It's July 1st of your third year in attending life. You are staring at your inbox: 50+ MyChart messages, six unfinished notes from yesterday, and an admin email about “productivity opportunities.” You did not train a decade to babysit an EMR and type for a living.
You’re not a brand-new hire anymore. You’re not yet the senior “institutional monument” either. You’re right in that sweet spot: Year 3 attending. This is exactly when you should start pushing—strategically—for tech upgrades and scribes.
Let’s walk this out chronologically: what to do Year 1, Year 2, early Year 3, and exactly how and when in Year 3 to negotiate for better tools and actual help.
Year 1 Attending: Quiet Data Collection Mode
At this point you should not be charging into the CMO’s office demanding scribes and a shiny AI note assistant. You do not have leverage yet. You have homework.
Your job in Year 1 is to set yourself up for the negotiation you’re going to have later.
Months 1–6: Learn the system and baseline your pain
You just started. Here’s what you should be doing behind the scenes:
- Learn all the native EMR tools.
- SmartPhrases, templates, order sets, “dot phrases,” whatever your system calls them.
- Every IT trainer will say “no one uses this, but it’s really helpful.” That usually means it saves time.
- Track your own after-hours work.
- Rough numbers are fine. Example I’ve seen:
- 1.5–2 hours/night finishing notes
- 3–4 hours over the weekend catching up
- Log it: “Week of Aug 7: 2.5 hours nightly in-basket; 4 hours weekend.”
- Rough numbers are fine. Example I’ve seen:
- Note what’s actually causing the pain:
- Inbox messages?
- Visit note bloat?
- Refill protocols?
- Prior auth nightmares?
By 3–6 months you want specific, boring data, not vibes. Vibes do not get you scribes. Numbers do.
Months 7–12: Start building your justification
Now you understand the clinic/hospital flow. Time to collect quiet ammunition.
At this point you should:
Pull your productivity data.
- RVUs, patient encounters per clinic day, procedure volume, wRVU/clinic session, etc.
- Get at least 3–6 months of clean data once your panel is “full.”
Document the spillover.
- How many notes are left open after clinic every day?
- Time from visit to note completion?
- Number of in-basket messages per clinic session?
Track any measurable risk or quality issues:
- Delayed notes leading to billing hold-ups.
- Missed messages because the inbox is overloaded.
- Refill errors due to high throughput and low bandwidth.
Put this somewhere you control: spreadsheet, OneNote, whatever. You’re building an argument: “Here’s what I accomplish. Here’s where the system is failing me. Here’s what that’s costing the organization.”
Year 2 Attending: Prove Reliability, Test Fixes, Build Allies
By Year 2 you’re no longer “the new doc.” People know if you’re solid or flaky. If you want leverage, you must be in the “solid” bucket.
Early Year 2 (Months 13–18): Show you’re a good investment
At this point you should be:
- Consistently meeting or slightly exceeding productivity expectations.
- Not constantly on an admin watchlist for late notes or angry patient complaints.
- Showing you’re coachable: you’ve tried their fixes first.
Do these, in order:
Optimize what you can control.
- Ruthless template optimization. Build templates for the 10–15 most common visits.
- Use all available EMR tools: phrase libraries, order sets, quick orders.
- Turn off non-essential inbox notifications if your system allows.
Test low-cost supports first.
- Shared in-basket pools with RN/MA filtering.
- Standard refill protocols.
- Pre-visit planning by staff.
- Voice recognition software if available (Dragon, etc.).
You do this for two reasons:
- To actually see what helps.
- To show, later, that you already “tried X, Y, and Z” before asking for bigger investments.
- Start building admin allies.
- Identify your immediate leaders: clinic medical director, service line chief, practice manager.
- Ask for quarterly or semiannual check-ins.
- In those meetings, share data calmly:
- “Here’s my RVU trend.”
- “Here’s my average after-hours EMR time: 8–10 hours/week.”
Do not ask for scribes yet. You’re still laying groundwork.
Late Year 2 (Months 19–24): Pilot mindset and strategic visibility
Now you start floating the idea that tech and staffing upgrades are not “nice-to-haves” but performance multipliers.
At this point you should:
Frame the problem in institutional language.
- Not: “I’m exhausted, I hate charting.”
- Instead:
- “I’m consistently at 90–100th percentile in wRVU for my FTE, but it’s costing 8–12 hours/week of uncompensated work.”
- “This level is not sustainable; I’m concerned it’ll affect retention.”
Ask about existing or upcoming initiatives.
- “Is the hospital looking at AI scribe tools?”
- “Are any departments piloting scribes, voice tools, or new EMR modules?”
- “Are there funds for workflow innovation pilots tied to productivity or burnout?”
Position yourself as the pilot person.
