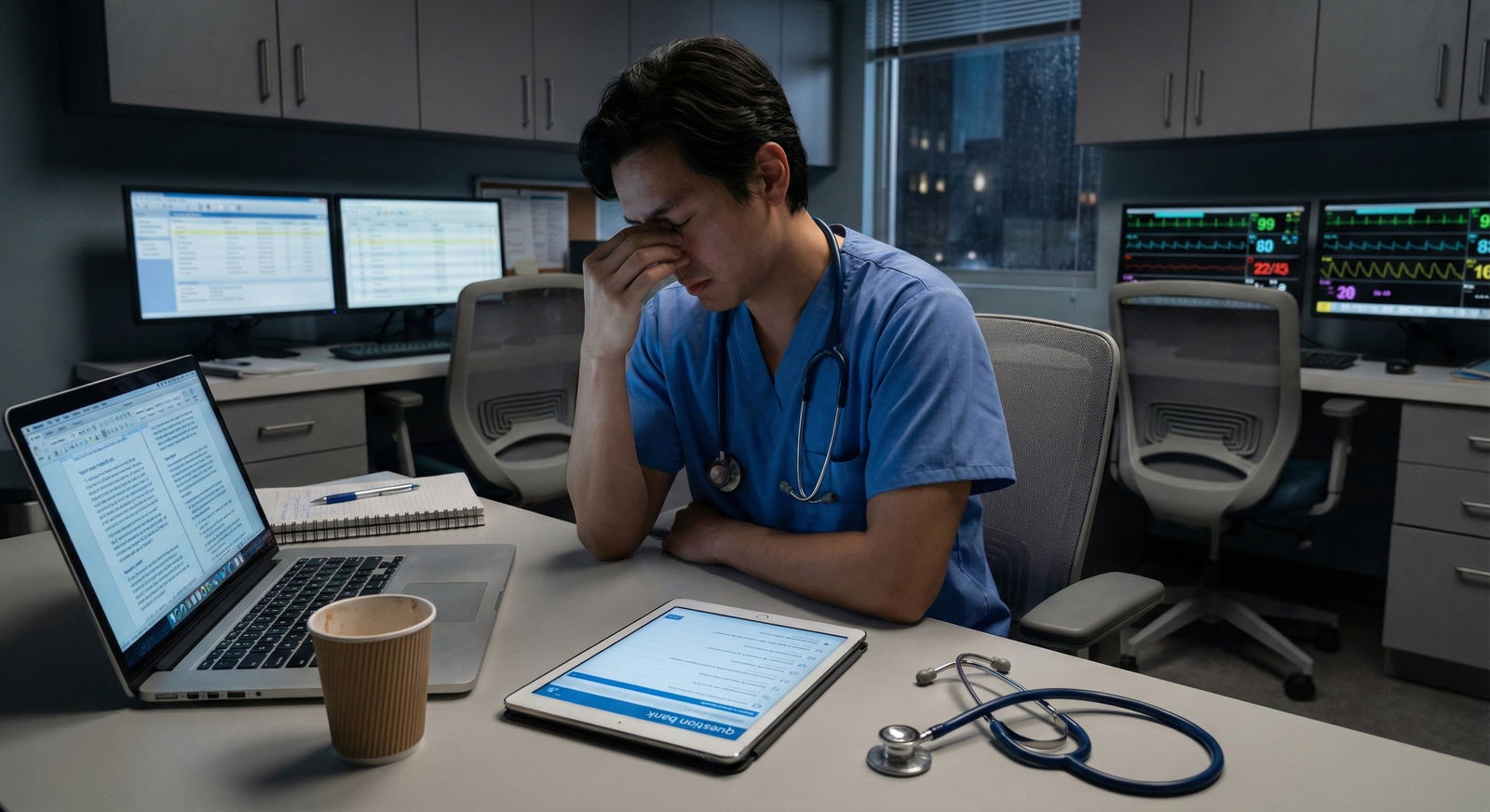
You just finished sign-out. It is 6:42 pm. You have eight active patients, two are marginally stable, and your phone has not been quiet for more than 10 minutes all day. Step 3 is in three weeks. There is no “golden month” of dedicated. There is this: a string of shifts that never seem to line up with your study plans.
