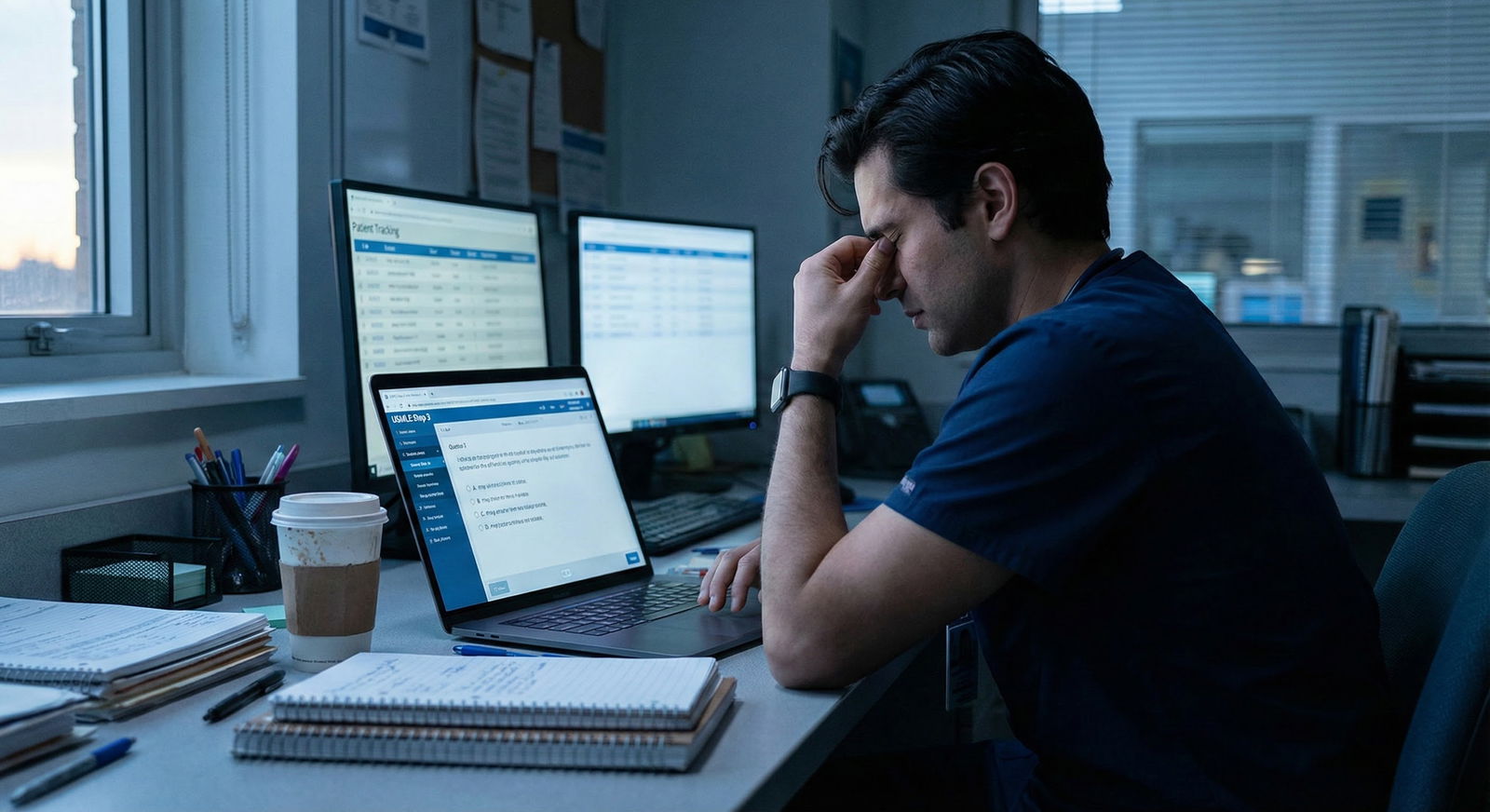
The usual Step 3 advice completely ignores what an ICU or night float block does to your brain and your schedule.
You are not lazy. You are not “bad at tests.” You are post-call, underslept, and running on caffeine and cortisol. The standard “do 40 questions a day no matter what” plan? Garbage for your situation.
