple‑choice tunnel vision back to patients and systems.
- If you are already on a rotation:
- Identify 1–2 specific patient problems where your Step 1 knowledge is shaky (electrolytes, ABGs, endocrine). Start tightening these.
- If you are between pre‑clinicals and clerkships:
Checklist – Week 0
- Celebrate 1–2 days, then stop.
- Write a one‑page Step 1 “lessons learned” document.
- Open your school’s clerkship expectations document.
- Email your academic advisor to schedule a planning meeting for Month 1.
Month 1: Reset and Re-Anchor to Clinical Reality
This month you should rebuild your foundation: schedule, identity, and goals.
At this point you should:
Define your next 12–18 month goals on one sheet of paper.
- Not fifty items. Four buckets:
- Step 2 CK target (yes, pick a number range).
- Clinical goals: “Honors in at least X core clerkships.”
- Scholarly goals: “1 poster or paper in [specialty] by ERAS season.”
- Professional network: “2 strong faculty mentors + 2 residents who know me well.”
- Not fifty items. Four buckets:
Meet with someone who has already played this game.
- Academic advisor, recent graduate, resident in a field you are considering.
- You bring:
- Your one‑sheet goals.
- Your Step 1 reflections.
- Ask directly:
- “Given Step 1 is pass/fail now, how heavily did programs in your specialty use Step 2 and clerkship grades?”
- “What would you do differently in the six months after Step 1 if you could redo it?”
Choose your “academic identity” for now.
- You do not need to lock in a specialty, but you need a direction.
- Examples:
- “Leaning IM / cards.”
- “Probably EM vs anesthesia.”
- “Broadly surgical, not sure which.”
- Your direction will guide:
- Which attendings to impress.
- Which research projects to say yes/no to.
- Which rotations you treat as “auditions.”
Audit your life logistics.
- Time-wasters you allowed during Step 1 “break” that will destroy your clerkship performance.
- Commute, sleep, exercise, meals. Boring but decisive.
- You are moving from “self‑paced study” to “externally scheduled clinical life.” You need structure.
Week-by-Week – Month 1
