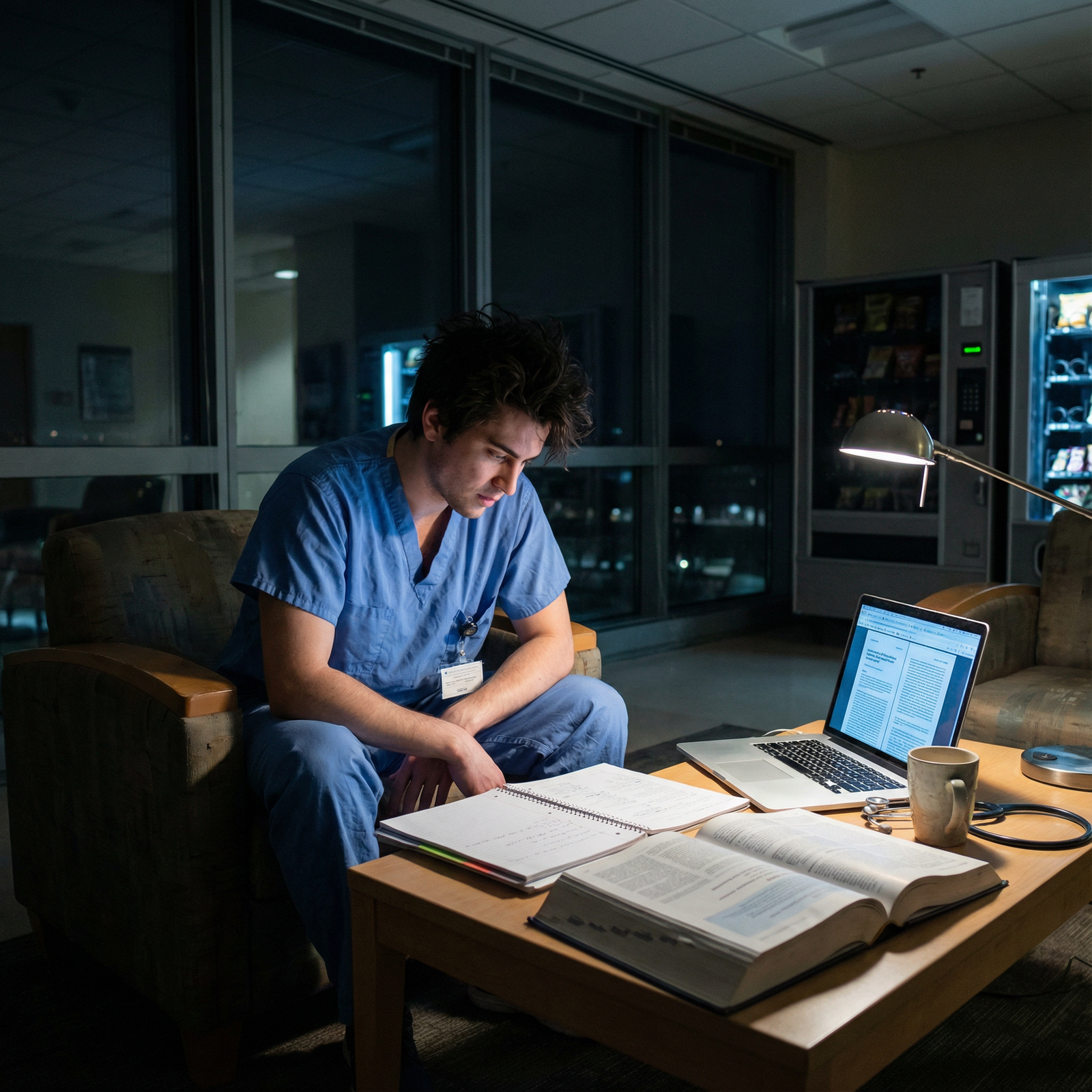
It is 2:47 a.m. on your third night of float. Your eyes burn. The telemetry pager has gone off seven times in the last ten minutes. You are staring at a potassium order you meant to sign, but you cannot remember if you already placed it… or just thought about placing it. A nurse is on the phone saying, “Doctor, what is the plan?” and you realize you do not have one. You are not “just tired.” You are cognitively unsafe.
