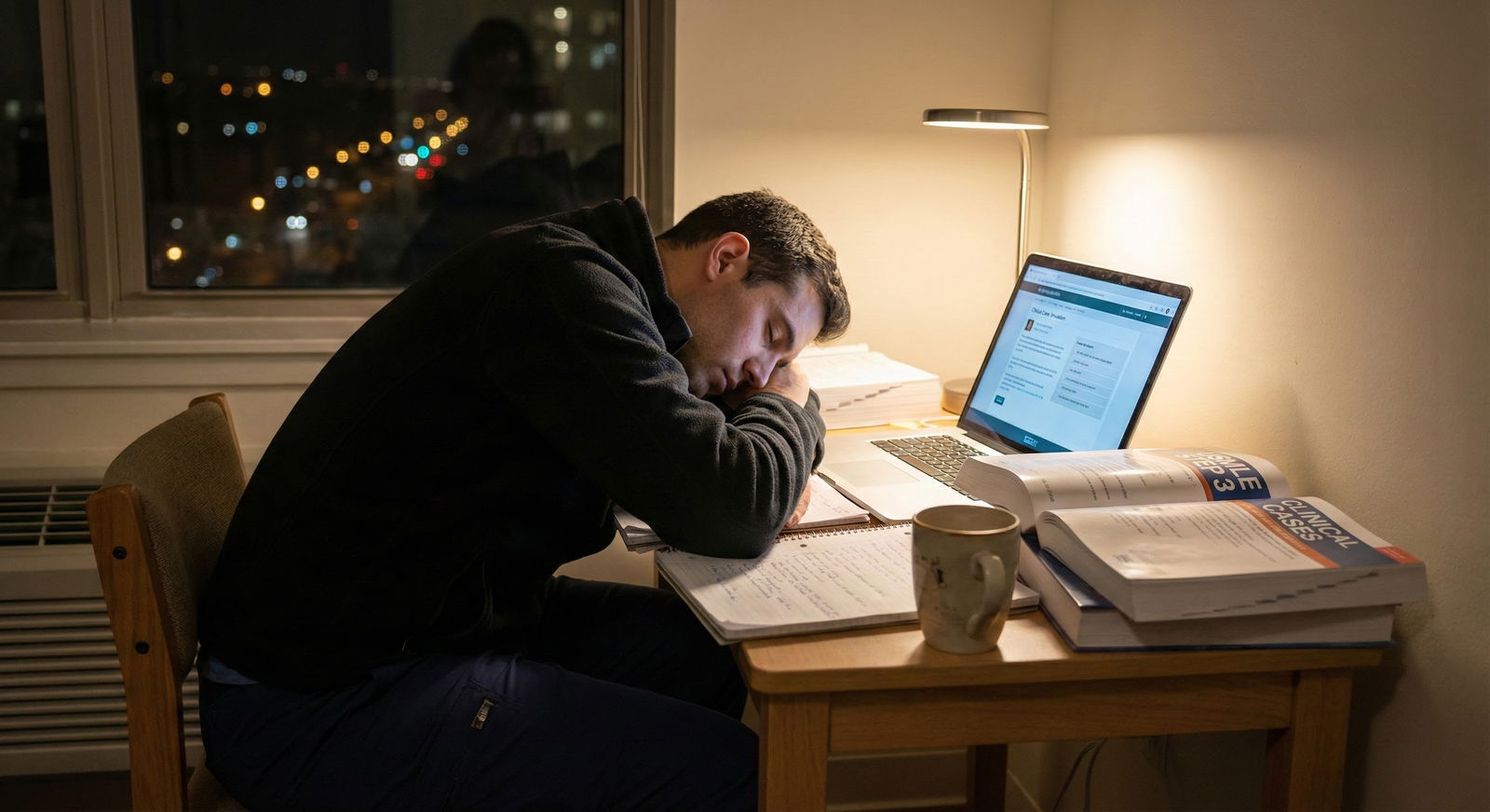
You are post-call, sitting at your kitchen table. Step 3 is in three weeks. Your multiple‑choice practice scores are fine. But every time you open a CCS case, you freeze.
Clock runs. Orders half‑remembered. You forget to reassess vitals. The case ends and you stare at the screen thinking, “I have no idea how that was scored.”
You are not alone. I have watched smart, clinically solid residents underperform on Step 3 purely because of CCS. Not knowledge. Not work ethic. Just no structure and no reps.
