The way most MCAT students “learn” hormone pathways virtually guarantees they will forget them on test day.
Let me be direct: if you cannot draw the core endocrine feedback loops from memory, you do not know them well enough for the MCAT.
This exam does not reward vague recall like “uh, cortisol is from the adrenal cortex somewhere.” It punishes it. The test writers love hormones because they can hit every level at once: anatomy, physiology, feedback control, pharmacology, even experimental design. Hormone passages are where sloppy memorizers get exposed.
I will walk you through the endocrine pathways that actually matter, how the MCAT likes to twist them, and how to build a mental “map” that you can reconstruct under pressure.
The MCAT Endocrine Mindset: Systems, Not Flashcards
Stop thinking “memorize hormones.” Start thinking “control systems and nodes.”
Every high-yield hormone question is basically testing three things:
- Where the hormone comes from (source gland or tissue)
- What stimulates or inhibits its release (upstream signal, feedback)
- What it does and how the system compensates if something changes
You need to see these as modular circuits. Hypothalamus → pituitary → target gland → target hormone → effect → negative feedback.
If you can visualize that generic template, you just swap labels:
- CRH → ACTH → adrenal cortex → cortisol
- TRH → TSH → thyroid → T3/T4
- GnRH → LH/FSH → gonads → sex steroids
Let us nail the “core loops” first, then layer on the tricky exceptions.
The Big Three Hypothalamic–Pituitary–End Organ Axes
These three show up constantly in passages, especially with pathology or drug questions.
1. HPA Axis: Stress and Cortisol
You must know this one cold.
Baseline loop:
- Hypothalamus: Corticotropin-releasing hormone (CRH)
- Anterior pituitary: Adrenocorticotropic hormone (ACTH)
- Adrenal cortex (zona fasciculata): Cortisol
Cortisol then exerts negative feedback on:
- Hypothalamus (↓ CRH)
- Anterior pituitary (↓ ACTH)
Now the MCAT games begin when something breaks in this loop.

| Step | Description |
|---|---|
| Step 1 | Hypothalamus\nCRH |
| Step 2 | Anterior Pituitary\nACTH |
| Step 3 | Adrenal Cortex\nCortisol |
Classic MCAT pathologies:
Primary adrenal insufficiency (Addison disease)
Target gland failure: adrenal cortex cannot make cortisol.- Cortisol: low
- ACTH: high (no feedback)
- CRH: high
Symptoms they like: hyperpigmentation (high ACTH → melanocyte-stimulating effect), hypotension, salt craving, hyperkalemia (since aldosterone often low too).
Secondary adrenal insufficiency (pituitary problem)
Pituitary cannot secrete ACTH.- ACTH: low
- Cortisol: low
- CRH: high (hypothalamus keeps trying)
Hyperpigmentation is typically absent (ACTH is low).
Cushing syndrome (excess cortisol)
Causes:- Exogenous steroids (most common real world)
- Adrenal tumor (primary)
- Pituitary ACTH-secreting tumor (Cushing disease, secondary)
- Ectopic ACTH (e.g., small cell lung carcinoma)
Lab patterns:
- Primary adrenal tumor: high cortisol, low ACTH, low CRH
- Pituitary tumor (Cushing disease): high ACTH, high cortisol, low CRH
MCAT-style question: They give EITHER ACTH and cortisol levels or describe a dexamethasone suppression test and ask you to localize the lesion. You do not need Step 1-level nuance, just the concept:
- Remove cortisol → ACTH goes up (if pituitary intact).
- Add cortisol (or steroid) → ACTH goes down (if feedback works).
If feedback does not change ACTH, the problem is at the tumor source.
Map this out at least 5 times from memory until you can see the pattern without effort.
2. HPT Axis: Thyroid Regulation and Metabolism
Second workhorse axis: metabolism and growth.
Baseline loop:
- Hypothalamus: Thyrotropin-releasing hormone (TRH)
- Anterior pituitary: Thyroid-stimulating hormone (TSH)
- Thyroid: T3 (triiodothyronine) and T4 (thyroxine)
T3/T4 exert negative feedback on:
- Hypothalamus (↓ TRH)
- Anterior pituitary (↓ TSH)
Production nuance: thyroid mainly secretes T4; T3 is more active and produced by peripheral conversion. Free hormone fraction is active; most is protein-bound (thyroxine-binding globulin).