Let me show you how to salvage Step 3 prep after a brutal ICU or night float month. Not in theory. In real, “I just admitted 15 patients and wrote 12 death notes this month” reality.
Step 1: Stabilize Your Brain Before You Touch a Qbank
If you try to “make up for lost time” on Step 3 prep the day your block ends, you will burn out and remember almost nothing. Your brain is cooked. Fix that first.
A 3-day reset protocol
For the first 3 days after ICU/night float, your job is recovery plus light activation, not heroics.
Day 1 – Full decompression
Non‑negotiables:
- Sleep until you wake up without an alarm (yes, really)
- Zero question blocks
- Gentle physical movement: 20–30 minutes walking outside
- Hydration: actual water, not only coffee
- One non-medical activity you enjoy: movie, friends, cooking, whatever
Optional:
- 15–20 minutes: skim a Step 3 CCS intro or watch 1 short video. Nothing intense. Just to reorient your brain to “test world exists”.
Day 2 – Turn the lights back on
Aim for:
- 2 short, low-pressure question “tastes”:
- 10–15 timed questions in the morning
- 10–15 tutor‑mode questions in the evening
- Review only the big learning points, not every micro-detail
- 30 minutes: walk, light jog, or stretching
- Bedtime target: before midnight, no screens 30 minutes before bed
Day 3 – First real Step 3 workday
Now you can test what you can handle.
Try:
- 1 full 20–25 question timed block
- Complete review of that block (max 1.5–2 hours)
- 10–15 CCS cases (if using a quick CCS simulator or outline) or 20 more questions in tutor mode
- Write down 5–10 “must-remember” learning points on a running digital or paper list
This alone separates you from most residents, who ping‑pong between total avoidance and panicked cramming.
Step 2: Time Reality Check – What You Can Actually Do
Stop pretending you are a board‑review monk with 8 free hours per day. You are a resident. You are tired. You have clinic, notes, and maybe kids or a partner who has not seen you all month.
You need an honest constraints audit:
How many weeks until Step 3?
- < 2 weeks
- 2–4 weeks
- 4–8 weeks
8 weeks
Current rotation intensity right after ICU/night float:
- Light (hemonc consult, research, elective)
- Moderate (wards, clinic heavy)
- Heavy (another ICU, ED nights, high-volume service)
Now plug those into realistic daily question targets.
| Time to Exam | Light Rotation | Moderate Rotation | Heavy Rotation |
|---|---|---|---|
| < 2 weeks | 60–80 Q/day | 40–60 Q/day | 30–40 Q/day |
| 2–4 weeks | 50–60 Q/day | 30–40 Q/day | 20–30 Q/day |
| 4–8 weeks | 40–50 Q/day | 25–35 Q/day | 15–25 Q/day |
| > 8 weeks | 30–40 Q/day | 20–30 Q/day | 10–20 Q/day |
If your numbers are way above that, you are writing fiction. And fiction does not pass Step 3.
Pick a target from the table and then cut it by 10–20% for the first week post-ICU/night float. You can always increase; you will not fix anything by overcommitting and then quitting.
Step 3: Build a “Post‑ICU” Study Schedule That Actually Works
You do not need a perfect master plan. You need a simple, repeatable daily structure that your sleep-deprived brain can follow.
Non‑negotiable rule
All real Step 3 work must be done:
- Before a long shift
- Or after a nap on post‑call days
Not at 1 a.m. in the call room. Not while cross-covering 40 patients. That is fantasy performance.
A practical daily template (for a moderate rotation)
Morning (pre‑work, 45–60 minutes)
- 1 timed block of 10–15 questions
- Immediate, focused review of:
- Why wrong?
- Why the right answer is right?
- One key teaching point per missed question
During the day (micro‑study, 10–20 minutes total)
- 2–3 “micro reviews”:
- On elevator rides
- Between patients
- While waiting for sign-out to start
Use:
- Flashcards (Anki or your own)
- Your “must‑remember” list
- Screenshots of Superbills or schemas (e.g., chest pain algorithm)
Evening (30–60 minutes)
- 10–15 tutor‑mode questions OR
- 1–2 CCS practice cases (no more than 30 minutes)
- Quick review of morning block key points
For heavy rotations, compress this:
- Morning: 10 timed questions
- Evening: 10 tutor‑mode questions
- One CCS case every other day
That will still move the needle. Consistency beats occasional 80‑question binges.
