
Introduction: Why Reviewing After USMLE Step 3 Still Matters
Finishing the USMLE Step 3 often feels like crossing the final major examination hurdle on your way toward independent clinical practice. You’ve survived pre-clinicals, clinical rotations, Step 1, Step 2 CK, and now the last exam in the USMLE sequence. It is tempting to close that chapter and never look back.
Yet, what you do after you take Step 3 can significantly influence your development as a clinician.
Step 3 sits at the intersection of Medical Education and real-world practice. It tests your ability to integrate clinical knowledge, decision-making, and patient management in a way that mirrors residency and beyond. A thoughtful, structured post-exam exam review can:
- Cement what you did well
- Clarify where your reasoning broke down
- Translate exam experience into better patient care
- Prepare you for in-training exams, board certification, and lifelong learning
This guide walks you through how to effectively review after taking USMLE Step 3, using your experience not just to “post-mortem” an exam, but to upgrade your clinical thinking for the rest of your career.
Understanding the Purpose of Post–Step 3 Review
Beyond the Score: Why Reflection Is Part of Clinical Training
Post-exam review is not just about dissecting a score report. It’s an extension of how you’ll practice medicine: observe, interpret, improve. For residency applicants and junior residents, learning to self-assess after high-stakes events (like Step 3) sets the foundation for reflective practice.
Reviewing your Step 3 experience serves several key purposes:
Identifying Strengths and Weaknesses
Your Step 3 performance is a snapshot of your current clinical reasoning, knowledge base, and test-taking skills. Reviewing it methodically helps you recognize:- Strong domains (e.g., acute management, pediatrics, preventive care)
- Vulnerable areas (e.g., biostatistics, chronic disease management, OB, ethics)
Enhancing Clinical Knowledge and Application
Step 3 is less about isolated facts and more about clinical decision-making. A deliberate review helps you:- Reinforce guidelines, algorithms, and standard of care
- Correct misconceptions before they show up in front of real patients
- Better integrate basic science with bedside reasoning
Turning Feedback into Future Performance Gains
Whether your score is above or below your expectations, it provides actionable feedback. When interpreted correctly, it can:- Guide your early residency reading
- Shape how you use downtime on rotations
- Prioritize which skills to develop (e.g., time management, CCS pacing)
Building Resilience and Professional Maturity
Processing the exam—emotionally and intellectually—helps you:- Recover from anxiety or disappointment
