The clicks you think are just “charting” are quietly writing your promotion story behind your back.
The Data Trail You Forgot You Were Leaving
Let me be very clear: once you are out of residency and on faculty or in an employed attending role, your EHR behavior is no longer just an IT issue. It is evidence. For or against you.
Most physicians still think promotion dossier = publications, teaching evaluations, letters. That’s the stated system.
Behind the scenes, especially at large health systems and academic centers, there’s an unstated system: EHR metadata. Clicks, timestamps, order patterns, inbox turnaround, note templates, after-hours activity. All of it sitting in data warehouses that leadership, quality officers, and informatics people mine when they’re trying to answer questions like:
- Who’s actually pulling their weight clinically?
- Who’s “efficient” vs who is dangerous?
- Whose documentation is driving revenue?
- Who looks like a future medical director or division chief?
- Who is burning out and becoming a risk?
You’re not told this. But committees see it. CMIOs see it. Division chiefs see distilled versions of it in “dashboard meetings” you’re not invited to.
Let me walk you through how your click patterns in the EHR quietly shape your promotion narrative—sometimes years before you ever ask for a title change.
How EHR Clicks Become “Your Reputation” in the C-Suite
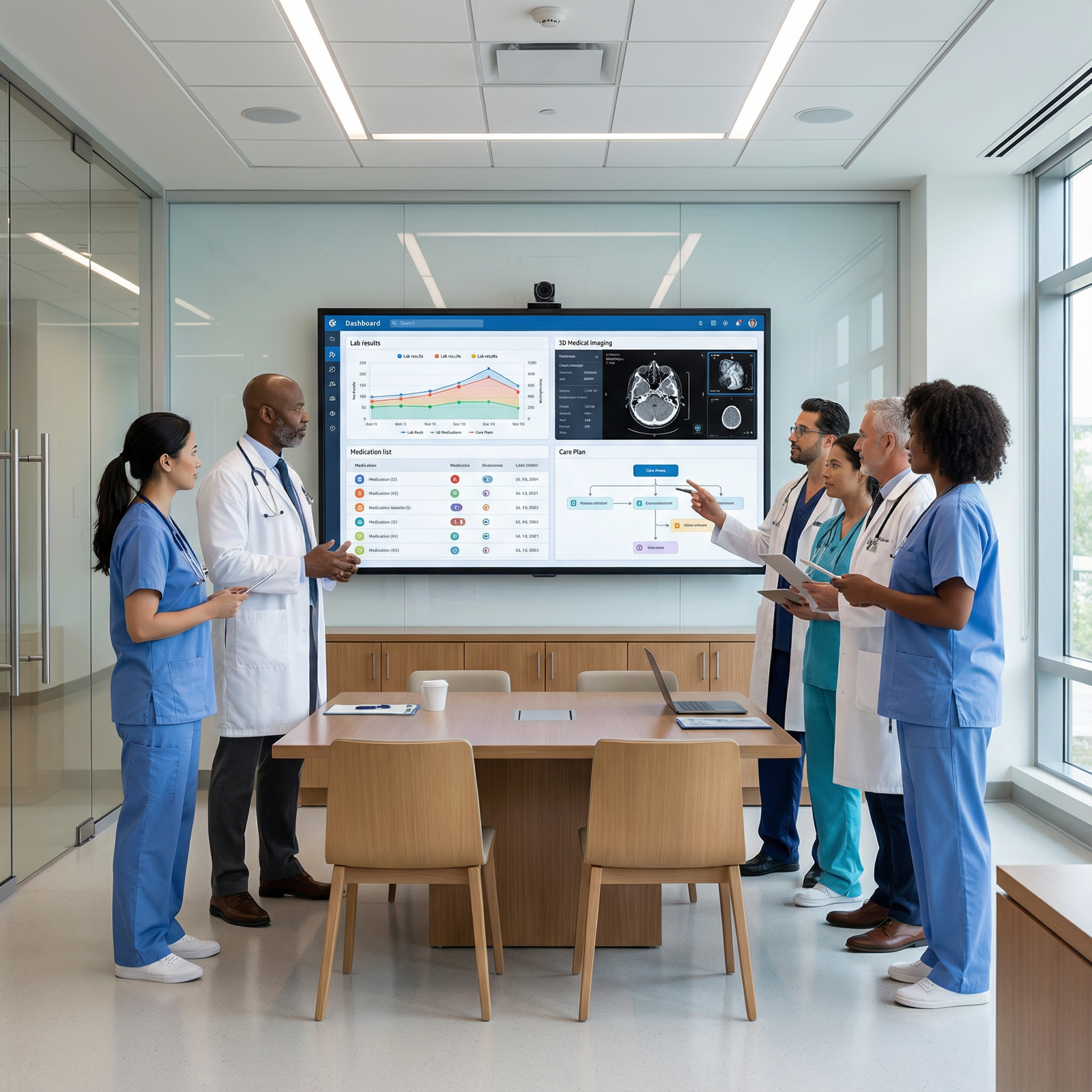
The promotion committee rarely opens Epic logs in real time. That’s not how this works. The pipeline looks more like this:
- Raw interaction data from the EHR feeds into analytics tools.
