
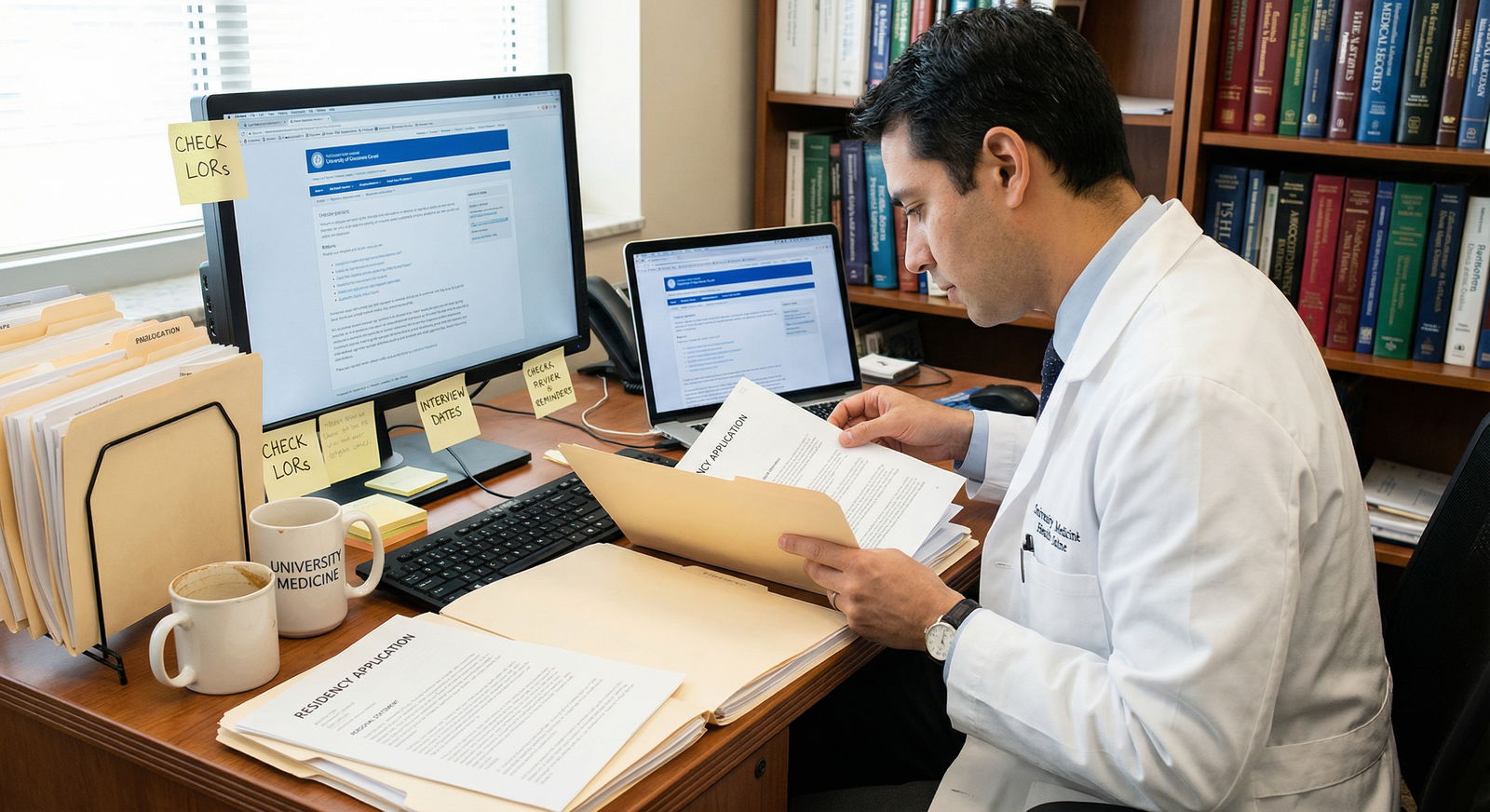
Common Residency Application Mistakes to Avoid if You Want to Match Successfully
The transition from medical school to residency is one of the most consequential steps in your healthcare career. After years of exams, clinical rotations, and constant evaluation, everything converges in one high-stakes process: your residency applications and the Match.
Strong board scores and solid clinical performance are important, but they are not enough on their own. Many highly qualified applicants damage their chances by making avoidable application mistakes—errors that can lead to fewer interview offers and, in some cases, not matching at all.
This guide breaks down the most common residency application mistakes, explains why they matter, and gives you concrete, actionable strategies to avoid them. Whether you are just beginning to plan your ERAS season or finalizing your materials, use this as a checklist to strengthen every component of your application.