Common test themes:
Primary hyperthyroidism (problem in thyroid itself)
- Graves disease (autoantibody stimulates TSH receptor)
Labs: - T3/T4: high
- TSH: low
- TRH: low
- Graves disease (autoantibody stimulates TSH receptor)
Primary hypothyroidism (e.g., Hashimoto thyroiditis, iodine deficiency)
- T3/T4: low
- TSH: high
- TRH: high
Secondary hypothyroidism (pituitary failure)
- TSH: low
- T3/T4: low
- TRH: high
MCAT loves this pattern: target hormone low, upstream stimulating hormone high = primary gland failure. Target hormone low, upstream hormone low = central (pituitary or hypothalamus) problem.
They also like pregnancy and oral contraceptives: increased thyroid-binding globulin (TBG) → total T4 up, but free T4 and TSH normal. Clinical euthyroid. If you panic at “increased T4” without looking at TSH, you miss the question.
Your mental rule: TSH is the most sensitive indicator of thyroid status. If free hormone is off, TRH/TSH respond in the opposite direction.
3. HPG Axis: Reproduction and Sex Steroids
This one is more variable across sexes and age, but the template holds.
Baseline loop:
- Hypothalamus: Gonadotropin-releasing hormone (GnRH), usually pulsatile
- Anterior pituitary: Luteinizing hormone (LH) and follicle-stimulating hormone (FSH)
- Gonads:
- Testes: testosterone, inhibin B (Sertoli), androgen-binding protein
- Ovaries: estrogen, progesterone, inhibin
Sex steroids give negative feedback to:
- Hypothalamus (↓ GnRH)
- Anterior pituitary (↓ LH/FSH)
Important MCAT details:
- Continuous GnRH → suppresses LH and FSH (used clinically with GnRH agonists in prostate cancer, endometriosis).
- Pulsatile GnRH → stimulates normal LH/FSH release.
Male example:
- High-dose exogenous testosterone:
- ↑ serum testosterone; ↓ GnRH, ↓ LH
- Testicular atrophy and ↓ endogenous testosterone production
- ↓ spermatogenesis (low intratesticular testosterone and FSH stimulus on Sertoli cells)
Female example they love: combined oral contraceptive pills (OCPs)
- Contain estrogen + progestin
- Maintain relatively constant levels of these → suppress GnRH, LH, and FSH
- Without LH surge, no ovulation.
MCAT question pattern:
“A researcher administers a GnRH agonist via continuous infusion. What happens to LH and testosterone levels after several weeks?”
Correct: both fall due to downregulation of pituitary GnRH receptors.
These are not random facts. They are just manipulated feedback loops.
Pituitary Hormones: Anterior vs Posterior and Their Controls
You should be able to mentally split the pituitary into two lobes with distinct rules.
Anterior Pituitary (Adenohypophysis)
Derived from oral ectoderm (Rathke pouch). Controlled mainly by hypothalamic releasing/inhibiting hormones via the hypophyseal portal system.
Key anterior pituitary hormones:
- TSH
- ACTH
- LH
- FSH
- Prolactin
- Growth hormone (GH)
Everyone memorizes, few understand their regulation. Let me break down the quirks.
Prolactin – the Inhibition Exception
Prolactin is weird. Its baseline default is “on,” but it is chronically held in check by hypothalamic dopamine (prolactin-inhibiting factor).
Regulation:
- Hypothalamus: dopamine (↓ prolactin); TRH (↑ prolactin, minor role)
- Anterior pituitary: prolactin
- Target: mammary glands → lactation
Feedback:
- Prolactin increases hypothalamic dopamine → negative feedback on itself.
Clinical/MCAT patterns:
Dopamine antagonists (e.g., antipsychotics like haloperidol, risperidone)
↓ dopamine effect → ↑ prolactin → galactorrhea, amenorrhea.Pituitary stalk damage (e.g., craniopharyngioma)
Dopamine cannot reach anterior pituitary → disinhibited prolactin secretion.Hypothyroidism
↑ TRH (trying to stimulate TSH) also mildly ↑ prolactin.
So if they say: “A patient on antipsychotics has milky nipple discharge and infertility,” you should immediately think: dopamine blocked → prolactin up → GnRH suppressed → ↓ LH/FSH → hypogonadism.
This is a network, not isolated facts.
Growth Hormone (GH) – Pulsatile and Sleep-Linked
Regulation:
- Hypothalamus:
- Growth hormone–releasing hormone (GHRH) → ↑ GH
- Somatostatin → ↓ GH
- Anterior pituitary: GH
- Target: liver (IGF-1/ somatomedin C production), bone, muscle
Feedback:
- IGF-1 and GH both feed back to inhibit GHRH and GH release.