- Quality, operations, and informatics teams build dashboards.
- Chiefs and chairs see these dashboards in leadership meetings.
- That picture of you—aggregated, simplified—is what’s in their heads when your name comes up.
You’re living in the raw world. They’re living in the dashboard world.

| Category | Value |
|---|---|
| Clinical Volume | 95 |
| RVUs per Hour | 88 |
| After-Hours Time | 72 |
| Inbox Lag | 80 |
| Note Length | 65 |
| Order Set Use | 78 |
Those numbers are not “neutral.” People assign meaning to them:
- High clinical volume + decent RVUs + low after-hours time → “Efficient workhorse. Potential leader.”
- High after-hours time + average RVUs → “Struggling. Needs coaching. Maybe burnout risk.”
- Very low inbox response times + long notes → “Safe but slow. Good for complex patients, maybe not for leadership.”
- Heavy order set use + consistent metrics → “Systems thinker. Could help with optimization, committees, medical directorships.”
You think you’re just surviving clinic. Someone else is quietly labeling you “optimized,” “problematic,” or “underperforming” based on click behavior you barely notice.
The Types of Click Data That Actually Matter
I’ve sat in meetings where these exact metrics were pulled up on a projector—physicians identified by name—and discussed in absurdly casual tones.
The main categories:
Time-stamped events
When you open charts, when you sign notes, when you place orders, when you respond to messages. They build a picture of your workday reality.Interaction density
How many clicks per visit, orders per encounter, messages per day. Sometimes used as a crude proxy for complexity or inefficiency.Template and order set usage
Are you using system-approved templates and decision support, or free-texting your way through life? This screams “team player” vs “cowboy” to certain leaders.After-hours activity (“pajama time”)
Chair sees a graph of your logins at 10:30 pm every night? That becomes a narrative bullet: “high burnout risk,” or “not efficient in clinic,” depending on the room.
And because you’re never in that room, you don’t get to explain.
What Your Click Patterns Say About You (Whether You Like It or Not)
Let’s translate this into promotion language. EHR metadata quietly feeds judgment across four main domains they care about post-residency: productivity, professionalism, safety, and leadership potential.
1. Productivity: “Are You Worth Your FTE?”
They won’t say it that bluntly. But the math is that blunt.
A typical internal dashboard tying EHR behavior to productivity will track:
- Encounters per session
- RVUs per hour and per click/interaction
- Average chart closure time
- “Time in chart per encounter”
| Raw Metric | How Leadership Reframes It |
|---|---|
| Charts closed same day | Reliable and efficient |
| Charts >3 days to close | Disorganized, possible backlog risk |
| Low time in chart + high RVUs | Efficient, potential coach for others |
| High time in chart + low RVUs | Struggles, may need workflow intervention |
If your clickstream shows:
- Charts left unsigned for days
- Notes finalized well after-hours consistently
- High click counts per visit with low throughput
You’re perceived as “labor intensive.” That alone can hold you back when someone asks: “Is this person ready to step into a leadership role and maintain clinical productivity?” Because the data implies you’re already at your limit.
On the other hand, the clinician who:
- Closes charts the same day
- Has modest time-in-chart per encounter
- Minimal pajama time
Gets described as “efficient, organized, handles volume well.” That line makes its way into emails, letters, and semi-formal comments at promotion meetings.