Understanding the Residency Application Landscape
Before looking at specific mistakes, it helps to step back and understand what residency programs are really evaluating.
Most U.S. residency applications are submitted through the Electronic Residency Application Service (ERAS). A typical residency application includes:
- Personal Statement (often specialty-specific)
- Curriculum Vitae (CV) / ERAS Experiences section
- Letters of Recommendation (LORs)
- USMLE or COMLEX scores
- Medical school transcript and MSPE (Dean’s Letter)
- Supplemental applications (e.g., supplemental ERAS, specialty-specific forms, or program-specific questions)
What Programs Are Looking For
Residency programs are not just screening for intelligence or test-taking skills. They are trying to answer several core questions:
- Can this applicant safely care for patients?
- Will they be reliable, professional, and teachable?
- Do their experiences and values align with our program’s culture and mission?
- Are they truly committed to this specialty?
- Will they work well with our team and patients?
Every part of your application—from your Personal Statement to your recommendation letters and even your email communication—contributes to how programs answer these questions.
1. Incomplete or Inaccurate Application Materials
One of the most preventable errors in residency applications is submitting incomplete or inaccurate information. In a highly competitive environment, basic administrative mistakes can quickly move your file to the bottom of the pile.
Common Application Errors to Avoid
1. Missing Required Documents
- Forgetting to assign USMLE/COMLEX scores to programs
- Not uploading or assigning the correct Personal Statement to each specialty
- Failing to ensure all required Letters of Recommendation are in and assigned
- Overlooking program-specific supplemental requirements
Programs often receive hundreds or thousands of applications; if yours is missing key components on review day, they may simply move on.
2. Typos and Incorrect Information
Errors such as:
- Misspelling your own name or email address
- Incorrect contact information for you or your letter writers
- Mismatched dates in your CV and Experiences section
- Inconsistent exam scores or attempts (e.g., not disclosing a prior failure)
These mistakes can come across as careless and raise questions about your attention to detail—an essential trait in medicine.
Practical Strategies to Get It Right
- Create a master checklist of every required document for ERAS and for each program.
- Use a timeline: Start gathering materials months in advance (often by late spring or early summer).
- Double- and triple-check personal data, program lists, and document assignments before certification.
- Have a trusted reviewer (advisor, mentor, or senior resident) scan your application for discrepancies.
Real-World Example
Sarah, an otherwise strong applicant, focused heavily on crafting a beautiful Personal Statement. Under time pressure, she submitted her ERAS application without realizing she had not released her USMLE Step 2 score to programs. She only noticed weeks later—after interview invitations had already gone out. Although she had excellent scores, many programs never saw them, likely reducing her overall interview yield.
2. Ignoring Program-Specific Requirements and Fit
Not all residency programs are the same. They differ in patient population, educational philosophy, research focus, size, and culture. Treating every program as interchangeable is a major application mistake.
Mistake: Failing to Research Programs Thoroughly
Some applicants send the same generic application to every program without:
- Reviewing each program’s website, mission, and curriculum
- Understanding typical applicant profiles (board scores, experiences)
- Noting special requirements (e.g., number and type of LORs, research expectations, visa policies, or specific rotations)
Programs can quickly tell when an applicant has not taken time to understand who they are and what they value.
Mistake: Not Following Instructions
Common examples include:
- Sending three letters of recommendation when the program clearly requests four
- Ignoring a prompt to address a specific question in your Personal Statement
- Skipping a required supplemental application or secondary essay
- Not completing program-specific fields on ERAS or supplemental portals
Even small lapses can be interpreted as poor attention to detail or lack of sincere interest.
How to Show Genuine Program Interest and Fit
- Create a program spreadsheet including:
- Requirements (LOR types, number, USMLE/COMLEX thresholds)
- Special tracks (research, global health, primary care)
- Location, call schedule, fellowship match data
- Tailor your Personal Statement or experiences:
- Highlight experiences aligned with the program’s strengths (e.g., community health, research, underserved populations).
- Mention specific program features in interviews and, when appropriate, in your Personal Statement (without overdoing it or copying/pasting the website).
- Follow instructions precisely, including word counts, document types, and formatting.
Real-World Example
John applied to multiple Internal Medicine programs using the exact same Personal Statement and minimal program research. Several of these programs emphasized community engagement and primary care; others were research-heavy academic centers. John’s generic statement failed to speak to either group. Meanwhile, his peers who tailored their materials and referenced each program’s strengths received significantly more interview offers.