This is where new interns get hurt. Or hurt someone else.
Night float is not about being heroic or proving you can “push through.” It is about not making the same predictable, preventable fatigue mistakes that every single intern is at high risk for.
Let me walk you through the big ones. The ones I have seen. The ones that actually lead to patient harm, bad evaluations, and near-misses that haunt people for years.
Mistake #1: Treating Night Float Like a Normal Day… Just Shifted
The first dangerous assumption: “I will just flip my schedule and live like it is daytime at night.”
No. You will not. And if you try to live like it is normal, you will end up:
- Sleep-deprived by night 2–3
- Making basic cognitive errors
- Snapping at nurses and co-residents
- Missing subtle but important clinical changes
The human body does not care that your schedule flipped. Your circadian rhythm is still wired to be asleep at 3 a.m., no matter how dedicated you think you are.
Common sub-mistakes here
Not protecting pre-shift sleep
New interns do this constantly:- Stay up doing life tasks
- Scroll on their phone
- “Just finish these notes” from the day
Then they walk into night #1 already 3–5 hours behind on sleep.
Drinking caffeine at the wrong time
Chugging coffee or an energy drink at 4–5 a.m. to survive sign-out is how you guarantee you will not sleep when you get home. By night 3, you are wrecked.Trying to “stay normal” on days off
Big rookie move: you flip back toward a day schedule on your golden day off (“I miss sunlight”). Then you slam yourself with another circadian reset when you go back onto nights. You never stabilize, so you stay in a half-jet-lagged state the entire rotation.

| Category | Value |
|---|---|
| Night 1 | 30 |
| Night 2 | 55 |
| Night 3 | 75 |
| Night 4 | 85 |
| Night 5 | 90 |
(I am assigning arbitrary “fatigue risk” numbers here, but you get the point: the risk spikes if you do not plan for it.)
How to avoid this
Do not “hope” your body will adapt. Build structure:
Before Night 1
- Sleep 3–4 hours in the late afternoon/evening (2–6 p.m. nap, blackout curtains, phone off).
- Light caffeine early in the shift only (before ~1–2 a.m.).
During Nights
- Keep caffeine front-loaded (start of shift, maybe mid-shift; nothing in the last 4–5 hours).
- Use bright light in the workroom early; dim your phone screen and room lights toward the end.
On Your Day Off
- Do not fully flip back. Shift halfway:
- Wake around noon–1 p.m.
- Sleep closer to 2–3 a.m., not 10 p.m.
- You will feel off, but less destroyed when you go back to nights.
- Do not fully flip back. Shift halfway:
Trying to live “normally” during a night float block is how you end up dangerously abnormal when it matters.
Mistake #2: Overestimating Your Brain at 3 A.M.
Here is a harsh truth: you are not smart at 3 a.m. You are not sharp. You are not at your “I got a 260 on Step” level.
You are slower. More impulsive. Worse at math. Worse at risk assessment. And much more likely to anchor on the first explanation that fits.
The mistake is pretending you are functioning at full capacity and making solo decisions that your 2 p.m. brain would never sign off on.
Classic fatigue errors I have watched interns make
Anchoring on the first story
“Oh, he is always short of breath, this is probably baseline,” instead of reassessing when vitals worsen.Medication errors
- Wrong decimal on an insulin sliding scale.
- Giving a med that was already given.
- Renewing a home med that was intentionally held.
Lazy differentials
- “It is probably anxiety” in a tachycardic, diaphoretic patient with chest pain.
- “They are just delirious” without considering sepsis, hypoxia, or withdrawal.
Skipping the chart review
This one is brutal at night. The intern reads the latest progress note only, ignores old cath reports, echo results, previous ICU stays, and makes a completely context-free decision.