Stimuli that increase GH:
- Sleep (especially deep sleep)
- Exercise, stress
- Hypoglycemia
- Fasting
Stimuli that decrease GH:
- Hyperglycemia
- Obesity
- Elevated IGF-1 (acromegaly/gigantism state)
MCAT loves dynamic tests: give glucose → GH should go down. If not, suspect acromegaly.
Again: think “what would this do to the loop?”
Posterior Pituitary (Neurohypophysis)
Derived from neural tissue (diencephalon). It does not synthesize hormones. It just stores and releases them.
Hormones made in hypothalamus, transported down axons:
- ADH (vasopressin) – made in supraoptic nucleus
- Oxytocin – made in paraventricular nucleus
Both are released from posterior pituitary into systemic circulation.
MCAT is obsessed with ADH.
ADH and Water Balance: Osmoregulation and Blood Pressure
If you only master one standalone hormone for the MCAT, make it ADH.
Function: Conserve water.
- Receptor V2 (kidney): inserts aquaporin-2 channels in collecting duct → ↑ water reabsorption → concentrated urine.
- Receptor V1 (vascular smooth muscle): vasoconstriction at high levels.
Stimuli for ADH release:
- High plasma osmolality (most sensitive)
- Low blood volume or pressure (baroreceptors)
- Angiotensin II
Inhibitors of ADH:
- Alcohol (classically tested)
- Decreased plasma osmolality
Two high-yield pathologies:
Diabetes insipidus (DI)
- Central: low ADH secretion (e.g., pituitary damage)
- Nephrogenic: kidney unresponsive to ADH (e.g., lithium toxicity, hypercalcemia)
Features:
- Polyuria, polydipsia
- Dilute urine, high serum Na+ and osmolality
- Water deprivation test: with central DI, desmopressin (ADH analog) will concentrate urine. With nephrogenic DI, it will not.
SIADH (syndrome of inappropriate ADH)
- Too much ADH → water retention
- Hyponatremia, low serum osmolality, concentrated urine
- Usually euvolemic hyponatremia (mild volume expansion triggers natriuresis)
MCAT question pattern: They describe labs and ask “which hormone is elevated/depressed?” If urine is sharply concentrated in a hypovolemic patient, think high ADH.
Again, this is feedback: low volume or high osmolality → hypothalamus → more ADH → kidney retains water → osmolality normalizes → ADH falls.
Insulin, Glucagon, and Counterregulation
Different gland now, but same game: negative feedback around blood glucose.
Pancreatic Hormones
- β cells (islets of Langerhans): insulin
- α cells: glucagon
- δ cells: somatostatin
Insulin: secreted in response to high blood glucose, amino acids, incretins.
- Increases glucose uptake in muscle and adipose (GLUT4), glycogen synthesis, fat synthesis, protein synthesis.
- Decreases lipolysis and gluconeogenesis.
Glucagon: secreted in response to low blood glucose, high amino acids (especially after protein meal).
- Increases glycogenolysis, gluconeogenesis, lipolysis, ketone production.
Negative feedback is simple:
- High glucose → ↑ insulin → ↓ glucose → insulin falls.
- Low glucose → ↑ glucagon → ↑ glucose → glucagon falls.
MCAT sometimes mixes this with stress hormones:
- Epinephrine (from adrenal medulla) and cortisol also increase blood glucose.
- Prolonged stress → sustained cortisol → muscle breakdown, hyperglycemia.
They love experimental setups where they block insulin receptors or remove the pancreas and watch what happens to blood glucose, lipolysis, or ketones. If insulin is low or ineffective, everything catabolic goes up.
Calcium Homeostasis: PTH, Vitamin D, and Calcitonin
This is another self-contained feedback system the MCAT likes.
Primary controller: parathyroid hormone (PTH).
PTH Loop
Stimulus: low serum Ca²⁺.
Parathyroid glands release PTH → actions:
- Bone: ↑ bone resorption (via osteoblasts stimulating osteoclasts) → ↑ Ca²⁺ and PO₄³⁻
- Kidney:
- ↑ Ca²⁺ reabsorption (distal tubule)
- ↓ PO₄³⁻ reabsorption (proximal tubule)
- ↑ 1α-hydroxylase activity → more active vitamin D (calcitriol)
Calcitriol (active vitamin D) then:
- ↑ Ca²⁺ and PO₄³⁻ absorption from gut
- Helps maintain mineralization (with Ca²⁺ and phosphate)
Feedback:
- Rising Ca²⁺ directly inhibits PTH secretion (via Ca-sensing receptors).