- Week 1: Goals + advisor meeting + rough Step 2 timing.
- Week 2: Read through clerkship syllabi, grading rubrics, and shelf exam weights.
- Week 3: Build a template weekly schedule for a heavy rotation (IM or surgery style).
- Week 4: Start light Step 2 exposure: 10–15 mixed clinical vignettes/day just to keep the test‑taking muscle alive.
Months 2–3: Early Clerkships + Strategic Reputation Building
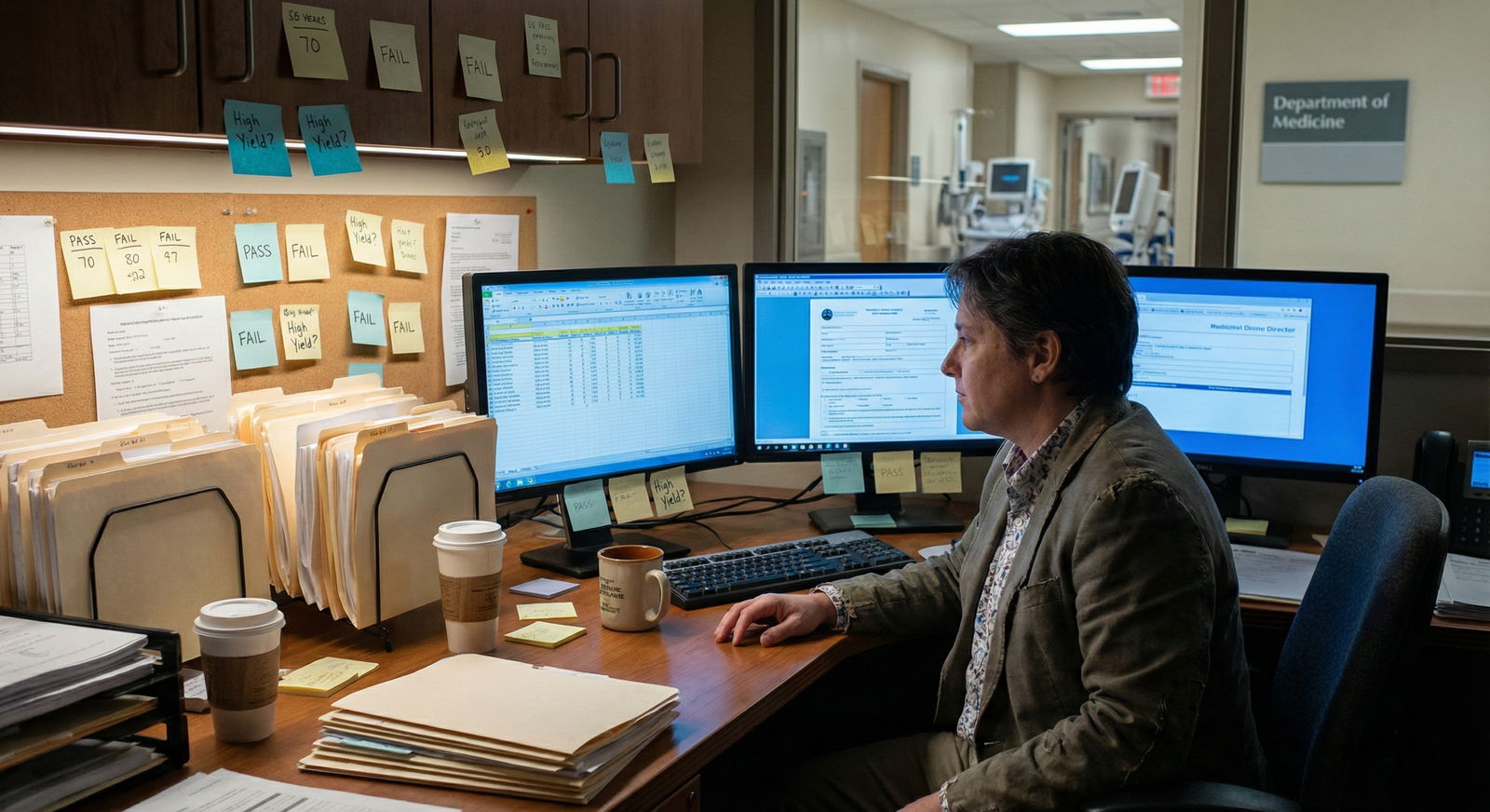
These two months usually land right at the start of your core clerkships. This is where most students drift because they “just want to survive.” That is how you end up with vague “Pass” comments in your MSPE.
At this point you should behave like someone who expects to be written about positively in detail.
Month 2: First Full Clerkship
Focus: Learning the game of clinical performance while keeping one eye on Step 2 and future letters.
Week 1 of the rotation
- Show up obviously over‑prepared for:
- Note structure.
- Presentation format.
- Common diagnoses in that service.
- Script you use with your attending or senior:
- “I am early in my rotations and want to build strong clinical habits. Can you tell me what separates an Honors student from a typical student on this rotation?”
You will hear the same themes over and over:
- Reliability.
- Ownership.
- Reading about your own patients.
- Not being a black hole of work.
Good. Then do those.
Week 2–3
Daily minimums:
- 1–2 patients you “own” and know deeply.
- 15–20 UWorld (or AMBOSS) questions tied to your current rotation subject.
- 10 minutes end-of-day to jot down:
- One thing you learned.
- One way you could have been more helpful.
- One concept to look up.
Week 4 (midpoint-ish)
- Ask for explicit feedback:
- “What do I need to do in the next two weeks to be in the Honors range?”
- Adjust immediately. I have watched students get saved from an average eval because they forced this conversation and then visibly improved.
Month 3: Sharpening Clinical + First Research Moves
You are no longer “brand new” on the wards. At this point you should start blending clinical performance with future‑facing moves.