You are not getting dedicated time.
So you need something better: a system that survives reality. Fatigue. Nights. Cross-cover disasters. A system that works shift-by-shift, not in some fantasy calendar where you have 4 weeks off.
That is what I am going to build for you here. A hard, practical blueprint to get through Step 3 with:
- No real dedicated time
- Unpredictable schedules
- A brain that is often half-fried
You will not love every part of it. But it works.
Step 3 Reality Check (and Why Your Old Study Style Fails Now)
First problem: you are still thinking about Step 3 like Step 1 or Step 2 CK. That is why you feel stuck.
Here is the honest breakdown.
| Feature | Step 1 | Step 2 CK | Step 3 |
|---|---|---|---|
| Focus | Mechanisms | Diagnosis/Treatment | Management & Safety |
| Question Style | Basic science heavy | Clinical vignettes | Real-world decision making |
| Time Flexibility | Often months dedicated | Some dedicated time | Usually none |
| Clinical Context | Hypothetical | Mixed | “You are the resident” scenarios |
| New Component | None | None | CCS (case simulations) |
Step 3 is not testing whether you remember every enzyme. It is asking:
- Can you stabilize this crashing patient?
- Do you know what to do first, not just what is theoretically correct?
- Will you order the right tests at the right time, and not order pointless garbage?
And you are now:
- Tired
- In the hospital constantly
- Dealing with real patients and real pages
That is actually an advantage—if you know how to weaponize it.
So the strategy is simple:
Use your shifts as your “content review,” and your “study time” as focused, high-yield drilling (questions + CCS) instead of open-ended reading.
Step 3 Blueprint Overview: The Core Rules
Let me lay out the framework first, then we will go shift-by-shift.
Non‑negotiable rules (yes, really non‑negotiable)
Daily contact with Step 3 material.
Even on your worst days: 10–15 questions or 1 CCS case. Zero days off. The brain forgets fast when you are exhausted.Question bank is primary.
UWorld Step 3 (or an equivalent high-yield bank) is your main resource. Everything else is secondary.CCS is not optional and not “for later.”
You need 15–20+ practice cases minimum. Most people push CCS to the end and regret it.Use your clinical work as study.
Every interesting patient = Step 3 scenario. You convert real cases into Step 3 learning points.You do not “binge-study” on post-call.
Post-call days are for recovery plus 10–15 light questions or one CCS case. You will not build hero points by burning yourself out.
Step 3 in 3–6 Weeks: Work-Back Plan
You said: No dedicated time. That usually means you are 3–8 weeks out and on full clinical duty.
Let us build a realistic workload for 4–6 weeks. Adjust the numbers based on your exact time frame.
Target Volumes
- Question bank: ~1,200–1,600 questions (full UWorld)
- CCS cases: 20–30 cases (mix of interactive + read-through)
- Full-length practice: 1–2 self-assessments (UWorld or NBME style if available)

| Category | Value |
|---|---|
| QBank Questions | 250 |
| CCS Cases | 5 |
| Self-Assessments | 0.5 |
A solid weekly target if you have 4–6 weeks:
- QBank: 200–300 questions / week
- CCS: 4–6 cases / week
- Assessment: One full practice test around ~2–3 weeks before
Now the real issue: where the hell does this fit between shifts?
Shift-by-Shift Blueprint
We will go through:
- Day shifts
- Night shifts
- Post-call days
- Golden weekends / random days off
1. Day Shift Schedule (the most common disaster zone)
Scenario: 6 or 7 am – 5/6/7 pm, depending on your service.
Here is a structure that actually works.
Morning: Pre-shift (20–30 minutes)
You will not want to do this. Do it anyway.
- Wake up 30 minutes earlier than normal.
- Goal: 10–15 mixed QBank questions (tutor mode allowed).