- Severe hypermagnesemia suppresses PTH; mild hypomagnesemia is like hypocalcemia and stimulates PTH.

| Category | Value |
|---|---|
| Low Ca | 90 |
| Normal Ca | 50 |
| High Ca | 10 |
Calcitonin (from thyroid C cells) is low-yield for the MCAT. It modestly lowers serum Ca²⁺ by inhibiting osteoclasts, but its physiologic role in humans is minor. If calcitonin does appear, it is more often in the context of medullary thyroid carcinoma (tumor marker) than a major regulatory hormone.
MCAT pattern: hyperparathyroidism from a parathyroid adenoma → high PTH, high Ca²⁺, low phosphate. Or chronic kidney disease → low vitamin D, hypocalcemia, secondary hyperparathyroidism.
Again, always loop back to the sensor (parathyroid glands) and main controlled variable (serum Ca²⁺).
Leptin, Ghrelin, and Other “MCAT Favorite” Hormones
The test occasionally dips into appetite and energy balance, usually in experimental passages.
Leptin: made by adipose tissue; signals satiety and energy sufficiency.
- More fat → more leptin → hypothalamus decreases appetite.
- Starvation, sleep deprivation → leptin drops → appetite increases.
Ghrelin: made mainly by stomach; signals hunger.
- ↑ before meals, ↓ after meals.
- Sleep deprivation → ↑ ghrelin.
This is a simple push-pull. They might show a graph where sleep-deprived subjects have elevated ghrelin, reduced leptin, and increased caloric intake.
Your job is to interpret the direction of change and map it back to feedback on hypothalamic appetite centers.
How the MCAT Actually Tests These Pathways
Let me show you the “moves” they like to use, so you can read endocrine passages with purpose.
1. Upstream vs Downstream Problems
They will describe:
- A lesion (tumor, infarct, trauma) at a specific structure
- A drug blocking a receptor or hormone
- A genetic knockout in an animal model
Then ask: what happens to hormone X, Y, Z?
You must:
- Identify whether the manipulation is upstream or downstream.
- Apply negative feedback logic.
Example: “A patient receives long-term high-dose exogenous glucocorticoids.”
- Exogenous cortisol high → inhibits CRH and ACTH → adrenal cortex atrophies → endogenous cortisol production decreases.
- If drugs suddenly stopped → acute adrenal crisis (cannot quickly restore cortisol).
You should immediately see that ACTH will be low in this chronic setting.
2. Axis vs Isolated Hormone Thinking
Lazy thinking: “Low cortisol = bad.”
MCAT thinking: “Low cortisol → what happens to ACTH, CRH, glucose, blood pressure, immune function?”
They want layered predictions, like:
- “Which other hormone will likely be elevated?”
- “What symptom best explains the elevated ACTH?”
- “Which lab value differentiates primary vs secondary failure?”
If you memorize cortisol but not its loop partners, you will struggle.
3. Dynamic Tests and Stimuli
The MCAT loves scenarios where a stimulus is applied and you must know the direction of hormone change.
Examples:
- Glucose infusion and GH / insulin behavior.
- Water deprivation and ADH / urine osmolality.
- TRH administration and TSH / prolactin in pituitary damage.
- GnRH agonist continuous infusion and LH/FSH in prostate cancer.
You do not need exact numbers. You just need to know:
- Stimulus → normal response vs blunted/absent response when part of the axis is broken.
How to Actually Study Hormone Pathways (Not Just Read About Them)
You cannot “passive review” your way into mastering this. You must externalize the loops.