The good news: CCS is extremely trainable in a short time. Four focused weeks is plenty to turn it from liability to advantage—if you stop “winging it” and start using a protocol.
Here is exactly how to do that.
Step 1: Understand What CCS Really Tests (And What It Does Not)
Before you start grinding cases, you need to get the target right. CCS does not reward:
- Random shotgun ordering
- Overly subspecialty‑level workups
- One‑size‑fits‑all templates pasted on every case
It does reward:
- Safe, timely stabilization
- Reasonable, guideline‑consistent plans
- Efficiency and appropriate setting (clinic vs ED vs ICU vs floor)
- Reassessment and follow‑up
Think like a competent, cautious PGY‑1 who reads the discharge summary. Not like a fellowship‑bound specialist showing off.
The CCS engine mainly scores:
Initial stabilization / triage
- Did you miss an unstable airway? Hypotension? Chest pain?
- Did you pick the correct setting (ED vs clinic vs ICU vs ward vs home)?
Appropriate, timely diagnostics
- Did you order the right “must‑not‑miss” tests early?
- Did you avoid obviously unnecessary or harmful tests?
Initial treatment and long‑term management
- Immediate therapy: antibiotics, fluids, insulin, anticoagulation, etc.
- Chronic care: lifestyle, screening, vaccinations, counseling, follow‑up visits.
Monitoring and reassessment
- Vitals, exam, labs, imaging reassessments.
- Adjusting management when new data comes in.
Understand this now, because your 4‑week plan is built entirely around drilling these behaviors until they are reflex.
Step 2: Build Your 4‑Week CCS Training Calendar
You need a plan, not vibes.
Here is a concrete 4‑week structure that works. Adjust days to your schedule, but keep the sequence and repetition.
| Week | Focus | Approx CCS Cases |
|---|---|---|
| 1 | Learn interface + basic protocols | 25–30 |
| 2 | Bread-and-butter high-yield cases | 35–40 |
| 3 | Edge cases + speed + errors review | 35–40 |
| 4 | Full exam simulation + polish | 25–30 |
Target total: ~120–140 cases. That is enough to make the system feel boringly familiar—which is exactly what you want on exam day.
Weekly structure
Week 1: Foundation and Interface
Goal: Stop feeling lost in the software. Build 2–3 core “opening moves” you can apply to most cases.
Day 1–2:
- Watch the official NBME/USMLE CCS orientation once.
- Do all the free sample CCS cases from USMLE.
- Do 3–5 cases from your chosen CCS resource without worrying about score; just explore interface.
Day 3–7:
- 4–5 cases per day.
- After each case, write down what you forgot.
- Build a one‑page checklist (more on this in Step 3).
Week 2: High‑Yield Patterns
Goal: Get fast and consistent with common presentations.
Focus categories:
- Chest pain / ACS / PE
- Shortness of breath (asthma, COPD, pneumonia, CHF)
- Abdominal pain (appendicitis, cholecystitis, pancreatitis, SBO)
- Diabetes emergencies, DKA/HHS
- Sepsis, meningitis, pyelonephritis
- Pregnancy: bleeding, preeclampsia, ectopic
Daily:
- 5–6 cases per day.
- One focused review block after cases: look up 1–2 conditions you clearly mishandled.
Week 3: Edge Cases and Efficiency
Goal: Kill your weak spots and tighten time management.
Focus categories:
- Psychiatry (SI, psychosis, alcohol withdrawal)
- Pediatrics (fever workup, bronchiolitis, meningitis, dehydration)
- Preventive and chronic care cases
- ICU/critical care decisions
Daily:
- 5–6 cases per day.
- Identify patterns of mistakes, not just case‑specific errors.
Week 4: Exam Simulation and Final Polish
Goal: Perform under test conditions, not just at home with snacks.
At least two full “CCS blocks”:
- Sit for 6–7 cases in a row with strict time limits.
- Use the same breaks you would use on test day.
Rest of days:
- 3–4 targeted cases hitting anything that still feels shaky.
- Quick review of your own cheat sheets and checklists (Step 3).
Step 3: Use Rigid Protocols, Not Memory, To Run Every Case
You do not want to think from scratch when a case opens. You want a protocol.
Here is the core framework that works for 90% of cases:
Read the stem once—slowly.
- Age, setting (clinic / ED / inpatient), key complaint, vitals.