Clinical
- Aim for:
- 20–30 high‑quality questions/day on weekdays.
- One half‑day each weekend for dedicated shelf prep.
- Rotate‑specific:
- For IM: acid‑base, heart failure, COPD, diabetes.
- For surgery: peri‑op management, fluids, basic trauma/ACS.
- For OB/GYN, peds, psych: memorize the algorithms; they are heavily tested.
Research
You do not wait until “after clerkships” to begin. That is how you end up panicking before ERAS.
At this point you should:
- Identify 1–2 faculty in your tentative specialty direction.
- Strategy: Look at your institution’s last 3–5 publications in that field.
- Send a short, targeted email:
- 3–4 sentences, including:
- Who you are.
- Your level (MS2 starting clerkships, for example).
- Your general interests.
- A specific ask: “Do you have any resident‑led or chart‑review projects where you could use a motivated student for data collection or literature review?”
- 3–4 sentences, including:
Keep your ego out of it. You are not too good for “data monkey” work. Those projects finish. Finished projects turn into bullets on your CV.
Month 2–3 Checklist
- Have asked at least one attending, “What does Honors require here?”
- Doing 20–30 focused questions per day tied to current rotation.
- Have emailed at least 2 potential research mentors.
- Tracking daily clinical learning in a tiny notebook or notes app.
Months 4–5: Step 2 Positioning + Real Production
By now you have some clinical mileage and maybe a project or two in motion. This is where most people either:
- Level up and separate from the pack.
- Or exhaust themselves with chaos and no plan.
At this point you should start thinking about Step 2 timing and score, without derailing your current clerkship.
Step 2 CK Planning

| Category | Value |
|---|---|
| Now | 10 |
| 2 mo out | 25 |
| 1 mo out | 40 |
| Exam | 0 |
That “values” row is roughly questions/day if you are studying consistently.
Decide on:
- A rough exam window (for many: end of core clerkships or during an easier rotation).
- A minimal baseline:
- 10–15 mixed Step 2‑style questions/day starting now.
- Gradually increase to 30–40/day closer to the exam.
Clerkship + Step 2 integration
- Do not “switch off” rotation‑specific prep yet. But the closer you get to your Step 2 date, the more you bias your questions to:
- Mixed, multi‑system sets.
- Time‑pressured blocks (40 q in 1 hour minimum).
Research and CV Output
Month 4–5 is where a lot of projects die quietly. At this point you should force your projects to move or be cut.
For each project you are on, ask:
- Is there a clear product? (Case report, abstract, paper, QI poster.)
- Is there a timeline? (Submission deadline, conference date.)
- Is someone clearly in charge? (Resident, fellow, PI who answers emails.)
If the answer is “no” to all three, you either:
- Push to create clarity. (“Can we target X conference in Month Y?”)
- Or gracefully deprioritize and put your time elsewhere.
Aim for by the end of Month 5:
- 1 thing submitted (case, abstract, or poster) or
- 1 project with clear data collection completed.
Month 6: Consolidation and Launch
You are now at the end of the six‑month window. This is not the finish line. It is the point where your trajectory is locked in unless you radically change.
At this point you should step back and make a brutally honest audit.
Clinical Performance Audit
List your core rotations so far with three columns:
- Grade (Pass/High Pass/Honors).
- Comments (strongest eval themes).
- Potential letter writers.
| Clerkship | Grade | Letter Potential |
|---|---|---|
| Internal Medicine | High Pass | Strong attending letter |
| Surgery | Pass | No (limited interaction) |
| Pediatrics | Honors | Great resident + attending |
| Psychiatry | In progress | TBD |
If you have:
- No clear letter writers yet: next rotation, you must deliberately pick 1 attending and 1 senior resident to impress and follow.
- Mostly Pass with no narrative strength: you need to change your behavior, not just “try harder.” That usually means:
- More proactive ownership.
- Better communication (“I will do X by Y time”).
- Visible reading about your own patients.