- Focus:
- Interpret vignettes quickly
- Reinforce “first step in management” logic
This is not your deep learning block. It is exposure, pattern recognition, and keeping your test brain warm.
During Shift: Micro-learning from your own patients
You are going to turn 1–2 cases per day into Step 3 reps.
Pick:
- 1 patient with a bread‑and‑butter condition:
- COPD exacerbation
- DKA
- NSTEMI
- CAP, pyelo, PE, etc.
For each of these, quickly (in a 3–5 min break) answer in your head or notes:
- What is the next best step in management?
- What are the must-not-miss orders?
- What labs or imaging are actually needed? What is unnecessary?
- What is the appropriate disposition (admit, ICU, floor, discharge)?
You are training the same decision tree Step 3 expects.
You can formalize this:
Keep a small note in your phone titled “Step 3 Patterns”
For each patient, jot down a 2–3 line algorithm:
- DKA:
- ABC, bolus fluids
- Insulin drip + electrolyte monitoring
- Replace K before insulin if K <3.3
- Transition to SQ insulin when AG closes
- DKA:
Every time you do that, you just studied without opening a book.
Evening: Post-shift block (30–45 minutes max)
After getting home, eat, shower, decompress for 20–30 min. Then:
- 10–20 QBank questions (timed or tutor, your choice)
- Focus on reading the explanations efficiently
- Do not chase references or open 3 textbooks
Total daily questions for a normal day shift:
- Morning: 10–15
- Evening: 10–20
→ 20–35 questions/day. That is enough if you stick to it.
2. Night Shift Strategy (when your brain is mush)
Night shifts wreck routines. You need a different system.
Assume a 7 pm – 7 am or 8 pm – 8 am block.
Pre-night: The “anchor session” (afternoon)
On your first night of a series:
- Wake up
- Eat
- Do a single, serious block of 20–30 questions sometime in the afternoon (1–2 hours before you get ready)
This is your main “study session” for that night.
During night shift: Be realistic
Middle of the night, your cognitive power is garbage. Use that.
If there is downtime and you are not dangerously tired:
- Do 5–10 questions at a time
- Or do 1 CCS case (especially if you have a computer and a quiet period)
If the night is chaos, forget questions. Use your patients:
- Any cross-cover “chest pain at 2 am” → build the ACS algorithm mentally
- Any sepsis or hypotension page → turn it into “what would Step 3 expect me to do first?”
Post-night: Controlled minimalism
After your shift, you are not a hero. You are a liability.
- No big question blocks
- At most: 5–10 light questions at home before bed or one quick CCS read-through
- If you are exhausted, skip questions but at least read 3–4 UWorld explanations you flagged earlier
The key during nights is preserving your streak. Zero days totally off from Step 3 content.
3. Post-Call Day Strategy
Post-call days are deceptive. You think you will study 3–4 hours. You will not. You will crash. So plan for that.
Here is the actual workable plan:
After sign-out, before going home:
- Do nothing. Go home. Sleep.
After a long nap and food:
- Aim for 15–20 questions max, tutor mode, lower pressure
- Or 1–2 CCS cases instead
No marathon sessions. Your hippocampus is not listening anyway.
Post-call days are about:
- Keeping your study habit alive
- Not overextending and then losing two more days recovering
4. Days Off / Golden Weekends: Your leverage days
This is where you do the heavy lifting.
On a full day off (not post-call):
Morning: Deep question block
- 2 blocks of 20–25 questions (separated by a decent break)
- Timed mode preferred
- Review explanations fully
Afternoon: CCS focus
- 2–4 CCS cases
- 1–2 interactive
- 1–2 read-throughs with structured note-taking
Evening: Clean-up + pattern review
- Go back over your “Step 3 Patterns” note and expand algorithms:
- Asthma management ladder
- Hypertensive emergency vs urgency
- Prenatal care visit schedule and testing
- Diabetes management intensification
These are also ideal days for a full-length practice exam (UWorld self-assessment). Plan that once in your prep, on a day off.