3. Submitting a Weak or Generic Personal Statement
Your Personal Statement is one of the few narrative elements of your application where you control the story. Underestimating its importance or treating it as a formality is a critical residency application mistake.
Common Personal Statement Pitfalls
1. Being Vague, Generic, or Cliché
Phrases like “I have always wanted to help people” or recounting the same standard “I loved my third-year rotation” story without depth do not differentiate you. Programs read hundreds of these each year.
2. Over-Focusing on Achievements Instead of Motivation
Your CV already lists your accomplishments. The Personal Statement should explain:
- Why this specialty?
- How did your experiences shape you as a future physician?
- What kind of resident and colleague will you be?
If you only re-list your awards and research, you miss a chance to convey your values, insight, and maturity.
3. Lack of Structure or Coherence
Disorganized narratives, abrupt topic shifts, or overly long and unfocused essays are hard to follow. Program directors often skim; clarity and impact in the first few paragraphs are key.
4. Ignoring Specialty and Program Fit
Submitting the same Personal Statement to dramatically different specialties or failing to explain your commitment to one specialty can raise red flags about your career direction.
How to Write a Strong, Compelling Personal Statement
Open with a specific, meaningful story
Choose a clinical encounter, moment of insight, or personal experience that genuinely shaped your path. Keep it concise and reflective, not melodramatic.Connect your story to the specialty
Explain how that experience led you toward Internal Medicine, Pediatrics, Surgery, Psychiatry, etc. Be explicit about what aspects of the specialty resonate with you (e.g., continuity of care, procedural work, diagnostic reasoning).Highlight growth and reflection
Programs value self-awareness. Discuss what you learned, how you responded to challenges, and how those lessons will guide you as a resident.Show—not just tell—your qualities
Instead of “I have strong communication skills,” describe a situation where you navigated a difficult conversation with a patient or team.Keep it professional and polished
Avoid overly casual language, controversial topics (unless handled carefully and professionally), or negative commentary about colleagues or institutions.
Real-World Example
Emily was passionate about women’s health and had extensive advocacy experience. However, in her Personal Statement, she focused almost entirely on her publications, presentations, and Step scores. She barely mentioned why she cared about Obstetrics & Gynecology or how her advocacy shaped her as a physician. Programs saw a technically strong applicant but not the depth of her commitment—an opportunity lost.
4. Weak, Generic, or Misaligned Letters of Recommendation
Letters of Recommendation (LORs) are among the most influential parts of your residency applications. A strong letter can elevate an otherwise average portfolio, while a weak or lukewarm letter can quietly undermine even a high-achieving applicant.
Mistake: Choosing the Wrong Recommenders
Common errors include:
- Selecting faculty with big names but who barely know you
- Asking pre-clinical instructors rather than clinical supervisors (when clinical letters are preferred)
- Requesting letters from fields unrelated to your chosen specialty (when specialty-specific letters are expected)
- Not confirming that the writer is comfortable writing you a strong letter
Mistake: Accepting Vague, Non-Specific Letters
Letters that say only “hard-working,” “nice,” or “good student” without concrete examples are often interpreted as minimal endorsements. Program directors are adept at reading between the lines.
Best Practices for Strong Letters of Recommendation
Choose people who know you well in a clinical setting
- Attending physicians from core or sub-internship rotations
- Research mentors with substantial interaction and direct supervision
- Program directors or clerkship directors who have observed your performance
Ask early and ask clearly
- Request letters at the end of a strong rotation while your performance is fresh.
- Ask directly: “Would you feel comfortable writing me a strong letter of recommendation for [specialty] residency?”
Provide supporting materials
- Updated CV
- Draft of your Personal Statement
- Brief summary of key cases or projects you worked on with the letter writer
- Your specialty choice and type of programs you’re targeting
Clarify letter logistics
- Confirm ERAS submission deadlines
- Politely remind them as the deadline approaches, if needed
Real-World Example
Mark requested letters from senior faculty members with national reputations, assuming their names would impress programs. In reality, these attendings had limited interaction with him and wrote generic letters like “performed adequately on the service.” Programs weighed those letters far less than the glowing, specific letters some of his peers received from less famous but more involved mentors.
5. Underestimating Achievements and Extracurricular Activities
Many applicants focus so heavily on exams and core rotations that they downplay or overlook the rest of their experiences. This can be a significant mistake because programs want to understand who you are beyond your board score.