- “If there’s a chance to pilot a scribe or AI note tool, I’d be very interested. My volume is stable and I’m meticulous with documentation, so I’d be a clean test case.”
You’re not negotiating yet. You’re making sure that by the time you hit Year 3, leadership already sees you as:
- High-volume,
- Reasonable,
- Data-oriented,
- Willing to pilot solutions.
Year 3 Attending: This Is When You Negotiate
Here’s the punchline: the best time to push hard is mid-Year 3. Not day one. Not after you’ve already threatened to quit. You want enough historical data, enough credibility, and enough relationship capital to make the ask land.
Let’s break Year 3 down.

| Period | Event |
|---|---|
| Year 1 - Months 1-6 | Learn EMR, baseline data |
| Year 1 - Months 7-12 | Track workload, outcomes |
| Year 2 - Months 13-18 | Optimize, build credibility |
| Year 2 - Months 19-24 | Float pilots, gather allies |
| Year 3 - Months 25-30 | Formal ask for pilots |
| Year 3 - Months 31-36 | Negotiate permanent support |
Months 25–27: Prep your case
At this point you should stop thinking “I’m drowning” and start thinking like a business proposal.
You need four categories of data:
Productivity
- 12–18 months of:
- RVUs/month
- Clinic sessions/week
- No-show rates (if relevant)
- Procedure numbers
- 12–18 months of:
Workload & burn time
- After-hours EMR time (rough range acceptable: “7–10 hours/week” with examples).
- Average notes unfinished at end of clinic.
- Turnaround time:
- Notes signed within 24 or 48 hours?
- Patient message response time?
Impact on revenue & quality
- Instances of delayed billing due to late notes.
- Days when clinic ran behind 60–90 minutes because of documentation.
- Any QI data linking message overload to errors or complaints.
Comparisons
- Benchmarks from your specialty’s burnout literature if you can pull them.
- Rough averages from your colleagues (without naming names): “Most within our group are around X; my metric is Y.”
Build a 1–2 page summary. Not a manifesto. A tight brief.
Then identify what exactly you want:
- Option A: Human scribes (in-room or virtual).
- Option B: AI scribe tool (ambient listening, auto-draft note).
- Option C: More robust voice recognition + template optimization with IT.
- Option D: Mix: partial scribe coverage + EMR template build support.
Do not walk in saying “I just want help.” Walk in saying “I want to pilot X, with Y metrics, for Z months.”
Months 28–30: Make the formal ask
This is the core negotiation window.
At this point you should schedule a dedicated meeting with:
- Your medical director/chief, and
- The practice administrator or operations lead.
Go in with:
- Your 1–2 page data summary.
- A concrete proposal (3–6 month pilot).
- A cost-benefit framing.
Example script structure:
Open with what’s working.
- “Over the last year and a half, my volume has stabilized at [X RVUs/month], [Y patients/clinic], with quality metrics [fill in if you have them]. I’m committed to sustaining that.”
State the problem in their language.
- “To keep that up, I’ve been averaging 8–10 hours per week of after-hours EMR time. That’s not sustainable long term and risks burnout and retention.”
Present data.
- Brief walk-through of your summary.
- Highlight specific bottlenecks:
- 30–40% of time on messaging.
- 20–30% on note formatting / boilerplate.
Propose a pilot with success metrics.
- “I’d like to propose a 3-month pilot using [scribe / AI scribe / upgraded voice recognition] with the following measurable goals:
- Reduce after-hours EMR work by 50%.
- Maintain or increase RVUs.
- Improve time-to-close notes to same day for >80% of visits.”
- “I’d like to propose a 3-month pilot using [scribe / AI scribe / upgraded voice recognition] with the following measurable goals:
Address cost directly.
- For human scribes:
- Show estimated cost/clinic session.
- Show even a small increase in volume or improved throughput would offset.
- For AI tools:
- Subscription cost vs. reclaimed physician time.
- For human scribes:
You are not begging. You are offering them a return on investment: reduced burnout risk, stable or increased productivity, better patient satisfaction.
Which Option When: Human Scribe vs AI vs “Just Make the EMR Suck Less”
At this point you should choose your primary ask based on your practice type and environment.
| Situation | Best First Ask | Backup Ask |
|---|---|---|
| High-volume clinic, stable team | In-person or virtual scribe | AI scribe pilot |
| Mixed telehealth + in-person | AI scribe tool | Virtual scribe |
| Rural / small group with thin IT | Human scribe (shared) | Voice recognition + templates |
| Inpatient heavy, complex notes | AI scribe or voice tool | Partial scribe for rounds |
| Academic with residents | AI scribe + template support | Scribe on high-volume days |
Human scribes – when to push
Push hardest for human scribes if:
- You have very high visit volume with a lot of repetitive documentation.