Step 4: Prioritize Like Someone Who Does Not Have Infinite Time
After a brutal block, you do not get to “cover everything equally.” You need to ruthlessly prioritize.
Focus on the Step 3 “money topics”
These are high‑yield, show up constantly, and you already saw them in ICU/night float:
- Sepsis and septic shock (resuscitation priorities, MAP targets, pressor choice)
- Vent management basics:
- ARDS vs COPD vs asthma settings
- When to intubate
- Acute coronary syndrome:
- STEMI vs NSTEMI initial management
- When to cath, when to stress test
- Stroke:
- tPA criteria
- Mechanical thrombectomy windows
- Blood pressure management
- DKA/HHS: fluids, insulin, electrolytes
- Common inpatient infections: CAP, HAP, UTI, cellulitis, C. diff
- CHF exacerbation: diuresis, when to use inotropes, when to hold beta‑blockers
- Pulmonary embolism diagnosis and treatment
- Acute GI bleed: transfusion thresholds, when to scope
- Alcohol withdrawal protocol (CIWA, benzo selection)
You already saw these 100 times during your block. Now you weaponize that experience.
Step 5: Convert ICU / Night Float Trauma into Step 3 Points
Here is the part everyone skips. Your month from hell is actually an asset—if you process it correctly.
Grab a notebook or a note app. Make a section called “From Service to Step 3”.
For each memorable case from your block, do this:
Write 1–2 lines:
- “45M with sepsis from pneumonia, BP 78/40, lactate 5.5, on norepi, on day 2 kidneys crashed.”
Ask: If this were a Step 3 question, what would they actually test?
Examples:- First‑line pressor in septic shock (norepinephrine)
- Target MAP (≥ 65 mmHg)
- When to add vasopressin
- When to give hydrocortisone
Turn it into a 1‑sentence rule or algorithm:
- “In septic shock, norepinephrine is first‑line pressor. MAP goal ≥ 65. Add vasopressin if norepi dose high, especially if refractory shock.”
If you have time, make a flashcard with that rule and one opposing option:
- Q: “Best first-line pressor in septic shock?”
- A: “Norepinephrine. Not dopamine. Not phenylephrine.”
Now you are not just passively doing questions. You are attaching Step 3 content to emotionally sticky real cases. Those stick in memory far longer.
Step 6: Fix the Two Biggest Post‑Night Float Problems: Sleep and Focus
If you do not repair your sleep, no plan will work. Step 3 is an 8–9 hour exam. Your brain cannot wing that on broken circadian rhythm.
Sleep repair protocol (for the first 7–10 days)
If you are coming off night float:
Days 1–3:
- Pick a wake time (example: 9 a.m.) and stick to it, no matter when you fall asleep
- No naps longer than 60 minutes, and not after 3 p.m.
- 10–20 minutes bright light exposure within 1 hour of waking (actual sun or a therapy light)
- Caffeine stops 8 hours before target bedtime
Days 4–10:
- Tighten wake time to ±30 minutes
- Add a wind-down routine:
- Same 3–4 steps every night: shower, tea, one chapter of a book, bed
- No study in bed, ever
- Expect 2–3 bad nights. Keep the routine anyway.
If you are coming off ICU days:
- You are often wired-tired. You fall asleep in chairs but then cannot sleep at night.
- Limit after‑work naps to 30 minutes.
- Move screens out of bed. Phone stays across the room.
- Use “study–relax–sleep” blocks:
- 45 minutes questions
- 15 minutes non‑screen relaxation
- Bed
Step 7: Use Question Banks Smarter (Not Just Harder)
You probably have UWorld. Maybe AMBOSS. Maybe a couple of CCS programs.
Your goal is not “finish every question.” Your goal is “learn to think exactly the way Step 3 expects under fatigue.”