Tools to protect your 3 a.m. brain
You will never be as sharp at 3 a.m. as 3 p.m. Accept it. Then build systems to compensate:
Use checklists for common situations:
- Acute chest pain
- New hypoxia
- Altered mental status
- Fever in an inpatient
Force a 30-second pause before major orders:
- ICU transfer
- Rapid transfusions
- Narcotic dose increases Ask yourself: “What am I missing that I would think of if it were 2 in the afternoon?”
Phone a friend early
Text your senior: “Can I run a quick situation by you?”
That is not weakness. It is what people who do not make big mistakes do.
Mistake #3: Letting Shame Stop You from Asking for Help
This one hits hard for new interns. You are terrified of being “the weak one” on nights. So you:
- Do not call your senior for a borderline unstable patient
- Try to manage a crashing patient alone for 10–15 minutes
- Fudge your level of concern when talking to the night attending
- Stay quiet in radiology or the ED when you do not understand what is happening
I have stood in a room where a new intern did chest compressions for almost 2 minutes on someone who had a DNR order clearly in the chart, because they were too embarrassed to say, “I do not know their code status,” in front of the nurse and respiratory therapist.
Fatigue + shame = dangerous.
Red flags you are letting shame run your night
- You think “They are busy, I should not bother them” before calling your senior about:
- New ST depressions
- Rising lactate
- Increasing pressor needs
- You rephrase your concern softer than it is:
- Saying “they look a bit off” instead of “I am worried they are decompensating.”
- You delay calling a rapid because “the attending will see it” and you want to avoid that spotlight.
Safer behavior patterns
You need some hard rules for yourself:
If you are thinking “should I call?” — you call.
Full stop. Fatigued brains undercall problems. Your threshold must be embarrassingly low.Make your uncertainty explicit.
Say: “I am not sure what is going on, but I am worried because X, Y, Z.”
That invites help. It signals the level of urgency.Use strong language when appropriate.
Nurses escalate faster when they hear you are genuinely concerned.- Not: “Let me know if it gets worse.”
- Try: “I am concerned. If X happens again, please call me immediately and I will see them at bedside.”
You are not there to impress people with how independently you can drown. You are there to keep patients alive and yourself out of the disaster zone.
Mistake #4: Sloppy Hand-offs That Blow Up Overnight
Terrible sign-outs are a root cause of so many night float disasters.
You know the moment: you get a “sign-out” at 7 p.m. that reads, “Stable, nothing to do,” and then at 1 a.m. you find out this “stable” patient came from the ICU yesterday, is on 6L nasal cannula, had a troponin bump, and the day team was “watching them.” Except they did not tell you that. You are now behind.
As a night float intern, you are also giving sign-out to others. Sloppily. When you are exhausted.
Common hand-off mistakes that night interns make
No clear “if-then” plans
“Watch vitals” is not a plan.
“If RR > 24 or sats < 92 on 2L, please call and I will evaluate,” is.Burying the real concern
Saying “just following up labs” when that lab is a critical potassium you are praying does not come back 2.3 at 3 a.m.Not flagging time-sensitive tasks
- Antibiotics that must be given before midnight
- Time-limited neuro checks
- Re-draw after transfusion
No clarity on limits of care
- Not mentioning DNR/DNI
- Not specifying no ICU escalation per family discussion
Now your night decisions may be completely misaligned with patient and family values.
| Situation | Dangerous Phrase | Safer Phrase with Actionable Plan |
|---|---|---|
| Borderline hypoxia | "Satting low 90s, just watch" | "On 4L, if needs >6L or RR >24, call me" |
| New troponin bump | "Trop bumped, stable" | "Trop 0.08, repeat at 2 a.m., page with result" |
| High fall risk | "Confused, fall risk" | "Delirious, bed alarm on, call if trying to get out of bed" |
How to fix your own hand-offs
As night float, you do two kinds of hand-offs: incoming (what you receive) and outgoing (what you give). You cannot control others’ laziness, but you can control your side.