CCS: Turn It from Mystery Box to Point Machine
CCS is where otherwise decent candidates lose points because they treat it like an afterthought.
Do not.
How CCS actually behaves
You get:
- Simulated patients (clinic or ER)
- Time moves when you make orders or advance clock
- You must order:
- Appropriate initial stabilization
- Correct labs and imaging
- Correct medications & consults
- Ongoing monitoring
- Follow-up and disposition
CCS rewards you not for memorizing obscure management, but for sound process:
- Stabilize
- Diagnose
- Treat
- Follow-up
CCS Practice Blueprint (20–30 cases total)
Break it down:
Week 1–2:
- 1–2 cases / week, just getting familiar with the interface
- Focus: What options exist? How do vitals and labs update with time?
Week 3–4:
- 4–6 cases / week
- Mix emergent + outpatient:
- Chest pain
- Abdominal pain
- Prenatal visit
- Child with fever
- Trauma/ER eval
Last 1–2 weeks:
- Do all the common life-or-death cases:
- Sepsis, shock
- DKA, HHS
- Status asthmaticus
- PE, stroke
- ACS, unstable arrhythmias
- Do all the common life-or-death cases:

| Category | Intro/Interface | Common Outpatient | Emergent/ICU |
|---|---|---|---|
| Week 1-2 | 4 | 2 | 0 |
| Week 3-4 | 2 | 8 | 4 |
| Week 5-6 | 0 | 4 | 8 |
A simple CCS order framework
When you open a CCS case, run this mental checklist:
Stabilize
- ABCs: oxygen, IV access, monitors, vitals
- If sick: move to ICU / appropriate level of care
Basic orders (if appropriate)
- Pulse ox, continuous monitoring
- NPO if needed
- Pain control if not contraindicated
- Pregnancy test in women of childbearing age
Diagnostic workup
- Targeted labs (CBC, BMP, LFTs, lipase, etc.)
- Disease-specific tests (troponins, d-dimer, ABG, etc.)
- Imaging (CXR, US, CT, etc.) if indicated
Initial treatment
- Antibiotics if suspect infection
- Anticoagulation if high suspicion for PE/DVT and no contraindication
- Fluid resuscitation if hypotensive
- Correct glucose, electrolytes, etc.
Reassessment
- Advance time by an hour or so
- Recheck vitals, labs
- Adjust management
Disposition & follow-up
- Admit/ICU vs discharge with follow-up
- Long-term management orders where relevant
If you drill this structure, CCS goes from terrifying to formulaic.
How to Study When You Are Brain-Dead
You will have days where “real” studying is not happening. Fine. You still have options.
Here is how to triage your brainpower.
High-energy days (rare, but use them)
- Timed question blocks (20–40 at a time)
- Full review of explanations
- Structured notes or Anki if you like that
- CCS interactive cases
Medium-energy days (common)
- Tutor-mode questions (10–20)
- Lighter CCS read-only cases
- Quick review of flagged QBank items
Low-energy days (very common on inpatient)
- Open your QBank app, do 5–10 questions max
- Or just read explanations of previously done questions
- Or read 1–2 CCS case write-ups, no active simulation
You are not looking for perfect, you are looking for contact with the material daily.
Stop Wasting Time: What Not to Do
Let me be direct about the common mistakes.
1. Massive, pretty notes
You do not have time to build a 60-page Step 3 notebook. It will look nice. It will not move your score much.
If you must take notes:
- One running digital note / doc only
- Only algorithms and patterns, not long prose
- Example entries:
- “Afib with RVR – stable: rate control, echo, anticoagulation decision tree”
- “Preeclampsia vs severe features vs eclampsia – when to deliver”
2. Endless videos
If you are watching hours of video per day while on service, you are not actually preparing efficiently.
Videos can help for:
- CCS walk-throughs (short)
- A weak topic you truly never understood (e.g., ventilator management)
But watch with a purpose. Not as a way to avoid questions.