How to run your Qbank after a brutal block
Small, high-quality timed blocks
- 10–15 questions timed, mixed, once or twice daily
- Treat them like mini-exam sections: no interruptions, no checking your phone
Aggressive review discipline For every missed question, answer three things out loud or in writing:
- What did I misinterpret?
- What key concept was this really testing?
- What mental shortcut can I use next time?
Pattern notes, not full transcripts Do not write down every detail. Capture:
- Repeated weak areas (e.g., OB management, ethics, statistics)
- “If X, then Y” style rules (algorithms)
- Opponent pairs:
- Chlamydia vs gonorrhea treatment
- Crohn vs UC features
- When to CT vs when to US
Weekly pattern check‑in (10–15 minutes)
- Once a week, look at your Qbank performance by system / topic
- Pick the top 2 weak systems and commit to:
- 10–15 extra questions in each over the next 3 days
- One short review resource (single chapter, 15‑minute video, summary table)
Step 8: CCS – Do Not Ignore It, But Do Not Let It Eat Your Schedule
Many residents overcorrect here. They panic about CCS, waste hours in the interface, and neglect MCQs, which are still most of your score.
Efficient CCS strategy for the exhausted resident
Week 1 post‑ICU/night float:
- Watch or read 1 simple CCS tutorial (60–90 minutes total)
- Understand:
- How to order tests
- How to advance time
- How to transfer level of care
- How to give patient counseling
Weeks 2–3:
- 3–4 CCS cases per week, total
- Focus on:
- Chest pain
- Shortness of breath
- Abdominal pain
- Vaginal bleeding / pregnancy
- Pediatric fever
For each case:
- Write 3 lines:
- Chief complaint
- Key initial orders you should always consider
- One mistake you made and the correct approach
Final 7–10 days before exam:
- Bump CCS to 1–2 cases most days
- Re‑run 3–5 of your worst cases, with a checklist next to you
Step 9: Repair Your Confidence After a Demoralizing Month
ICU or night float often leaves you feeling dumb, behind, and inadequate. That mindset kills Step 3 performance more than any missed topic.
You are not starting from zero. You just did high‑acuity medicine for weeks. Your problem is not knowledge alone. It is test‑format translation and fatigue.
Carve out 5 minutes at the end of each day for a quick “evidence of competence” review:
Write:
- 1 thing you handled well clinically that day (even if small)
- 1 thing you learned from a question that you could use on the wards
- 1 system/topic you feel slightly more comfortable with now than last week
This is not “toxic positivity.” It is data collection against your brain’s default narrative of “I am failing.” You need that data when you sit in front of an 8‑hour exam.
Step 10: Concrete Plans by Time Remaining
Let me give you very blunt, realistic battle plans depending on how much time you have from the end of your brutal block.
If you have < 2 weeks until Step 3
You are in salvage mode, not perfection.
Your goals:
- 500–700 high‑quality questions reviewed
- Basic CCS familiarity and 10–15 cases completed
- Solid routines for sleep, caffeine, and stamina
Daily (light/moderate rotation):
- 2 blocks of 20 timed questions
- 1 block of 10–15 tutor‑mode questions
- 1–2 CCS cases
- 30–40 minutes of review of “must memorize” notes in the evening
Daily (heavy rotation):
- 1 block of 20 timed questions
- 10–15 tutor‑mode questions later in the day
- CCS: 1 case on days off, skip on brutal days
Last 2–3 days:
- No new resources
- One moderate‑length self‑assessment or two long mixed blocks to test stamina
- Sleep and routine take priority over extra questions
If you have 2–4 weeks
Your goals:
- Finish most of your main Qbank once
- Identify and patch top 3–4 weak areas
- Do 20–30 CCS cases
Weekly structure:
- 5 days “full” days, 1 light day, 1 rest / social day
- 40–60 Q/day on most days (scaled down if heavy rotation)
- 5–7 CCS cases per week
Your week might look like:
- Mon–Fri: 2 x 20‑Q blocks + 1 CCS case
- Sat: 1 self‑assessment or 2 long blocks + light review
- Sun: 15–20 questions only, plus mental rest
If you have 4–8 weeks
You can actually rebuild in a civilized way.