- Your organization already uses scribes in some departments (ED, ortho, cardiology).
- You have relatively predictable clinics.
Leverage points:
- “ED and cardiology already use scribes with excellent throughput. We can adapt that model.”
- “If a scribe allows 2–3 more visits/day without lengthening clinic, that pays for itself.”
AI scribe / ambient tools – when to push
Push AI scribes if:
- Your institution is already talking about “digital transformation” or AI pilots.
- You do complex visits where in-room dictation to a human feels awkward.
- Telehealth is a big chunk of your practice.
Leverage points:
- “This technology reduces documentation while preserving physician-patient eye contact.”
- “Many large systems (Mayo, Stanford, etc.) are piloting or rolling this out; we risk falling behind.”
EMR optimization + voice recognition – when you’re blocked
Sometimes you’ll hear: “Budget freeze. No scribes this year.” Fine. Your move is:
- “Then I’d like dedicated IT support to build better templates and full-feature voice recognition. Here’s what I propose…”
This still moves the needle and creates a record that:
- You tried low-cost tech solutions first.
- They blocked higher-level support despite a reasonable case.
That history matters if/when you eventually consider leaving. Or when the next budget cycle opens.
Negotiation Tactics: How Hard to Push, and When to Back Off
You’re not a resident anymore. Playing nice but silent gets you nowhere. But storming in with threats is dumb unless you’re genuinely ready to walk.
At this point in Year 3, your tactics should be:
Step 1: Start with a pilot, not a permanent line item
Leaders love pilots. Pilots sound temporary and low-risk.
Propose:
- Duration: 3–6 months.
- Scope: one clinic per week, or all clinics if volume justifies it.
- Metrics:
- After-hours EMR time.
- Clinic on-time performance.
- Patient satisfaction (optional but nice).
- RVUs or encounters.
Agree up front: “If targets are met, we’ll discuss making this permanent.”
Step 2: Tie it explicitly to retention and sustainability
You don’t have to threaten. Just be clear:
- “I enjoy this practice and want to stay long term. To make that realistic, I need a sustainable documentation solution.”
If you’re already flirting with burnout:
- “Without meaningful change, I don’t think I can maintain my current panel size and schedule long-term.”
That sentence gets attention.
Step 3: Use comparison pressure—carefully
If other departments or competitors are doing better, mention it like this:
- “Our ED colleagues have scribes and report significant throughput gains. I’d like to see if similar benefits exist in outpatient IM.”
- “Local competitors X and Y advertise scribe support and AI tools as physician perks. That matters in retention and recruitment.”
You’re pointing out risk they actually care about: losing you and future hires.
If They Say No: Plan B and C
You should plan in advance for “No” or “Not now.”
If the answer is “Not now, maybe next year”
You respond with:
- “Okay. What would you need to see over the next 6–12 months to reconsider?”
- “Can we put a follow-up meeting on the calendar for Month X where we revisit this with updated data?”
And then you document everything. In email.
If the answer is a flat “No, we don’t do scribes/AI/etc.”
Your play changes:
Request the lower-cost optimization aggressively:
- Full-feature voice recognition.
- Dedicated EMR optimization session.
- Protected admin time to complete notes (carved into your schedule).
Quietly assess your true options:
- Do other local groups in your specialty offer scribes/AI?
- Are there hybrid or telehealth jobs with better tech support?
Tie this to your future decisions:
- You don’t need to threaten.
- But for yourself: “If in 6–12 months I still have 10 hours/week of unpaid EMR, I will seriously consider moving.”
That’s not drama. That’s self-preservation.
Day-to-Day Once You Have a Pilot
Let’s say they said yes to a 3–6 month pilot. At this point you should treat that pilot like an extended job interview—for the tool and for you.
First 2 weeks of the pilot
- Work closely with the scribe or AI trainer.
- Fix note structure quickly:
- Clear HPI structure.
- Standard exam and plan templates.
- Track your time obsessively for these first 2 weeks:
- Note completion time.
- Inbox time.
- After-hours work.
Weeks 3–8
Your job:
- Keep your clinical volume stable or modestly up.
- Do not let care quality slip; do not let documentation become garbage because “the AI does it.”
- Send leadership a 1–2 paragraph mid-pilot update:
- “After 4 weeks, my after-hours EMR time has decreased from ~9 hours/week to ~4 hours/week, RVUs are stable, and notes are signed same-day in 85% of encounters.”
That sort of email is gold. It gives them something to show their bosses.
End of pilot (Month 3–6)
At this point you should sit down with your leaders again and:
- Present before/after comparisons.
- Include:
- Numeric data.
- A couple of clean sample notes (de-identified, obviously).
- Say clearly:
- “This has made my practice sustainable. Without it, I don’t think I can maintain current volume long-term.”