- Normalize setbacks as part of growth in medical education
- Develop a mindset of continuous improvement that will serve you through residency and board exams
Step 1: Gather and Organize Your Review Resources
Before you analyze anything, assemble your tools. A disorganized review feels overwhelming and is easy to abandon. A structured approach makes it efficient and sustainable.
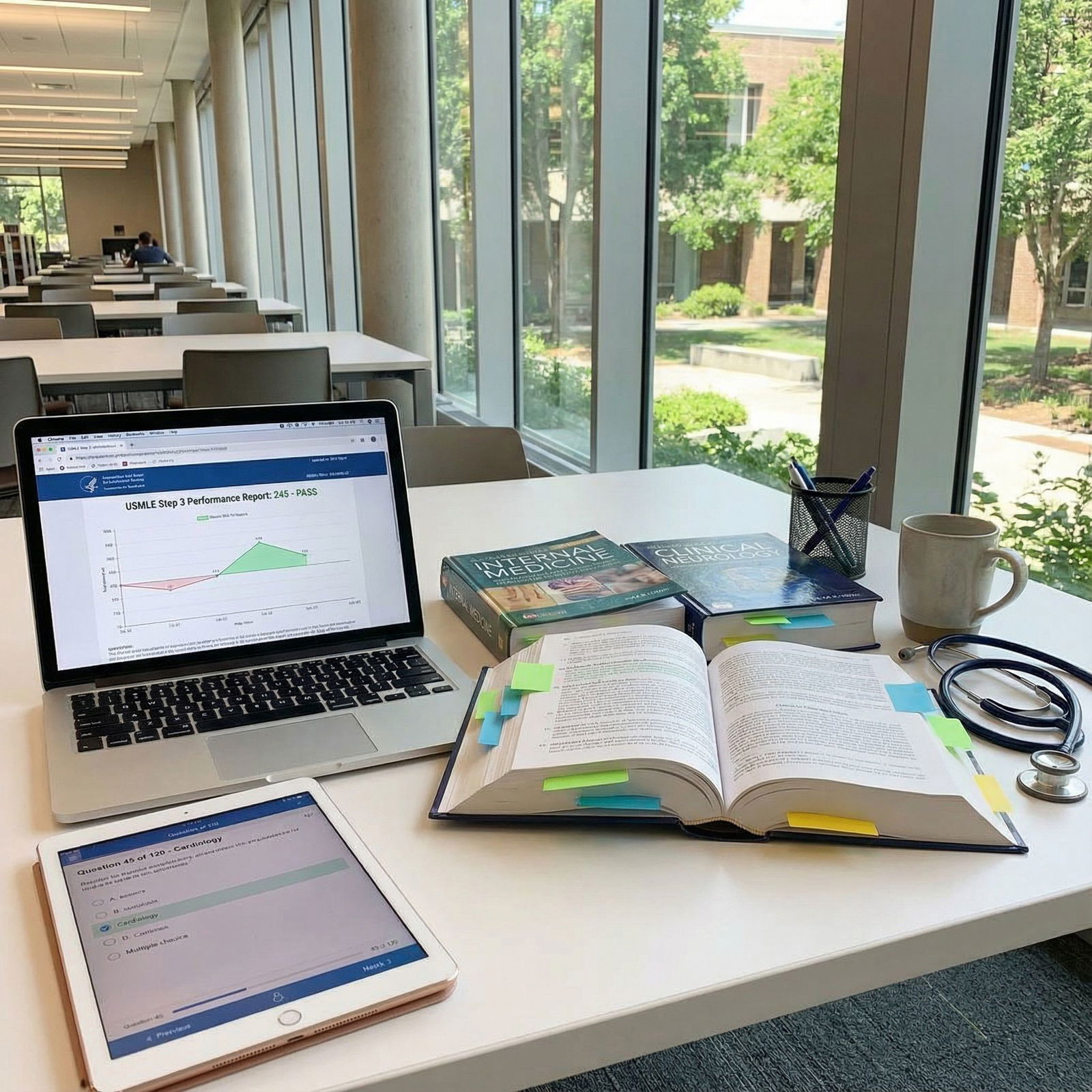
Key Resources to Collect
Official Score Report
- Review both your overall score and the breakdown across content and competency domains.
- Look for:
- Relative strengths (e.g., “above average” in internal medicine)
- Relative weaknesses (e.g., “below average” in epidemiology/biostatistics, CCS cases, or specific systems)
Practice Question Data
- From question banks (e.g., UWorld, Amboss, others used for Step 3).
- Focus on:
- Question blocks or subjects where your percentage was consistently low
- Common error patterns (e.g., always missing management questions, or questions with long stems)
Textbooks and Core Online References
- Internal medicine, pediatrics, OB/Gyn, psychiatry references you trust.
- Gold-standard resources:
- UWorld Step 3 explanations (for post-hoc review)
- UpToDate or similar platforms for current guidelines
- First Aid (or equivalent) for high-yield summaries
Personal Notes and Anki Decks (if used)
- Tag or mark Step 3-specific cards or notes where you felt shaky.
- Flag topics related to any content areas you recall struggling with on test day.
Peer and Mentor Input
- Co-residents, attendings, or co-applicants who recently took Step 3.
- Study partners who may offer alternative approaches or resources you missed.
Setting Up a Simple Review System
- Create a Step 3 Review Folder (digital or physical).
- Include:
- PDF of your score report
- A spreadsheet or document with:
- “Strong Topics”
- “Weak Topics”
- “Process/Strategy Issues”
- Links or references to your primary learning resources
Step 2: Analyze Your Performance Thoughtfully
Once your materials are organized, it’s time for a structured performance analysis. Avoid broad judgments like “I’m just bad at OB.” Instead, aim for specific, actionable insights.
2.1 Interpreting Your Score Report
Break your report into:
- Content Areas (e.g., internal medicine, surgery, pediatrics, OB/Gyn, psychiatry, preventive medicine, epidemiology/biostatistics)
- Competencies (e.g., diagnostic reasoning, management, patient safety, CCS performance)
For each area, ask:
- Was this consistent with my Step 2 CK performance and clinical rotations?
- Did my practice question percentages predict this, or was it a surprise?
- Are weaknesses due to:
- Knowledge gaps?
- Poor test-taking strategy?