Stage 1 (first 2 weeks post‑ICU/night float):
- Focus: rhythm, recovery, and base question volume
- 30–40 Q/day moderate, 20–30 Q/day heavy
- 3–4 CCS cases/week
Stage 2 (last 2–4 weeks):
- Ramp to your target daily volume from the table
- Add:
- 1 self‑assessment every 10–14 days
- Deliberate review of weakest 2–3 systems per week
If you have > 8 weeks
Reschedule Step 3 to fall after a lighter block if you can. You have the luxury of strategy.
Phases:
- Weeks 1–4: slow, steady build
- Weeks 5–8: higher‑intensity practice, more CCS, targeted weak‑spot repair
- Final 2 weeks: stabilization, stamina runs, and sleep optimization
Step 11: What to Do If You Are Already Burned Out on Studying
Very common scenario: you tried to “keep up” during ICU/night float, failed, and now you feel behind and ashamed. Which makes you avoid studying even more.
Fix this with very small wins and hard limits.
For 3–5 days, cap yourself at:
- 15–20 questions per day, maximum
- 1 CCS case every other day, maximum
And a minimum:
- 10 questions + review, that is it
Why? Because success rewires the avoidance loop. You need to experience:
“I said I would do 15 questions and I did it.”
Not: “I planned 80 and did 12 so I am a failure.”
After 3–5 days of clean wins, increase by 5–10 questions per day until you hit your realistic target.
Visual: Balancing Qbank, CCS, and Recovery

| Category | Value |
|---|---|
| Qbank MCQs | 45 |
| CCS Practice | 15 |
| Content Review/Notes | 10 |
| Sleep & Recovery | 30 |
Step 12: One‑Week Sample Plan Right After ICU/Night Float
To make this painfully concrete, here is a 7‑day blueprint assuming:
- You just finished a brutal month
- You have 3–4 weeks until Step 3
- Next rotation is moderate intensity

| Period | Event |
|---|---|
| Reset - Day 1 | Full rest, no blocks, light reading only |
| Reset - Day 2 | Two 10-15 question mini-blocks |
| Ramp - Day 3 | One 20-25 Q timed block + light CCS |
| Ramp - Day 4 | Two 20 Q blocks + 1 CCS case |
| Ramp - Day 5 | One 20 Q block + targeted weak-area review |
| Consolidate - Day 6 | Longer mixed block or self-assessment |
| Consolidate - Day 7 | 15-20 Q only + recovery and planning |
Layer your own realities (post‑call, clinic days, golden weekends) on top of that. The skeleton stands.
Key Takeaways
- You do not fix a brutal ICU or night float month by “grinding harder.” You fix it by structured recovery, realistic daily targets, and ruthless prioritization.
- Small, consistent question blocks plus targeted CCS practice beat unfocused marathon sessions, especially when you are tired.
- Your worst call nights are not wasted time; they are raw material. Turn your actual patients into memorized Step 3 rules and you will outperform people who only studied from books.
FAQ
1. I failed Step 3 once after a bad rotation. Should I delay my retake if I just finished ICU/night float?
If you failed once, you need a real 3–6 week window of structured prep, ideally during a lighter rotation. If your retake date falls within 1–2 weeks of finishing another brutal month, I would seriously consider rescheduling if your program allows. One more failure is harder to explain than a reschedule with a plan.
2. Is it even worth doing CCS practice if I am short on time and exhausted?
Yes, but in a limited, strategic way. You do not need to master every niche CCS scenario. You do need to understand the interface and the logic of initial orders, disposition, and follow‑up. Fifteen to thirty well‑chosen cases, done carefully, will give you most of the benefit.
3. How many self‑assessments should I do after a rough block?
If you have less than 2 weeks: usually one. If you have 2–4 weeks: one early to calibrate, one about 7–10 days before the exam. More than that is optional and only if they do not cannibalize your Qbank and review time. The value is trend and stamina, not the exact three‑digit number.
4. What if my schedule is so chaotic that I keep missing my “ideal” plan?
Then your plan is wrong, not you. Scale it down until you hit it 4–5 days in a row. That might mean 10–15 questions on busy days and 30–40 on off days. Build around your rotation reality instead of fighting it. Consistency with a smaller plan beats ambitious plans you never follow.






















