The quiet assumptions about DO vs. MD clinical skills start before you ever touch a patient. And they’re not written anywhere. They live in attending lounges, in offhand comments on rounds, and in the pause before someone asks, “You’re a DO, right?”
Let me tell you exactly what faculty really assume about DO vs. MD students on day one. Because if you understand those assumptions early, you can weaponize them instead of getting blindsided by them.
The First-Day Reality: What’s Already In Their Heads
(See also: What Happens to DO vs. MD Applications in the First 5 Minutes of Review for more on initial evaluations.)
On day one of your clinical rotations, you walk onto the floor thinking you’re a blank slate.
You’re not.
By the time you introduce yourself, three things are already true:
- Your badge says DO or MD.
- The attending and residents already have a mental story about what that means.
- Nobody will say that story out loud.
I’ve sat in those pre-rotation meetings. “We’ve got three students this block: two MDs from [well-known university], one DO from [regional COM].” Then you see people’s faces. A raised eyebrow. A shrug. Or a quick, “Our DOs have usually been solid,” or “Keep an eye on them for Step knowledge.”
They’re making assumptions about:
- Your fund of knowledge
- Your clinical reasoning
- Your procedural comfort
- Your documentation skills
- Your professionalism and independence
Not because they’re evil. Because they’ve seen patterns over years and their brains do what human brains do: generalize.
Are those patterns always accurate? No. But you’re judged by them until you prove otherwise.
The Core Assumption: Knowledge vs. Hands-On Ability
Here’s the uncomfortable truth:
Most faculty assume DO and MD students are roughly equivalent at the bedside on day one of clerkships. What they do not assume is that you’re equivalent on exam-level medical knowledge and documentation.
If you’re DO, many attending physicians quietly expect:
- Slightly weaker standardized test strategy
- Slight unevenness in basic science recall
- Equal or better bedside manner and patient interaction
If you’re MD, many expect:
- Stronger test-taking and memorization
- Slightly more polished academic vocabulary and presentation style
- Variable bedside manner depending on school culture
They’re not sitting in pre-rounds saying, “This DO student can’t examine a patient.” They’re thinking, “We’ll see how their knowledge base stacks up and how they present.”
The big misconception students have is that faculty are hyper-focused on the letters “DO” vs “MD” for clinical skills. They’re not. They’re focused on two questions:
- Can you function safely?
- How much teaching will you need to not slow the team down?
The DO vs. MD label just tweaks their initial guess.
What Program Directors Tell Each Other (That You Never Hear)
I’ve heard these exact sentences in PD meetings and hallway conversations:
- “Our DO students usually have good people skills. Sometimes they’re behind on shelf-style questions.”
- “The MDs from [X school] are book-smart but helpless in the ED at first.”
- “That DO school? Their students hustle. I’ll take hustle over pedigree.”
- “If a DO student crushed Step 2, I don’t worry at all.”
Let me decode that.
They do not walk in thinking:
“DO = bad clinician, MD = good clinician.”
They think in tiers:
- School reputation + board scores set expectations for knowledge.
- Year after year of previous learners from those schools shapes expectations for work ethic and bedside performance.
- The DO/MD label mostly adds a bias about test performance and overall competitiveness.
On pure clinical skills day one—listening to lungs, doing an abdominal exam, writing a note—most faculty assume:
- Everyone is green.
- Everyone will be clumsy.
- Everyone will miss things.
Your degree letters color how generous they’re going to be while you learn.
The Real Day-One Checklist in Attendings’ Heads
Let me be blunt: nobody cares how many Anki cards you did.
On day one, attendings and senior residents are unconsciously grading you on:
- How you enter a room
- Whether you shake the patient’s hand and introduce yourself clearly
- How you present the patient later (organized vs. chaos)
- Whether your physical exam is at least coherent, even if incomplete
- Whether you can be left alone in a room for 5 minutes without doing something unsafe or weird
Here’s what’s different in their heads for DO vs. MD.
What They Assume About DO Students
- You’ll probably be comfortable talking to patients.
- You might be a little apologetic about being DO if you’re insecure. They notice that.
- They may or may not expect you to use OMM; some will ignore it, some will test you on it.
- They’ll watch closely to see if your medical knowledge matches your “I had to fight to get here” story.
One academic hospitalist told me directly:
“My DO students tend to be more coachable. They’re used to being underestimated. The weak ones crumble when they act like they have something to prove instead of just learning.”
That’s the unspoken test. Are you here to prove a point, or to work?
What They Assume About MD Students
- You’ll have the board-style knowledge roughly aligned with your school’s reputation.
- You may talk a better game than your exam room skills justify at first.
- You’re more likely to have seen an academic hospital workflow already.