- Time management errors?
- Anxiety or fatigue during the exam?
2.2 Reflecting on Test-Day Experience
While you cannot recall or review specific exam items, you can reflect on patterns:
Time Management
- Did you finish with comfortable time buffers?
- Did you rush through early questions or run out of time at the end?
- In CCS, did you:
- Advance time appropriately?
- Order necessary tests promptly?
- Forget key monitoring or counseling steps?
Question Approach
- Did you read answer choices before the stem?
- Were you frequently torn between two options?
- Did you change a lot of answers, and did that help or hurt you in prior practice?
Content Confidence
- Which types of patients felt most stressful? (e.g., obstetric emergencies, pediatric rashes, post-op complications)
- Were biostatistics or ethics questions sources of panic?
Document this in a brief reflection document (1–2 pages). This becomes your roadmap.
Step 3: Designing a Targeted Post–Step 3 Study Plan
Your goal is no longer just “pass Step 3.” After the exam, your study strategies should focus on building durable skills for residency and beyond.
3.1 Clarify Your Objectives
Depending on your situation, your goals may differ:
As a residency applicant or incoming intern:
- Strengthen core clinical knowledge in areas relevant to your intended specialty.
- Prepare for early rotations (e.g., IM, surgery, pediatrics, OB) where foundational knowledge is critical.
- Build confidence in managing common conditions safely and efficiently.
As a current resident:
- Align your review with in-training exam content.
- Focus on topics frequently encountered on your current or upcoming rotations.
- Sharpen clinical decision-making and guideline-based care.
3.2 Building Your Plan: Structure and Timeline
Time Frame
- Plan a 4–12 week review period, depending on your schedule and intensity.
- Even 2–3 hours per week can make a difference if consistently applied.
Weekly Structure A sample weekly framework:
- 1–2 focused content sessions (60–90 minutes each)
- Deep dive into one weak content area (e.g., OB hemorrhage, diabetes management).
- 1 question-based session
- 20–40 timed, mixed questions with post-review.
- 1 CCS-focused session (if still early in training)
- Run through 1–2 simulated cases, critique your steps.
- 1–2 focused content sessions (60–90 minutes each)
Prioritize High-Yield Systems and Skills Especially for Step 3–style thinking and residency preparation:
- Internal medicine (cardiology, pulmonology, infectious disease, nephrology)
- OB/Gyn (pregnancy emergencies, prenatal care, postpartum complications)
- Pediatrics (vaccination schedules, common infections, growth and development)
- Psychiatry (acute agitation, depression, substance use, suicidality)
- Preventive care and screening (USPSTF-style thinking)
- Biostatistics and epidemiology (test interpretation, study design, bias)
3.3 Active Learning Techniques
Use active methods rather than passive reading:
Teach-Back Method
- Explain a topic to a peer, junior student, or even to yourself out loud.
- If you can’t explain it simply and logically, you haven’t mastered it.
Error Log
- Maintain a running list of:
- Questions you missed in practice
- Why you missed them (knowledge, misreading, overthinking, fatigue)
- The corrected takeaway in 1–2 sentences
- Review this log weekly.
- Maintain a running list of:
One-Pager Summaries
- For each core topic (e.g., diabetic ketoacidosis, preeclampsia), create:
- Key diagnostic criteria
- First-line management
- Red flags and “never miss” considerations
- For each core topic (e.g., diabetic ketoacidosis, preeclampsia), create:
Step 4: Using Clinical Cases to Solidify Step 3 Concepts
Step 3 is case-based for a reason: it mirrors how you’ll function on the wards and in clinic.

4.1 Case Studies and Scenarios
Use your question banks’ tutor mode to:
- Walk slowly through long stems.
- Identify key clues and “red flag” phrases.
- Practice building a mental differential diagnosis and stepwise plan.
Supplement with:
- Case-based texts or apps that present a symptom and guide you through:
- Differential
- Diagnostic workup
- Management, including follow-up and counseling
- Case-based texts or apps that present a symptom and guide you through:
4.2 Practicing CCS-Style Thinking (Even After the Exam)
Even if you will never sit for another CCS, the structure is educational:
- For each case you see (real or simulated), ask:
- What are the immediate life-threatening issues?
- Which diagnostics need to be ordered now vs. later?
- What consults or ancillary services would I involve?
- What patient counseling is essential?