Step 2 Readiness Check
By Month 6, you should have:
- Finished at least 50–60 percent of a main Q‑bank for Step 2.
- Done at least one timed 40‑question block under exam conditions.
- Scheduled a realistic exam window (even if you still may adjust slightly).
If you are far below that, adjust:
- Either:
- Push exam date and commit to consistent daily questions now.
- Or accept that Step 2 will become your primary focus as soon as the heaviest clerkships are done.
Letters and Mentorship
At this point you should lock in at least:
- 1 faculty mentor who knows your work and your goals.
- 1–2 potential letter writers.
You do not have to ask for letters right now, but you should:
- Email or meet them:
- Update them briefly on:
- Your clerkship performance.
- Any research or scholarship activity.
- Your rough specialty leaning.
- Ask:
- “Can I check in with you again in X months as I get closer to residency applications?”
- Update them briefly on:
This keeps the relationship alive without being awkward.
Timeline Snapshot: The Whole 6 Months
Here is what this six‑month arc should look like if you are using it well:

| Period | Event |
|---|---|
| Month 0-1 - Step 1 result & reflection | You pass, debrief, set goals |
| Month 0-1 - First planning meeting | Define Step 2 and clerkship targets |
| Months 2-3 - First core clerkship | Learn evaluation game, aim for Honors |
| Months 2-3 - Start research | Join 1-2 realistic projects |
| Months 4-5 - Step 2 baseline work | Daily mixed questions, plan exam window |
| Months 4-5 - Research output | Abstract/case or clear progress |
| Month 6 - Performance audit | Review grades, letters, progress |
| Month 6 - Lock next phase | Firm Step 2 date, mentor ties |
Micro-Level: A “Good” Week During This Window
At this point you should have a default weekly pattern, especially on full‑time clerkships. Example for an IM rotation during Months 2–5:
Weekday
- 6:00–6:30 – Wake, quick review of 5–10 flashcards or one short topic.
- 7:00–5:00 – Wards/OR/clinic. You are present, reliable, and writing good notes.
- 5:30–6:00 – Decompress, food.
- 6:00–7:00 – 20–30 rotation‑specific or Step 2 questions, review explanations focusing on patterns.
- 7:00–7:15 – Write down:
- 1–2 “pearls” from the day.
- 1 thing to improve tomorrow.
Two evenings per week:
- 30–45 minutes extra to push a research task forward (data extraction, drafting an intro, revising a figure).
Weekend
- Half‑day (3–4 hours) of deeper shelf/Step 2 work:
- Longer question blocks.
- Reviewing high‑yield material for that rotation.
- 1–2 hours total for research tasks.
- The rest: life. If you erase your life, you will burn out before Step 2.
You can adjust times, but the structure should exist. If your week has no default pattern, you will get whatever the rotation throws at you and nothing more.
What You Should Stop Doing in This Window
I will be blunt. There are a few things that are simply bad moves in this six‑month window.
At this point you should not:
- Float specialty‑less through clerkships “waiting to see what clicks” without at least narrowing to 2–3 directions.
- Say yes to every random project with no clear product, then brag about being on “five research teams” while none of them ever submit.
- Treat Step 2 as “future me’s problem” because Step 1 is now P/F. Programs have already moved on. You should too.
- Hide from feedback. Mid‑rotation feedback—even if painful—lets you salvage a grade. End‑of‑rotation feedback is just autopsy.
Key Takeaways
- The six months after Step 1 in the pass/fail era are not downtime; they are when you set the trajectory for Step 2, clerkship performance, and early scholarly output.
- At each stage—Month 1 planning, Months 2–3 early clerkships, Months 4–5 Step 2 positioning, Month 6 audit—you should have specific, concrete behaviors: questions per day, feedback conversations, research steps, and mentor contacts.
- If you exit this window with a clear Step 2 plan, at least one strong potential letter writer, and visible progress on at least one scholarly project, you have used the P/F transition correctly. If not, adjust now. The system will not slow down for you.
