One surgical attending summed it up this way in a debrief:
“The MD kids show up acting like small attendings. The DO kids show up acting like senior medical students. I can work with both, but the ones who realize how much they don’t know win.”
You need to understand: that’s the battle you’re fighting. Not DO vs MD. Humility vs insecurity. Performance vs posture.
The OMM Factor: What They Actually Think About It
Let’s deal with the sacred cow.
Most non-DO faculty don’t know what to do with OMM. They’ll say things like:
- “Do they still teach you guys manipulation?”
- “Can you use your DO stuff for this patient’s back pain?”
- “I don’t really use OMM but I support it in theory.”
Behind the scenes, the sentiment is usually:
- Neutral-to-mildly-positive in primary care, family medicine, PM&R.
- Mildly dismissive in high-acuity fields like surgery, EM, ICU.
- Highly variable based on personal exposure to competent DOs using it well.
Faculty almost never assume:
“DO student = better at physical exam.”
They assume:
“DO student = has extra tools I may or may not value.”
If you walk in trying to “prove OMM is real” on day one, you’ll set off all their alarms. If you quietly demonstrate that you understand anatomy cold, your exam is methodical, and you can explain why you believe a patient’s pain is mechanical vs. visceral—suddenly the DO label works in your favor.
What impresses them isn’t doing a rib raising technique. It’s this:
- You tie your exam maneuvers to anatomy and pathophysiology.
- You can explain musculoskeletal pain logically.
- You don’t abandon standard-of-care medicine to push manipulation as magic.
Use OMM as a subtext to signal, “I think deeply about structure and function,” not as a party trick.
Where DO Students Get Undervalued (And How To Flip It)
Here are the three recurring pain points I’ve seen for DO students on day one.
1. Knowledge Signaling
Faculty may assume, fairly or not, that your basic science or Step-style knowledge is uneven unless you’ve got a high Step 2 or COMLEX to back it up.
You don’t fix that by flexing obscure facts. You fix it by:
- Giving clean, structured presentations.
- Answering core questions clearly: “What are the three top causes of X in this population?”
- Admitting when you don’t know, then circling back the next day with a concise answer you read about.
When a DO student does that consistently, the quiet conversation changes from:
“Let’s see how they do on the shelf,”
to
“They overperformed our expectations.”
That matters when evals are written.
2. Self-Presentation
Too many DO students walk in with one of two bad stances:
- Apologetic: “I’m just a DO student from [school].”
- Defensive: Overcompensating, trying to out-argue everyone on every question.
Both are poison.
The students who destroy these biases walk in like this:
“I’m [Name], third-year medical student. I’m excited to learn as much as I can and help the team however you need.”
Neutral. Professional. No chip on the shoulder. No preemptive excuse. That disarms half the bias in the first 30 seconds.
3. Documentation and Workflow
This is where attendings quietly decide if you’re an asset or a burden.
Faculty assume MD and DO students are equally clueless about the EMR. The difference is what they expect next.
With DO students, some faculty subconsciously expect more “I wasn’t trained in that system.” With MDs, they may expect faster adaptation. Is that fair? No. But it’s there.
You counter that by being the person who:
- Asks once, writes things down, and doesn’t ask the same EMR question 5 times.
- Volunteers: “I can start that note,” or “I can put in that discharge summary draft.”
- Learns the admission template and uses it consistently and cleanly.
Once a DO student becomes “the reliable note person” on a team, the DO vs. MD lens comes off faster than you think.
How This Plays Out Across Specialties
The assumptions aren’t uniform. They shift by specialty.

| Category | Value |
|---|---|
| Family Med | 85 |
| Internal Med | 80 |
| Pediatrics | 78 |
| EM | 72 |
| General Surgery | 70 |
| Ortho | 68 |
| Psychiatry | 82 |
Treat these as rough “comfort levels” with DO students, not hard numbers.
Primary Care (FM, IM, Peds)
These attendings often work with DOs regularly. Many are DOs themselves.
Assumptions:
- DO and MD students will be similar at patient interaction.
- DO students may even be expected to excel in rapport-building.
- Academic MD schools might be pegged as a little more “research-talk, less bedside” early on.
You can dominate these rotations as a DO by leaning into patient communication, but you’d better not flounder on bread-and-butter medicine or prescribing.
EM and Surgery
Here’s where the DO vs. MD thing shows up more strongly, mainly because of board score and competitiveness history.
Unspoken assumptions:
- MD students, especially from big-name schools, are presumed to have seen high-acuity environments earlier.
- DO students are a question mark: “Are they gunning for this field or just rotating through?”
- Everyone is assumed to be clumsy with procedures; nobody expects you to be slick on day one.