- Decide: Sick or not sick?
Immediate triage and safety check
- If any of these: chest pain, dyspnea, hypotension, fever + confusion, trauma, pregnancy bleeding, suicidal/homicidal ideation →
- Move patient to ED or ICU if appropriate.
- Order vitals q1h, pulse ox, cardiac monitor, IV access, O2.
- If any of these: chest pain, dyspnea, hypotension, fever + confusion, trauma, pregnancy bleeding, suicidal/homicidal ideation →
Global initial orders (your default startup bundle)
On almost any moderately sick or undifferentiated patient in ED/inpatient, consider:- Vitals Q1–2H
- Pulse oximetry continuous
- Cardiac monitor (if cardiorespiratory concern)
- IV access / saline lock
- Diet: NPO if surgery or unclear abdominal pathology
- Activity: bed rest if unstable
Symptom-specific bundles
Do not reinvent. For 4 weeks, live off simple bundles. For example:
Chest pain bundle (non‑trauma)
- ECG, cardiac enzymes, CXR
- CBC, BMP, PT/INR, PTT, lipid panel, HbA1c
- Aspirin chewed, nitroglycerin (if BP OK, not RV infarct suspicion), O2, morphine (prn severe pain)
- Consider heparin, beta‑blocker, statin, cardiology consult, admission to telemetry/ICU depending on severity.
Fever + hypotension bundle (sepsis)
- IV fluids bolus (NS or LR)
- CBC, CMP, lactate, blood cultures x2, UA/urine culture, CXR
- Broad‑spectrum IV antibiotics ASAP
- Admit to ICU if persistent hypotension / organ dysfunction
DKA bundle
- Fingerstick glucose, BMP, ABG, serum ketones, UA
- IVF resuscitation, insulin drip, potassium management
- ICU or step‑down unit, frequent glucose and electrolyte checks
You can create 6–8 such bundles and tape them to your wall during practice. After a week of using them, you will not need to glance anymore.
Reassess and advance the clock
After initial orders, do not just sit there. Advance time in short steps:
- Advance 30–60 minutes.
- Check new vitals, lab results, notes.
- Adjust therapy (increase O2, treat hyperkalemia, escalate antibiotics, etc.).
Disposition and follow‑up
- Once stable and diagnosis clear, think:
- Ward vs ICU vs home vs OR.
- Arrange follow‑up:
- Clinic visit, repeat labs, imaging, counseling.
- Once stable and diagnosis clear, think:
CCS scores heavily on whether you:
- Recognized urgency early
- Started appropriate initial management
- Reassessed and escalated care as needed
This protocol makes that almost automatic.
Step 4: Build a One‑Page CCS “Command Sheet”
You are allowed scratch paper on test day. Use it like a grown‑up.
During your first week, construct a single, dense page with:
- Top section: Global initial orders checklist
- Middle section: 6–8 symptom‑based bundles
- Bottom section: Preventive care / chronic management essentials
Examples of what should be there:
Global Initial Orders (for most ED/inpatient cases)
- Vitals q1–2h
- Pulse ox continuous
- Cardiac monitor
- IV access / saline lock
- Oxygen by nasal cannula / mask (if needed)
- Fingerstick glucose (if altered, diabetic, or unknown)
- NPO if abdominal pain / surgery concern
- Pregnancy test (all women of reproductive age unless obviously pregnant)
Symptom Bundles (short phrases only)
- Chest pain: ECG, troponin, CXR, ASA, O2, IV, nitro (if ok), morphine, labs
- SOB: CXR, ABG, CBC, BMP, pulse ox, bronchodilators, steroids if asthma/COPD, lasix if CHF suspicion
- Abdominal pain RLQ: CBC, BMP, UA, pregnancy test, abdominal US/CT, NPO, IV fluids, surgical consult
Preventive/Chronic
- DM: HbA1c, microalbumin, statin, ACEI if HTN/proteinuria, eye exam, foot exam
- HTN: BMP, UA, EKG, lifestyle counseling
- Vaccines: flu, pneumococcal, Tdap, zoster based on age/comorbidities
You are not writing a textbook here. You are writing triggers for your brain.
On test day, as soon as the first CCS case starts, quickly rewrite the skeleton of this sheet on your scrap paper in 1–2 minutes. Just the headings and main words. It reduces cognitive load for later cases when you are tired.