Minimum standard for a halfway decent sign-out:
One-sentence summary with trajectory.
- “72M, COPD, admitted for pneumonia, improving on day 3, on 2L O2, baselines at 3L at home.”
Top 2–3 active issues.
- “Issue 1: slow GI bleed, Hb trended 9.5 → 8.2, repeat at 3 a.m., call if <7.5.”
- “Issue 2: delirium, on sitter, no antipsychotics overnight without MD discussion.”
Explicit “if-then” safety plans.
Spell it out. Vitals, labs, behaviors that should trigger a call.
Anything less, and you are making it easier for your future exhausted self (or your co-intern) to miss something critical.
Mistake #5: Letting Physical Needs Collapse (Until You Are a Risk)
You will hear interns brag: “I did not sit down once all night.”
That is not heroic. It is stupid.
You are not a machine. You are a human with a brain that needs:
- Glucose
- Hydration
- Bathroom breaks
- A short mental reset
Deny all of that for 12 hours, then ask that same brain to:
- Calculate an anion gap correctly
- Recognize subtle early sepsis
- Catch a med interaction at 6 a.m.
You are setting yourself up to fail.
How this shows up on nights
- You ignore thirst, then spike a headache and brain fog around 4 a.m.
- You go 10 hours without peeing (common in new female interns) and end up with pelvic pain and UTIs mid-rotation.
- You start grabbing whatever is fastest: vending machine candy, stale pizza, energy drinks. Your glucose spikes and crashes, mood tanks, and you become irritable and sloppy.

| Category | Value |
|---|---|
| Well-rested | 10 |
| Mildly Dehydrated | 40 |
| Very Hungry | 45 |
| No Breaks 10+ hrs | 60 |
(Error risk % is illustrative, but the pattern is real.)
Minimal physical safety standards you should enforce for yourself
If you do nothing else, do this:
Hydration
Keep a water bottle at the workstation. Every time you sign an order, take a sip. Yes, it is that basic.Bathroom
Commit to one bathroom break every 3–4 hours. Tell the nurse, “I will be off the floor for 5 minutes. If something is truly emergent, call my pager twice.” That is what codes and emergency call systems are for.Food
Pack something that is not just sugar and caffeine:- Nuts or trail mix
- Protein snacks
- A real meal to eat early in the shift, not at 3 a.m.
You are not being self-indulgent. You are maintaining minimum operating conditions.
Mistake #6: Ignoring Micro-sleep and Fatigue Warning Signs
Here is where people get in real danger. Not just clinically. Personally.
Micro-sleeps are 1–10 second involuntary sleep episodes. They happen when you are severely exhausted. On nights, I have seen:
- Interns nod off standing up during cross-cover sign-out
- People fall asleep on the toilet
- Someone “blink” and wake up charting the wrong patient’s note
The worst: dozing off while driving home. More common than anyone wants to admit.
Early warning signs you are not just “tired,” you are unsafe
- Re-reading the same note or page three times and not absorbing it
- Forgetting what you were about to order right after clicking “New Order”
- Typing nonsense or half-words in your note (and not noticing)
- Missing obvious alarms or overhead pages that others react to
- Feeling like your vision is “blurring” when you stare at the screen
If you are here, you must stop pretending everything is fine.
What to do when you hit that wall
You cannot willpower your way out of this level of exhaustion. You need tactical moves:
Micro-break
5 minutes. Phone down. Step away from the screen. Splash cold water on your face. Breathe.
Tell the nurse you are doing this. They will understand. They see how bad nights get.Re-prioritize tasks
Stop trying to do low-yield busywork: non-urgent med recs, note formatting, perfect ROS. Focus on:- New pages and urgent issues
- Time-sensitive orders
- Safety checks
Buddy-check on dangerous tasks
If you are ordering something high-risk (heparin drip, chemo agents, weight-based peds meds) while feeling this level of fatigue, ask a senior or co-intern to sanity-check the order.