- “I’m asking that we make this support permanent.”
If they still balk despite clear benefits, you’ve learned something important about how your institution values physicians’ time and longevity. Act accordingly.
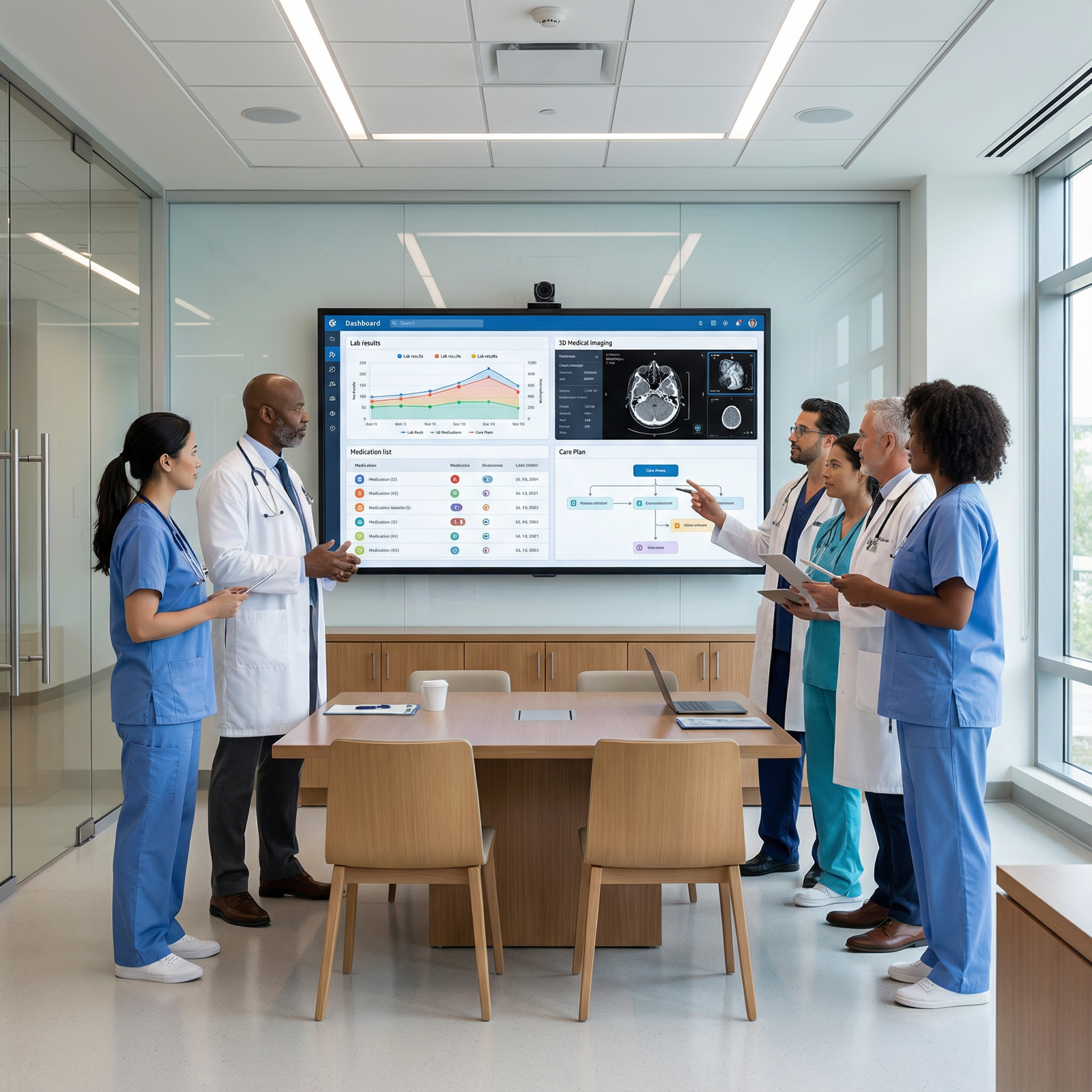
Quick Visual: Where Your Time Is Going

| Category | Value |
|---|---|
| Direct patient care | 50 |
| Documentation during clinic | 20 |
| After-hours EMR | 20 |
| Admin/meetings | 10 |
Your negotiation is about cutting that “After-hours EMR” slice in half without shrinking clinical care.
Final Takeaways
- Year 3 is the right moment to negotiate for tech upgrades and scribes because you finally have leverage: data, volume, and credibility.
- Do the groundwork in Years 1–2: track your time, learn the tools, build allies, and show you’re a good investment.
- When you ask, come with a concrete, time-limited pilot proposal tied to measurable outcomes—and be honest with yourself about what you’ll do if the answer is no.