Step 5: Drill the Interface Like It Is a Procedure
Most people lose CCS points not from knowledge gaps, but from fighting the software. That is a dumb way to lose points. Fix it.
Spend an entire early session just learning:
- How to move the patient between:
- ED → ward → ICU → home
- How to:
- Advance time in 10‑minute, 30‑minute, hourly, daily increments.
- Change diet and activity.
- Schedule follow‑up visits and labs in the future.
- Enter “as needed” (PRN) meds and nursing orders.

| Category | Value |
|---|---|
| Late stabilization | 30 |
| Wrong setting | 20 |
| Missing key test | 25 |
| No follow-up | 15 |
| Interface confusion | 10 |
You want the interface to feel as boring and automatic as opening Epic or Cerner on day 3 of residency. You are not “figuring it out” on exam day.
Concrete practice drill for interface:
- Take 3–4 low‑stress cases.
- Your only goal:
- Move patient to correct setting.
- Enter global orders.
- Schedule future test + follow‑up appointment.
- Advance time logically.
Ignore score. You are practicing finger‑movements, not medicine.
Step 6: Systematically Fix Your Weakest Patterns
By week 2, you will start noticing the same annoying mistakes over and over. That is where your improvement lives.
Create a “CCS error log”—just a running list on your phone or notebook with three columns:
- Scenario
- What I did wrong
- Correct pattern next time
Examples:
- “Chest pain, forgot aspirin until 2 hours in → Next time: ASA ordered with ECG at minute 0.”
- “Fever + stiff neck, waited for CT before antibiotics → Next time: start IV abx before imaging once meningitis suspected.”
- “Suicidal ideation in clinic, sent home with follow‑up → Next time: ensure psych consult, safety precautions, inpatient admission if needed.”
Every few days, scan this list for themes:
- Do you repeatedly miss triage/setting (clinic vs ED vs ICU)?
- Do you under‑order or over‑order labs/imaging?
- Do you forget reassessments?
Then deliberately assign yourself 2–3 cases only in that weak domain the next day.
You are not trying to get a random 10% better at everything. You are trying to eliminate repeatable, dumb errors.
Step 7: Align CCS With Your Real‑Life Clinical Brain
If you are an intern, you have an advantage: CCS is closer to your real life than you think. The problem is that you often act differently on the exam than on the wards.
When you feel stuck in a case, ask:
“If this patient was in front of me at 3 a.m. at my hospital, what would I actually do next?”
Usually, the answer is straightforward:
- Call rapid response? Start fluids? Get an ECG?
- Move them to ICU? Call surgery? Start antibiotics while waiting?
Then do that in the CCS interface.
Where CCS differs from real practice:
- You need to be more explicit with nursing and monitoring orders (vitals frequency, I/O, neuro checks).
- You must manually schedule follow‑up visits and labs, instead of relying on a discharge template or automated system.
So integrate this into your mental checklist:
- After stabilization and initial diagnostics:
- “What monitoring would I ask the nurse for?”
- “What follow‑up labs/visits would I put in my discharge instructions?”
Add those as default orders.
Step 8: Simulate Exam Conditions in Week 4
People underestimate how much performance drops when you are tired and under timed conditions. Full simulations are how you expose the cracks before it matters.
How to run a CCS simulation
At least twice in week 4:
- Set aside a 2–3 hour uninterrupted block.
- Close everything else: phone, notifications, snacks.
- Run 6–7 CCS cases in a row, with:
- Strict case time limit
- Minimal breaks, same pattern you will use on exam day
Afterward, review:
- Did you start to rush and skip reassessments on later cases?
- Did you stop moving patients to correct setting because you got lazy?
- Did you forget global orders like monitoring or diet?
Take what you see and refine:
- Your written scratch‑paper checklist
- Your symptom bundles
- Your personal “don’t be dumb” list of common misses
Step 9: Know What Not To Do (Common CCS Traps)
There are patterns I see repeatedly that tank scores for no good reason. Avoid these.
Overordering everything “just in case”
If you order:
- CT head, CT abdomen, CT chest, MRI brain, full rheum panel, multiple invasive tests…
on a stable, straightforward patient, that is not “thorough.” It is bad medicine, and CCS will treat it that way.
Rule of thumb: If you would roll your eyes seeing that ordered in real life, do not order it here.
- CT head, CT abdomen, CT chest, MRI brain, full rheum panel, multiple invasive tests…
Ignoring the clock
Staring at the screen while results are pending is a waste.