If you’re a DO interested in these fields, they’re testing something very specific: can you handle stress and feedback without folding or posturing?
I’ve seen DO students go from “Who is this?” to “We should interview this person” in a week by:
- Showing up early, staying late.
- Asking to observe every procedure, then to assist, then eventually to try under close supervision.
- Owning their weaknesses without whining: “I haven’t done this before, but I watched X do it and I read about the steps.”
What Premeds and Early Med Students Get Wrong
You’re in the “PREMED AND MEDICAL SCHOOL PREPARATION” phase. Here’s where most of you are badly miscalibrated.
You obsess over:
- Ranking lists
- Match rate charts
- “Prestige”
Faculty obsess over:
- How you act at 4:30 a.m. on rounds when you’re tired
- Whether patients trust you when you walk in
- Whether your notes are safe, clear, and not a liability
- Whether you respond to feedback or argue with it
You think DO vs MD will dictate everything about your clinical life. It won’t. What it will dictate is:
- Your default assumptions on day one
- The level of proof you need to be taken seriously in competitive fields or big-name academic centers
- How closely your attendings watch your knowledge base early
As a premed or early med student, the strategic response isn’t to panic. It’s to prepare in a very specific way:
If You’re Considering DO vs MD
Ask yourself:
- Can you handle walking in with something to prove—but without being defensive?
- Are you willing to overprepare clinically and academically to shut down lazy assumptions?
- Do you understand that letters matter less after your first strong rotation eval than you think?
If yes, you’ll be fine at either. If you know you bruise easily from subtle bias, you should factor that in honestly.
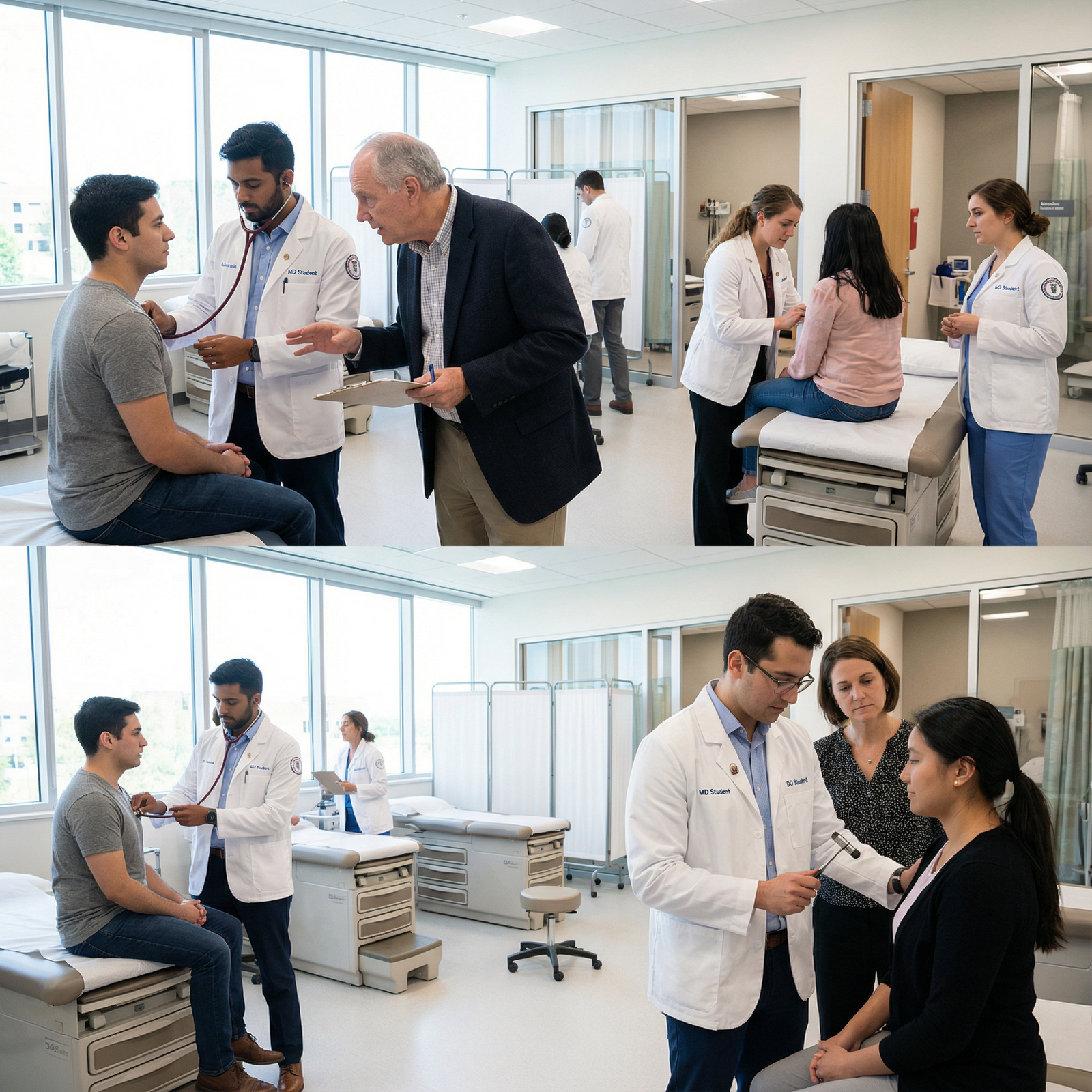
If You’re Already Matriculated (DO or MD)
Your priorities before clinicals:
- Master basic physical exam sequences until they’re muscle memory.