Mistake: Minimizing Non-Clinical Experiences
Your non-clinical background—teaching, leadership roles, previous careers, athletics, arts, or tech skills—can all:
- Demonstrate resilience, discipline, creativity, and teamwork
- Differentiate you from applicants with similar academic metrics
- Signal future contributions to the residency program (teaching, quality improvement, leadership)
Mistake: Not Highlighting Volunteer Work and Community Engagement
Community service and advocacy work are especially important in many specialties and programs that value service to underserved populations. When you fail to highlight:
- Long-term volunteer commitments
- Community outreach projects
- Involvement in free clinics, global health, or health policy
…you miss a chance to show empathy, social responsibility, and commitment to holistic care.
How to Showcase Your Experiences Effectively
Use the ERAS Experiences section strategically
- Choose your “Most Meaningful” entries thoughtfully.
- Describe impact and outcomes, not just duties.
- Use concise, action-oriented language.
Connect experiences to core residency competencies
- Leadership in a student group shows organizational and team skills.
- Teaching experience demonstrates communication and mentorship ability.
- Research reveals curiosity, persistence, and critical thinking.
Reflect on growth
- Briefly note what you learned and how it prepared you for residency.
Real-World Example
Rachel volunteered for years at a local free clinic and served in leadership roles in student organizations. In her ERAS application, she listed these activities but provided minimal detail, treating them as afterthoughts. Her peers who framed similar roles with specific examples of leadership, impact, and personal growth were more memorable and competitive in holistic reviews.
6. Unprofessional or Inconsistent Communication and Follow-Up
Program directors and coordinators notice how applicants communicate. Emails, thank-you notes, and response times all contribute to impressions of maturity and professionalism.

Mistake: Skipping Thank-You Notes After Interviews
While not every program expects thank-you emails, many interviewers do appreciate them. Failing to send a brief, professional note can:
- Miss a low-effort opportunity to reinforce your interest
- Make you seem less engaged compared with peers who do follow up
Mistake: Poor Email Etiquette
Common problems:
- Overly casual tone or unprofessional language
- Using non-professional email addresses
- Long delays in responding to program communications
- Sending mass, copy-paste messages that are clearly generic
How to Communicate Professionally
- Use a professional email address (e.g., firstname.lastname@…)
- Respond promptly (ideally within 24–48 hours) to any program communication.
- Be concise, respectful, and clear in all messages.
- Customize thank-you emails
- Mention one or two specific aspects of the conversation or program.
- Reiterate your interest without making promises you cannot keep.
Real-World Example
Daniel attended several interviews but never sent thank-you notes, believing they were unnecessary. Some interviewers interpreted this as limited interest in their programs. In a competitive ranking discussion, small differences—like perceived enthusiasm and professionalism—can tip the scale between two similar applicants.
7. Inadequate Interview Preparation
The interview is often the most heavily weighted component once you get your foot in the door. Many otherwise strong applicants underperform because they underestimate the need for deliberate preparation.
Mistake: Not Practicing Interview Skills
Even highly articulate students can struggle under pressure if they have not:
- Practiced common residency interview questions
- Organized their thoughts into clear, concise narratives
- Refined explanations of their CV, any red flags, and their career goals
Mistake: Fumbling Basic or Behavioral Questions
Questions like:
- “Tell me about yourself.”
- “Why this specialty?”
- “Why our program?”
- “Describe a conflict you experienced and how you resolved it.”
- “Tell me about a time you made a mistake.”
These are predictable, yet many applicants are caught off guard and ramble, contradict themselves, or provide superficial answers.
Strategies for Strong Residency Interviews
Do mock interviews
- With advisors, residents, or career services.
- Practice both traditional and behavioral questions.
Use the STAR method for behavioral questions
- Situation – Brief context
- Task – Your role
- Action – What you did
- Result – Outcome and what you learned
Prepare your core messages
- 2–3 key strengths and how you have demonstrated them
- A thoughtful explanation of any red flags (e.g., exam failures, leave of absence)
- Clear, specific reasons you are interested in that specialty and program type
Prepare questions to ask programs
- About curriculum, mentorship, wellness, research, and fellowship outcomes.
- Avoid questions easily answered on the website.
Real-World Example
Jessica had strong scores and solid clinical evaluations, but she did not rehearse common interview questions. In multiple interviews, she struggled to articulate why she chose her specialty and what she hoped to accomplish in residency. Her responses seemed hesitant and disorganized, leading some programs to question her fit and readiness.
8. Poor Planning for the Match Process and Timeline
The National Resident Matching Program (NRMP) process has specific rules, dates, and timelines. Misunderstanding these can have serious consequences, even if your application materials are strong.