3. Saving CCS “for the last week”
That last week is usually a mess. You are tired, anxious, and behind on QBank.
Start CCS early with low intensity. Let familiarity build over weeks.
Sample 7-Day Micro-Schedule (Busy Resident, No Dedicated)
Here is a concrete schedule for a typical week on inpatient with one day off.
| Day | Schedule | Study Plan |
|---|---|---|
| Mon (Day shift) | 6a–6p | 10 Q AM, 15 Q PM |
| Tue (Day shift) | 6a–6p | 10 Q AM, 10 Q PM, 1 CCS read |
| Wed (Day shift) | 6a–6p | 15 Q PM only (tired) |
| Thu (Post-call or lighter) | 6a–12p | Nap, then 15 Q tutor, 1 CCS interactive |
| Fri (Day shift) | 6a–6p | 10 Q AM, 10 Q PM |
| Sat (Day off) | Off | 2×20 Q blocks, 3 CCS cases |
| Sun (Night shift) | 7p–7a | 20–25 Q afternoon, 5–10 Q overnight if quiet |
That week still gives you:
- 120–150 questions
- 5–6 CCS encounters
Multiply that by 4–5 weeks and you have more than enough exposure.
Tracking and Adjusting Without Overthinking It
You do not need a beautiful spreadsheet. You need a brutally simple tracker.
Use:
- A note on your phone
- Or a whiteboard in your room
Columns:
- Date
- Questions done (total)
- CCS cases (count)
- Quick note (“weak: OB, neuro; focus tomorrow”)

| Step | Description |
|---|---|
| Step 1 | Daily Plan |
| Step 2 | Do QBank / CCS |
| Step 3 | Log Progress |
| Step 4 | Target Topics On Next Day Off |
| Step 5 | Maintain Current Mix |
| Step 6 | Pattern of Weak Areas? |
Once a week (probably on your day off):
- Look at the weak areas that keep repeating
- Devote one focused block (20–30 questions) to those:
- OB
- Peds
- Psych
- Biostats / ethics
You are not trying to “master everything.” You are trying to drag up your weak zones to “safe” and sharpen your strong areas where Step 3 gives easy points (management, safety, CCS).
Using Real Patients as Step 3 Reps (This Is Your Secret Weapon)
Residents who score well on Step 3 with no dedicated time almost all do this instinctively.
For every common condition you see on service, ask yourself:
If this were a Step 3 question:
- What would they want as the next best step?
- What would be a dangerous but tempting wrong answer?
For each admission, think in algorithms:
- “What would I do if this patient crashed in the next 10 minutes?”
- “What labs and imaging are absolutely required? What is fluff?”
After sign-out, pick 1–2 cases and do a 2-minute mental CCS run:
- Initial orders
- Consults
- Monitoring
- Disposition
You are already doing the medicine. The trick is to consciously map it to exam logic.
The Psychological Part: How to Not Spiral
This exam comes at a time when you are underpaid, overworked, and already stretched.
Three quick points that matter more than people admit:
Perfectionism kills performance here.
You will not cover every topic. Accept it. This is a competence exam, not an honors exam. The pass bar is lower than you think, but it expects consistency.Fatigue is part of the design.
Step 3 is two long days for a reason. You are supposed to be tired. That is not a sign you are failing; it is the playing field.You are learning this stuff every day anyway.
You are closer to ready than your anxiety says. Channel what you see daily into exam answers.
Your Very Next Step (Today)
Do this right now, before you close this:
- Open your QBank.
- Create a 10-question mixed block (any subject, any system).
- Set a timer for 20–25 minutes.
- Do the block. Review only the explanations for questions you got wrong or guessed.
When you finish:
- Open a single note on your phone titled “Step 3 Patterns.”
- Write down three management algorithms or principles you either learned or relearned from that block.
That is your core habit. You stack that—shift after shift—for 4–6 weeks, and Step 3 stops being this impossible monster and becomes what it really is: a long, annoying exam on things you are already doing every day.






