Here is the approach that works:
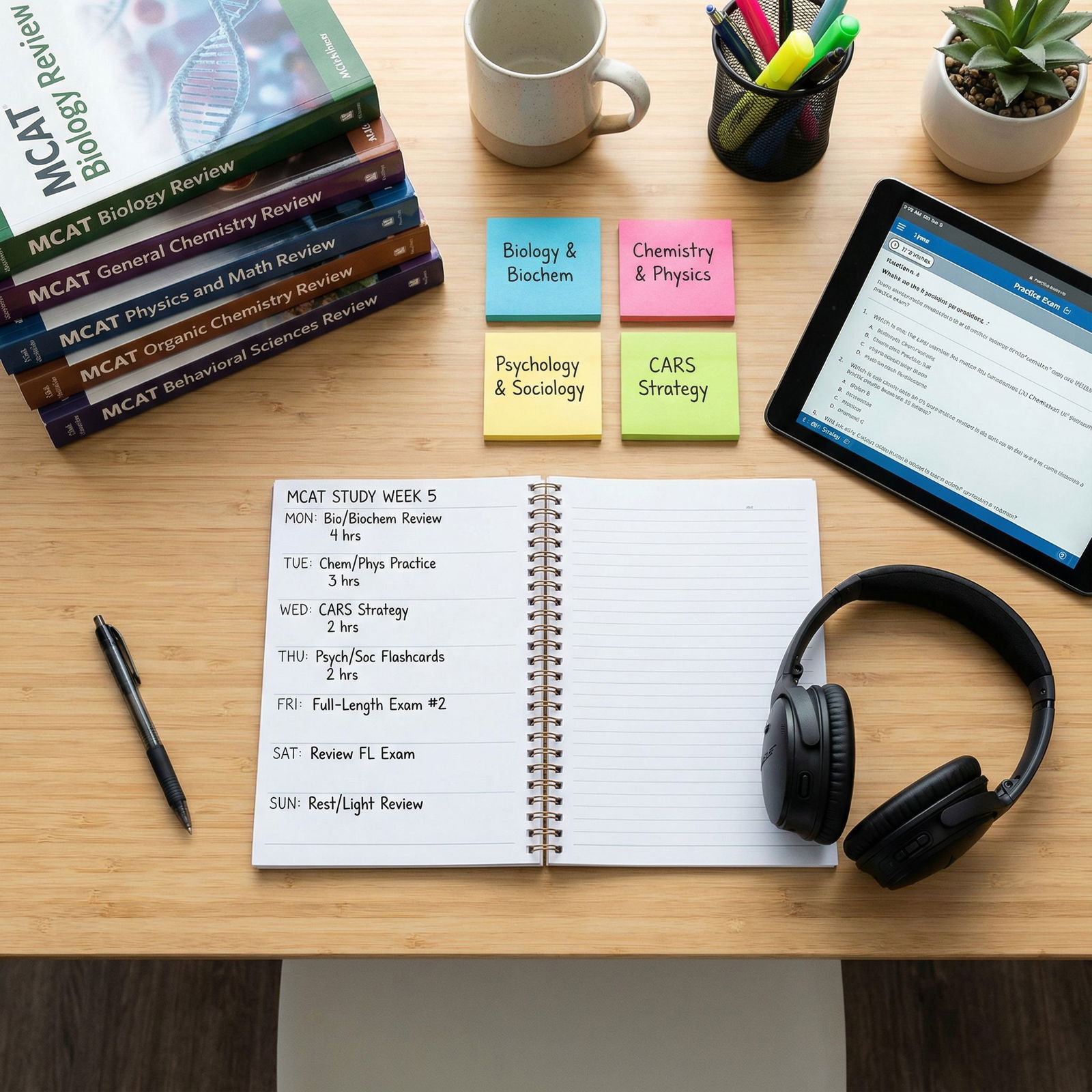
Pick one axis at a time
HPA, HPT, HPG, ADH, insulin/glucagon, PTH.Draw it from memory
No notes, no peeking. Hypothalamus at top, pituitary (if applicable), target gland, target hormone, feedback arrows.Annotate stimuli and inhibitors
Next to each node, write 2–3 major things that increase or decrease that hormone. Example for ADH: high osmolality, low volume, angiotensin II vs alcohol.Create 3 pathological or drug scenarios per axis
For each:- Identify the lesion or drug action.
- Predict all hormone levels in the axis (upstream and downstream).
- Then add 1–2 clinical consequences (e.g., hyperpigmentation, hyponatremia).
Check against a reliable source
Anki, Kaplan, BC notes, or a good review book. Correct, redraw, repeat.Do targeted questions
Use UWorld, AAMC Section Bank, or other high-quality question banks. Flag every endocrine question where you miss a hormone level or feedback direction and immediately redraw that loop.
If you want a quick “daily loop drill,” rotate like this:
| Day | Axes to Practice |
|---|---|
| 1 | HPA, HPT |
| 2 | HPG, Prolactin/GH |
| 3 | ADH, Insulin/Glucagon, PTH |
Each day, pick 2–3 axes, draw them from scratch, and generate a few “what if X fails?” scenarios. Ten minutes, max. The repetition is what sticks.