You can occasionally run through:
- Online CCS practice cases (if still available in your account)
- Self-made “CCS scripts”:
- Write out your orders for a classic case (e.g., chest pain, seizure, GI bleed).
This trains the habit of organized, protocol-based care, highly valued in residency.
Step 5: Seek Constructive Feedback and Support
Self-directed review can only go so far. External feedback refines your perspective and prevents blind spots.
5.1 Mentors and Faculty
Schedule brief conversations with:
- Program leadership (if you’re a resident) or advisors (if you’re an applicant)
- Faculty in areas you identified as weak (e.g., OB attendings if OB/Gyn was low)
During these sessions:
- Share a concise summary:
- “My Step 3 report showed below-average performance in epidemiology and OB emergencies. I’d like to strengthen those areas before intern year.”
- Ask targeted questions:
- “What core topics in OB/Gyn do you see interns struggle with the most?”
- “Any go-to resources or guidelines you recommend?”
5.2 Peer and Group Learning
Form or join a small review group (2–4 peers) to:
- Discuss tricky concept areas
- Walk through clinical algorithms
- Quiz each other on high-yield scenarios
Online communities (Reddit, USMLE forums, specialty-specific forums) can:
- Highlight common pitfalls
- Suggest effective resources
- Normalize concerns about Step 3 scores and preparation
5.3 Professional Coaching (If Needed)
If your Step 3 attempt was unsuccessful or far below your expectations:
- Consider a structured plan with:
- A USMLE-focused tutor or coach
- Your institution’s academic support office, if available
- Focus on:
- Diagnostic testing (to understand root causes)
- A targeted remediation plan
- Building sustainable study habits that align with your clinical schedule
Step 6: Ongoing Self-Assessment and Feedback Loops
Improvement in medicine is cyclical: learn → apply → reflect → adjust.
6.1 Regular Question Blocks
Even after Step 3, periodically:
- Do timed, mixed blocks of 10–20 questions:
- Prioritize your weaker systems.
- Use explanations to reinforce correct reasoning, not just facts.
- Track:
- Question performance over time
- Whether previously weak areas are now stabilizing
6.2 Integrating Learning into Clinical Work
As you move through rotations, use real patients as your curriculum:
- After a shift, pick 1–2 patients and:
- Read guideline-based management for their key diagnosis.
- Compare what was done vs. what the literature recommends.
- Convert clinical encounters into enduring knowledge:
- “Every time I see COPD exacerbation, I will review its severity staging and management.”
6.3 Reflective Practice
At regular intervals (monthly or quarterly), ask:
- What aspects of my practice still make me feel uncertain?
- Where do I consistently seek help from seniors?
- Which patient scenarios do I dread?
These are your next “study targets.”
Step 7: Protecting Your Well-Being and Maintaining Perspective
High-stakes exams can take a psychological toll, especially when layered onto clinical responsibilities.
7.1 Managing Emotional Reactions
Your feelings about Step 3—relief, disappointment, pride, frustration—are all valid. Address them so they don’t silently impact your performance or confidence.
- If satisfied with your performance:
- Use that confidence constructively—don’t become complacent.
- If disappointed:
- Separate your score from your worth as a clinician-in-training.
- Recognize:
- Exams sample a limited slice of knowledge.
- Many outstanding physicians have average exam scores.
Consider debriefing with:
- Trusted peers
- A mentor
- Mental health professionals (especially if distress is persistent or severe)
7.2 Supporting Physical Health
- Sleep: Prioritize consistent, adequate sleep. Cognitive performance, memory consolidation, and emotional regulation all depend on it.
- Nutrition and Exercise: Simple, sustainable routines (e.g., 20–30 minutes of activity a few days per week) can significantly boost focus and resilience.
- Boundaries: Structure your review so it fits your life; avoid over-committing to an unrealistic study schedule that leads to burnout.
Step 8: Set Long-Term Learning Goals Beyond Step 3
Step 3 is a milestone, but it’s not the endpoint. Use your experience to shape the next phase of your professional development.