- Always advance time in sensible intervals.
- Always reassess vitals and status after an intervention or a time jump.
Forgetting disposition
Stabilizing is not enough. You must:
- Admit to appropriate level (ICU vs step‑down vs floor)
- Or discharge with clear follow‑up, meds, and safety net signs.
Panicking on peds and OB cases
Take 2–3 nights and specifically practice pediatric fever and pregnancy emergencies. These are test‑writer favorites. And they are algorithmic.
Step 10: What To Do This Week, Day by Day (Concrete 7‑Day Micro‑Plan)
If your exam is 4 weeks away, here is exactly what I would assign you for the next 7 days.
Day 1
- Watch official CCS tutorial (once).
- Do 2–3 sample cases slowly, exploring interface.
- Start your one‑page command sheet skeleton.
Day 2
- Do 4 cases:
- 2 chest pain / SOB
- 2 abdominal pain / sepsis type
- After each:
- Write 2–3 bullet errors in your error log.
- Update your command sheet with missing orders.
Day 3
- Do 5 cases:
- Mix clinic and ED.
- Focus: always decide correct setting in the first 30 seconds.
- Spend 20 minutes after reading about any condition you clearly mismanaged.
Day 4
- Do 4 cases:
- At least 1 pediatric, 1 OB, 2 adult medicine.
- Practice writing out your cheat sheet from memory before starting the first case.
Day 5
- Do 5 cases focused on your weakest pattern so far.
- Update your error log and circle any error that has happened more than once.
Day 6
- Light day if you are also doing MCQs:
- 3 CCS cases only.
- Spend 30–40 minutes reorganizing and simplifying your command sheet.
Day 7
- Mini simulation:
- 4–5 CCS cases back‑to‑back with no long breaks.
- Brief review:
- What fell apart when you were tired? That is what you target next week.
Repeat this weekly rhythm with more cases and longer simulations as you progress.
Quick Visual: The CCS Case Flow You Should Be Running

| Step | Description |
|---|---|
| Step 1 | Read stem once |
| Step 2 | Move to ED/ICU |
| Step 3 | Clinic/Ward/Home |
| Step 4 | Global safety orders |
| Step 5 | Symptom-specific bundle |
| Step 6 | Advance time 30-60 min |
| Step 7 | Review results & vitals |
| Step 8 | Escalate care / adjust tx |
| Step 9 | Plan disposition & f/u |
| Step 10 | End case |
| Step 11 | Sick or stable? |
| Step 12 | Improving? |
Print this flow in your mind. You want this loop to be automatic.
FAQs
1. How many CCS cases should I do if I am very short on time (working 80-hour weeks)?
If you are slammed and realistically can only study CCS 4 days per week, I would set a hard minimum of 60–70 cases total before test day.
Priority order:
Interface mastery (first 10–15 cases):
You must know how to move patients, advance time, and enter common orders without thinking.High‑yield emergencies (next ~30 cases):
- Chest pain, SOB, sepsis, DKA/HHS
- Meningitis, GI bleed, PE, pregnancy emergencies
- Pediatric fever and dehydration
Chronic and preventive care (remaining cases):
- Diabetes, HTN, hyperlipidemia, COPD, asthma
- Screening and vaccinations
If you only do 2–3 cases on a given day, make them deliberate practice: immediately review and log your errors, and fix those in the very next case.
2. Should I focus more on MCQs or CCS in the final 2 weeks?
If your MCQ percentage is consistently weak (for example, <60% on reputable Step 3 question banks), MCQs still deserve the bulk of your time. CCS alone will not carry a failing MCQ performance.
However, once your MCQs are in a safe range (mid‑60s+ on average), CCS is high‑yield time:
- A modest improvement in CCS—by not missing critical early stabilizing orders and key diagnostics—can give you a real bump.
- CCS prep also reinforces clinical reasoning that will bleed over into MCQs, especially management questions.
Smart split in the last 2 weeks for most people:
- 70–75% MCQ time
- 25–30% CCS time, tightly focused, with 1–2 full CCS simulations.
Open your calendar for the next 4 weeks and block out specific CCS sessions—days, times, and number of cases. Do it right now. If it is not on your schedule, it will not happen, and CCS will still be a weakness instead of an easy win.






