Mistake: Ignoring Key Dates and Deadlines
Potential issues include:
- Certifying ERAS application late, missing early review by programs
- Failing to register for the NRMP on time
- Forgetting to certify your rank order list by the deadline
- Missing deadlines for supplemental applications or program-specific tasks
Mistake: Not Understanding How the Match Works
Some applicants misunderstand critical aspects such as:
- How the algorithm favors applicant preferences
- How to build a realistic and strategic rank list
- The implications of including or excluding certain programs
- The Supplemental Offer and Acceptance Program (SOAP) procedures if you do not initially match
How to Navigate the Match Strategically
Familiarize yourself early with NRMP rules and timelines.
Use official resources: NRMP and ERAS guides, specialty-specific advice, and your school’s advising office.
Plan your application strategy
- Number and types of programs to apply to
- Geographic flexibility
- Balance of reach, target, and safety programs
Build a thoughtful rank list
- Rank programs in true order of preference—not based on where you think you are “most likely” to match.
- Do not rank a program you would not be willing to attend.
- Discuss your rank list with advisors who know your application well.
Real-World Example
Liam was an otherwise competitive applicant but did not pay close attention to NRMP deadlines. He delayed finalizing his rank list and missed the certification deadline, forcing it to remain incomplete. As a result, he did not match into his preferred program, despite having had a solid chance there.
Conclusion: Avoidable Mistakes Can Make the Difference
The residency application and Match process is demanding, but many of the most damaging missteps are entirely avoidable with planning, attention to detail, and honest self-assessment.
To maximize your chances of matching successfully:
- Start early and stay organized
- Treat every element—Personal Statement, Letters of Recommendation, CV, interviews, and communication—as part of a coherent professional story
- Research programs and show genuine interest and fit
- Seek feedback from mentors, advisors, and residents who have recently matched
- Understand the technical aspects and deadlines of ERAS and NRMP
Matching is not just about raw metrics; it is about presenting a thoughtful, authentic, and professional portrait of yourself as a future resident physician.
Frequently Asked Questions About Residency Application Mistakes

1. What is the most critical part of the residency application?
There is no single “most important” component—programs use a holistic review. However, several factors consistently carry heavy weight:
- USMLE/COMLEX performance (especially Step 2 in the current landscape)
- Clinical evaluations and MSPE
- Specialty-appropriate Letters of Recommendation
- Interview performance
- A focused, well-written Personal Statement that clearly explains your interest in the specialty
If forced to choose one area you fully control during application season, the Personal Statement and interview preparation are often where you can still significantly influence how programs perceive you.
2. How can I choose the right recommenders for my Letters of Recommendation?
Select recommenders who:
- Have directly supervised you clinically or in research
- Can comment on your work ethic, clinical reasoning, professionalism, and teamwork
- Know you well enough to provide specific examples
- Are within or closely related to your target specialty (especially for core letters)
When you ask, be upfront: “Would you feel comfortable writing me a strong, supportive letter for [specialty] residency?” If they hesitate, it is better to seek someone else.
3. How important are extracurriculars and non-clinical activities in residency applications?
While they do not replace strong clinical performance and exams, extracurriculars add valuable context to your candidacy. They can:
- Differentiate you in a large applicant pool
- Demonstrate leadership, service, resilience, and communication skills
- Signal alignment with a program’s values (e.g., community engagement, research focus, advocacy)
Programs increasingly value attributes beyond test scores, especially as more exams move to pass/fail. Thoughtfully presenting your extracurriculars can meaningfully strengthen your application.
4. Should I send thank-you notes after residency interviews?
Yes, it is generally advisable. Short, professional thank-you emails:
- Acknowledge the interviewer’s time
- Reaffirm your interest in the program
- Help keep you fresh in the interviewer’s mind
Avoid generic mass emails; instead, reference a specific part of your conversation or something you appreciated about the program.
5. What are some common residency interview mistakes, and how can I avoid them?
Common interview pitfalls include:
- Not having clear answers to “Why this specialty?” and “Why our program?”
- Rambling, unfocused responses to behavioral questions
- Speaking negatively about previous supervisors, schools, or colleagues
- Not being prepared to discuss red flags on your application
- Appearing disinterested, unprofessional, or late
You can avoid these by:
- Doing multiple mock interviews
- Preparing key stories using the STAR framework
- Reviewing your own application thoroughly so you can speak confidently about any detail
- Researching each program prior to the interview and preparing thoughtful questions
By understanding and avoiding these common residency application mistakes, you significantly improve your chances of matching into a program where you will thrive and grow as a physician.




