- Practice 2-3 minute, structured case presentations out loud.
- Read actual admission and progress notes so the format isn’t foreign.
- Learn how to look patients in the eye, introduce yourself clearly, and not mumble through your role.
If you show up able to function as a semi-useful human on the team, the DO vs MD story fades fast.
The Part Nobody Tells You: Redemption Is Fast
Here’s the good news.
Faculty are lazy in their assumptions, but they’re also quick to update based on reality. I’ve watched this happen hundreds of times:
Day 1:
“Okay, DO from [X school], we’ll see.”
Day 3:
“She gave a clean, concise presentation and picked up on a physical exam finding the intern missed.”
Week 2:
“Honestly one of our top students this year. Write her a strong eval.”
By the time you’re a week into a rotation, most attendings do not care anymore that you’re DO vs MD. They care that you:
- Don’t scare them
- Don’t create extra work
- Make patients feel safe
- Learn quickly and own your growth
If you’re DO, your job is simple: compress that timeline. Make them forget their assumptions faster.
If you’re MD, your job is not to coast on those assumptions. Nothing sours faculty faster than “strong test score, lazy on the floor.”

| Period | Event |
|---|---|
| Week 1 - Day 1 | Initial bias based on DO vs MD, school name |
| Week 1 - Day 3 | First impressions from presentations and exam skills |
| Week 2 - Day 8 | Pattern recognition of work ethic and reliability |
| Week 2 - Day 12 | Trust level for independent tasks |
| End of Rotation - Day 20 | Final eval driven by performance, not degree letters |
FAQs
1. As a premed, will choosing DO over MD permanently label me as “less skilled” clinically?
No. It will label you as someone faculty initially wonder about more in terms of knowledge and competitiveness. Clinically, everyone is assumed to be green on day one. Your real label comes from your first few clerkship evals, not your degree. What you do those first two rotations matters more than what’s printed on your diploma.
2. Do attendings actually know or care which schools are DO vs MD?
They know more than you think. They track patterns: “We’ve had good students from [X COM], weaker ones from [Y school].” The DO vs MD distinction is just one layer. A DO from a strong, consistent school can outrank an MD from a weak or unknown program in their mind very quickly once they’ve worked with a few of each.
3. Should I bring up OMM/OMT on day one as a DO student to show my ‘extra’ skills?
Usually no. That’s a rookie move. Show you can do a standard, rock-solid exam first. Once you’ve proven you’re safe, teachable, and not trying to convert anyone, you can selectively offer OMM in appropriate cases—especially if your attending is open to it. Let them see your clinical reasoning before your manipulation skills.
4. If I’m an MD student, do faculty automatically think I’m better prepared clinically?
Not clinically. Academically, maybe, depending on your school. But I’ve seen MD students from big-name schools look absolutely lost in clinic while a DO student runs circles around them with patient interaction and notes. Faculty care about who is useful and safe on their team now. Your degree only buys you a very short grace period.
5. What’s the smartest way to prepare during preclinical years so I crush day one, regardless of DO or MD?
Study how real medicine looks, not just what’s in First Aid. Watch or read sample case presentations. Practice them out loud. Learn a basic, reproducible approach to H&P that you can perform half-asleep. Spend a little time shadowing on wards to see the flow. If you can walk in already able to present a simple pneumonia case without rambling, examine a patient without skipping half the systems, and write a halfway decent note, you’ll instantly rise above the noise—DO or MD.
Key points: Faculty don’t walk in thinking “DO = bad, MD = good.” They walk in with lazy, experience-driven shortcuts about your likely knowledge and competitiveness, and they update those fast when you prove them wrong. On day one, what matters most isn’t the letters after your name. It’s whether you show up as safe, teachable, organized, and willing to work—because that’s what they actually remember when they write your eval.




