And if you are too exhausted to safely drive home, the correct move is not to “just tough it out.” That is how residents crash their cars. Sit in the call room. Set an alarm. Sleep 30–60 minutes. Then reevaluate driving. If your hospital has fatigue policies or cab vouchers, use them. That is what they are for.
Mistake #7: Letting Emotional Exhaustion Turn into Contempt
Night float does something to people. The loneliness, the reversals of day-night, the constant interruptions — it strips your usual patience.
A subtle but very dangerous shift happens: you start to see patients, and even nurses, as problems instead of people.
This is when I hear interns say things like:
- “It is just the frequent flyer calling again.”
- “She always says she is 10 out of 10 in pain, just ignore it.”
- “Can you ask the nurse not to page me about this stuff?”
At 3 p.m., you might handle that exact conversation with curiosity. At 3 a.m., you are more likely to dismiss it. And sometimes the “annoying” page is actually the only early warning you get.
Emotional fatigue red flags
- You roll your eyes internally every time you see certain room numbers on your pager.
- You talk yourself out of seeing a patient in person because “they always do this.”
- You feel irritated at the nurse before you even hear what they are saying.
- You catch yourself hoping nothing happens, more than hoping you catch problems early.
This is exactly when someone with “chronic pain” will actually have an acute abdomen. Or your “always delirious” patient will blow a pupil.
How to protect against this slide
You will not become a saint at 2 a.m. But you can impose a few non-negotiables:
Bedside rule for repeats
If a nurse pages twice about the same concern, you go see the patient. Even if you are convinced it is “nothing.”Language check
Ban certain phrases from your own mouth and notes:- “Frequent flyer”
- “Drug-seeking” (without a clear, documented pattern)
- “Just anxious” as the sole explanation for tachycardia or chest pain
Narrate what you are doing
When you are exhausted, saying out loud, “I am going to see them to make sure nothing bad is going on,” keeps your brain on the hook for actually looking.
You will still feel frustrated. That is fine. Just do not let that frustration make clinical decisions for you.
Mistake #8: Not Debriefing Bad Nights (and Repeating the Same Errors)
The last dangerous mistake is subtle. You survive the rotation. You are proud. So you do not look back.
You do not examine:
- The near-miss where you almost gave the wrong dose
- The delayed rapid call that still bothers you
- The pattern that you always forget to check something (tele, labs, imaging) at the end of your shift
You just push it all down and move on.
That is how people repeat the same fatigue mistakes year after year.
What a real debrief looks like
This does not need to be therapy. It can be 10–15 minutes after the block:
Identify 2–3 moments that felt bad or unsafe.
- “I almost fell asleep driving.”
- “I delayed seeing a patient who was actually sick.”
- “I ordered something without fully understanding the med.”
Ask: what was the upstream cause?
Not the symptom (fatigue), but the pattern:- No plan for naps or pre-night sleep?
- Shame about asking for help?
- Poor hand-off from day team that you did not push back on?
Create one specific change for the next block.
- “I will always ask about code status and document it clearly on my handoff list.”
- “If I think ‘should I call my senior?’ I will call.”
- “I will not drink caffeine after 2 a.m.”
Write it down. Literally. Put it in your notes app as “Night Float Lessons” and add to it each year.
Your Next Step (Do This Before Your First Night)
Do not wait until you are delirious at 3 a.m. to think about these things.
Today, do one concrete thing to reduce your risk of dangerous fatigue mistakes:
Open your notes app and create a simple “Night Float Safety Plan” with three headings:
Sleep & Caffeine Rules
- When you will nap pre-shift
- When you will cut off caffeine
Call-Your-Senior Triggers
- A short list of situations where you will always call, no matter how “small” they seem (new chest pain, rising O2 needs, repeat pages, your gut feeling that “something is wrong”).
Non-Negotiable Breaks
- How often you will drink water, eat, and step away from the screen.
Write it now. Not later. Because later will be 2:47 a.m., on your third night of float, with a ringing pager and a brain that cannot be trusted to improvise safely.



