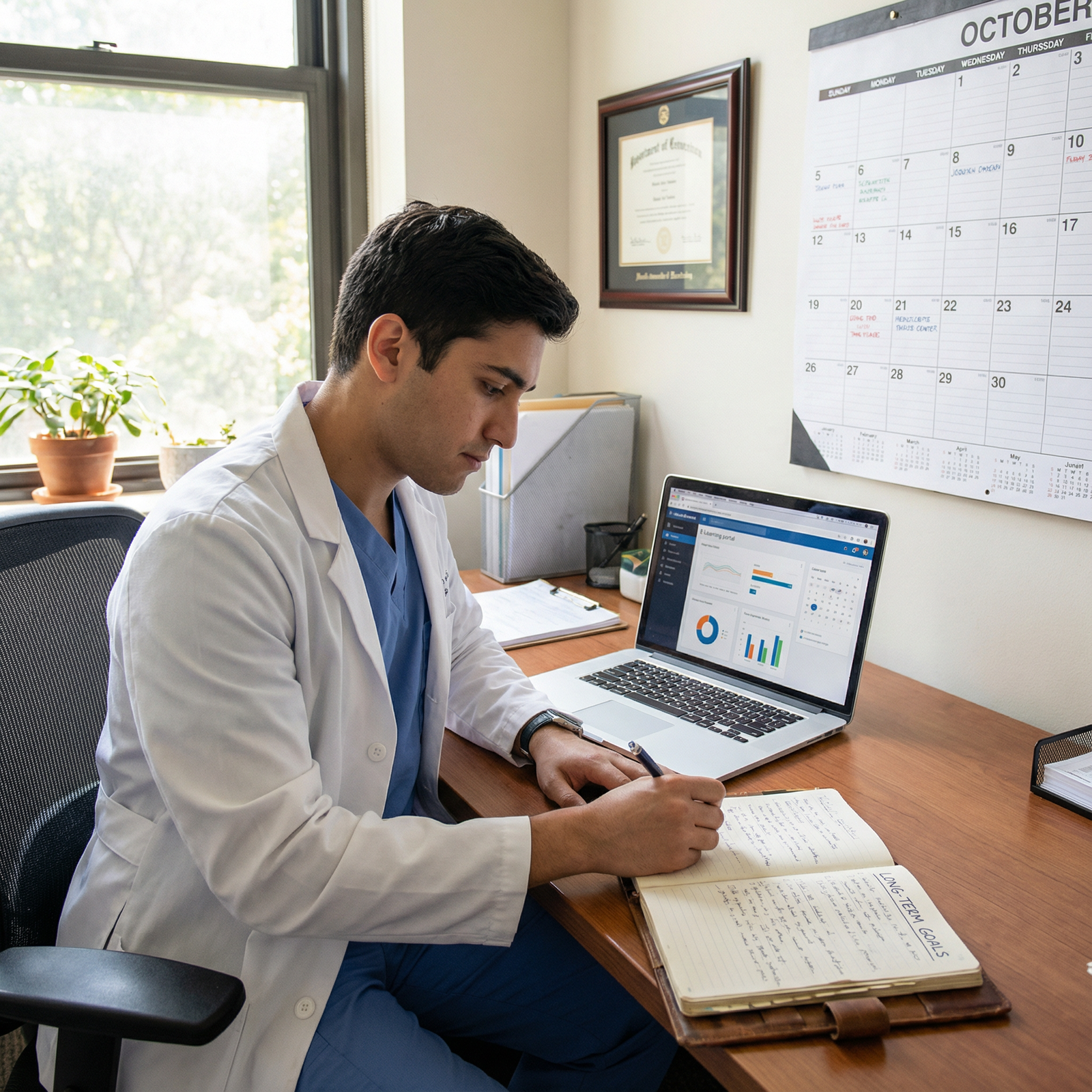
8.1 Aligning with Your Intended Specialty
If you have a clear specialty interest:
- Map your weak areas to what your specialty demands. For example:
- Aspiring internist with weak preventive medicine → focus on chronic disease screening, outpatient guidelines.
- Future OB/Gyn with low OB scores → reinforce pregnancy management algorithms and labor complications.
8.2 Continuing Medical Education (CME) Mindset
Adopt a lifelong learning framework:
- Subscribe to:
- Key journals or summaries (e.g., ACP Journal Club, specialty society updates).
- Use:
- Podcasts or brief online modules that integrate easily into commute or workout time.
- Aim to periodically:
- Revisit fundamental topics
- Update your practice with evolving guidelines
8.3 Research and Academic Growth
If academic medicine or research interests you:
- Use weak Step 3 areas as research inspiration:
- If you struggled with epidemiology or critical appraisal, consider joining a QI project, clinical trial, or outcomes study.