Visual Tools To Keep These Straight
Some people are visual learners but they try to cram hormones as text. Not efficient.
Use:
Color-coded arrows
Green = stimulation; red = inhibition. Draw the hypothalamus in one color, pituitary in another, target glands in a third.Consistent layout
Always put hypothalamus at the top, pituitary in the middle, end organs at the bottom. Same orientation every time. Your brain will build a template.Side annotations
Along the side of each axis, list 2–3 key diseases and 1 key drug that hit that axis. It makes the networks more concrete.
Here is a simple conceptual flow for how a typical MCAT endocrine passage plays out if you understand pathways:

| Step | Description |
|---|---|
| Step 1 | Read scenario |
| Step 2 | Identify primary variable\n(hormone, gland, drug) |
| Step 3 | Map to known axis\n(HPA, HPT, HPG, etc.) |
| Step 4 | Locate level of disturbance\n(hypothalamus, pituitary, gland, receptor) |
| Step 5 | Apply feedback rules\npredict up/down changes |
| Step 6 | Match predictions\nto answer options |
You are not “guessing hormones.” You are just running a well-practiced algorithm.
A Quick Reality Check With MCAT-Style Data
Just to anchor this: endocrine content is not fringe. A substantial chunk of Bio/Biochem and Psych/Soc passages are hormone-heavy, often wrapped in experimental clothes.

| Category | Value |
|---|---|
| Bio/Biochem questions with hormone content | 25 |
| Psych/Soc questions with hormone content | 10 |
| Other questions | 65 |
Those are rough, but they match what I see when students bring me AAMC practice data. If your endocrine reasoning is weak, you are handicapping yourself on 30–40% of the exam’s reasoning-based biology.
Bringing It Together On Test Day
Let me give you a concrete scenario and how you should think:
“Researchers remove the pituitary gland from rats. They then infuse synthetic cortisol at a constant low dose. Compared to normal rats, what will be the levels of CRH and endogenous cortisol?”
You should mentally run:
- No pituitary → no ACTH → no endogenous adrenal stimulation → endogenous cortisol low.
- Exogenous cortisol (even low) provides some negative feedback → CRH will be lower than in a pure pituitary ablation without replacement, but likely not zero.
- Endogenous cortisol: low.
- Total cortisol: near normal (because of infusion).
They may just be testing that you understand the difference between endogenous vs exogenous sources and that the hypothalamus responds to serum hormone, not “source origin.”
Or:
“A patient with a TSH-secreting pituitary adenoma has which pattern of lab findings?”
- TSH: high (tumor)
- T3/T4: high
- TRH: low (feedback from high thyroid hormones)
- If you removed the pituitary adenoma surgically, T3/T4 would fall, TSH would normalize, and TRH would recover over time.
If you can verbalize that in your head, you can answer 90% of endocrine pathway questions.
One Last Point About Overstudying
You do not need every obscure hormone or rare disease. Do not sink hours into calcitonin or GIP or VIP or obscure hypothalamic peptides unless you have already mastered:
- HPA, HPT, HPG axes
- Prolactin and GH regulation
- ADH and water balance
- Insulin/glucagon and counterregulation
- PTH/vitamin D and calcium balance
- Leptin/ghrelin basics
Once those are automatic, sure, add polish. But most students fail the MCAT endocrine section not because it is “hard,” but because they spread themselves thin over trivia and never built rock-solid loops for the big systems.



| Category | Value |
|---|---|
| HPA/HPT/HPG Axes | 40 |
| ADH & Water Balance | 20 |
| Insulin & Glucagon | 15 |
| PTH & Calcium | 10 |
| Appetite Hormones | 10 |
| Low-Yield Misc. Hormones | 5 |
Key Takeaways
- Think in axes and feedback loops, not isolated hormones. If you can draw HPA, HPT, HPG, ADH, insulin/glucagon, and PTH loops from memory, you are ahead of most test-takers.
- MCAT endocrine questions almost always reduce to: “What is the level of disturbance, and how does feedback change upstream and downstream hormones?” Train that reasoning explicitly with diagrams and scenarios.
- Master the big systems first, then worry about polish. Strong command of a handful of core pathways will pay off far more than scattered memorization of every hormone name you have ever seen.





