- This allows you to:
- Improve your understanding of study design and statistics.
- Build an academic portfolio that strengthens residency or fellowship applications.
Real-World Example: Learning from Dr. Michael’s Journey
Consider Dr. Michael, a recent graduate who underperformed on the epidemiology/biostatistics component of USMLE Step 3. He passed the exam, but his score report clearly showed this as a relative weakness.
What he did:
Honest Assessment
He acknowledged that he often guessed on interpretation of sensitivity/specificity, likelihood ratios, and study design questions—both in practice and on the actual exam.Targeted Resource Use
Over 8–10 weeks, he:- Revisited UWorld questions tagged for biostatistics and epidemiology.
- Used a concise biostatistics review book and short online videos.
- Created simple summary sheets for:
- Types of bias
- Common study designs
- Interpreting confidence intervals and p-values
Applied Learning Clinically
During residency, he:- Read the methods sections of major articles discussed on rounds.
- Asked seniors and attendings to help dissect study strengths and limitations.
- Joined a small QI project, working directly with a mentor on data interpretation.
Outcome:
- Within months, he felt significantly more confident in:
- Critically appraising articles
- Applying evidence to patient care
- On his specialty in-training exam, his performance in epidemiology and statistics was markedly improved.
- He later became a go-to resource among his peers for understanding complex study designs—proof that an intentional post–Step 3 review can transform a weakness into a professional strength.
FAQs: Reviewing and Learning After USMLE Step 3
1. If I passed Step 3, do I really need to review my performance?
Yes. Passing Step 3 is important, but your post-exam review is about far more than the test:
- It reveals gaps that can affect your clinical performance and confidence.
- It guides what you focus on as you enter or continue residency.
- It helps transform an isolated exam experience into ongoing professional growth.
Even a few structured hours of review can prevent the same weaknesses from resurfacing on in-training exams or in patient care.
2. How soon after getting my score should I start reviewing?
Ideally:
- Take a few days to decompress after receiving your result.
- Within 1–2 weeks, review:
- Your score report
- Your practice question performance patterns
- Your memory of test-day challenges
This timing allows you to still recall how the exam felt, while giving you enough emotional distance to be objective.
3. What are the best resources for post–Step 3 review and ongoing clinical learning?
Commonly effective resources include:
- Question Banks: UWorld Step 3 (and some Step 2 CK questions for foundational topics)
- Online References: UpToDate, clinical guidelines from professional societies, CDC recommendations
- Textbooks: Concise internal medicine, OB/Gyn, pediatrics, and psychiatry references relevant to your specialty
- Biostatistics/Epi Resources: Short focused texts, high-yield review guides, and online video explanations
Choose resources that you can realistically integrate into your schedule, and focus on areas highlighted as weak by your performance analysis.
4. What if I failed Step 3 or my score is much lower than my Step 1/Step 2 CK?
First, know that you’re not alone, and this does not define your long-term potential:
- Conduct a root-cause analysis:
- Content gaps?
- Time management issues?
- Poor test-day conditions (illness, fatigue, life stress)?
- Build a structured remediation plan:
- Seek coaching or academic support if available.
- Prioritize weaker systems and competencies.
- Use a detailed error log and timed practice blocks.
- Communicate constructively:
- If you’re in or entering residency, discuss this with your program leadership or advisor to ensure support and avoid surprises later.
Many clinicians have recovered from a low or failed attempt and gone on to successful careers by using the experience as a catalyst for growth.
5. How can I track whether my post–Step 3 review is actually helping?
Use simple, objective markers:
- Practice Question Performance:
- Track improvement in weaker domains over several weeks.
- Clinical Confidence:
- Note whether common clinical scenarios that used to feel daunting are now more manageable.
- Feedback from Seniors/Attendings:
- Pay attention to comments on your clinical reasoning, presentations, and management plans.
- In-Training Exams or Later Boards:
- Over the long term, performance on these assessments can reflect the cumulative effect of your improved study strategies and clinical learning.
By intentionally reviewing your USMLE Step 3 experience, you transform a single high-stakes exam into a powerful learning opportunity. Instead of letting your score report gather digital dust, use it to sharpen your clinical knowledge, refine your study strategies, and position yourself for success in residency, board exams, and lifelong medical education.






