They’re not just looking at your CV. They’re thinking of your graph.
2. Professionalism: “Can We Trust This Person With More Responsibility?”
There’s a reason compliance, risk, and quality officers love EHR data: it exposes patterns.
Here’s what quietly gets flagged:
Late signatures on critical results or notes
If you consistently sign discharge summaries two weeks late, that shows up in audits. It’s interpreted as reliability—or lack of it.Inbox neglect
Long delays responding to patient messages, test results, or staff communications look like unprofessionalism. It becomes ammo: “We’ve had concerns about responsiveness.”Odd-hour charting without explanation
Chronically documenting at 2 am on outpatients despite daytime clinic suggests either time mismanagement or instability. No one will say that out loud in front of you. They say it in the debrief after your name comes up.Template abuse / copy-forward dependence
Risk and compliance folks run tools that scan for high levels of cloned text, copy-paste events, and boilerplate with minimal updates. That gets labeled as “documentation risk.”
Your click patterns are building a case about whether you have the professional discipline to hold an administrative title or be promoted. Not the whole case. But enough to sway marginal decisions.
When Clicks Become a Quality or Safety Story
This is the part most attendings never see. Quality and safety committees correlate EHR behaviors with outcomes.
You hear “we’re looking at trends.” What’s actually happening is: they’re matching your interaction trail with adverse events, missed follow-ups, readmissions, and complaints.

| Category | Value |
|---|---|
| Physician 1 | 1.2,0 |
| Physician 2 | 3.8,2 |
| Physician 3 | 4.5,5 |
| Physician 4 | 2,1 |
| Physician 5 | 5,7 |
(Axis example they use informally: X = average days to act on abnormal result, Y = number of safety events linked to delayed follow-up.)
Patterns that hurt you badly when someone is deciding whether you’re “promotable”:
Delayed result acknowledgment
Being slow to click “acknowledge” on critical or even routine abnormal labs. Those timestamps get pulled in every root cause analysis.Order reversals and corrections
Lots of discontinuations, corrections, and modifications shortly after placing orders create a narrative of “sloppy ordering.” Especially if pharmacy or nursing raised concerns.Alert fatigue fingerprints
If you’re one of the high-alert override people, and there’s a medication event, your override patterns will be shown on a slide somewhere. I’ve seen attendings shocked when they’re confronted with “You overrode this allergy alert in 94% of cases over the last year.”
Over time, this builds into a labeled archetype: “safe pair of hands” versus “cutting corners” versus “walking near the edge.”
Guess whose CV gets a halo effect when they ask to be promoted to associate professor or medical director?
The Leadership Question: Can You Think in Systems or Only in Single Visits?
Here’s the dirty little secret: modern promotions in big systems are not only about how good you are one-on-one with patients. Leadership roles, titles, committee chairs—these go to people who can “speak data” and “play nicely with the EHR.”
If your click patterns show that you:
- Use standardized order sets appropriately
- Leverage templates that align with institutional pathways
- Have stable documentation metrics over time
- Adapt to new workflows without a months-long dip in performance
You get coded—in people’s heads—as “systems-aligned” and “change-capable.”
Those are the people CMIOs and chairs put on:
- EHR optimization committees
- Quality improvement pods
- Documentation steering groups
And once you’re “in the room” for those, your name shows up in exactly the places that feed promotion letters and leadership nominations.
On the flip side, the chronic EHR complainer whose data also shows:
- Avoidance of order sets
- Extreme free-text use
- Resistance to new workflows (everyone else adapted, your metrics never did)
Becomes “difficult,” “old-school,” or “not adaptable” in informal discussions. Even if you’re clinically excellent, this can freeze you out of the inner circle where opportunities originate.
How to Make Your Click Patterns Work For You
You’re not getting out of the EHR. That fantasy is dead. What you can do is be deliberate about the trail you’re leaving.
Think of this less as “gaming the system” and more as controlling your own narrative.
1. Stabilize Your Core Metrics
You want your dashboard self to look boring in all the right ways:
- Charts closed within 24 hours, most of the time.
- Minimal backlog of unsigned notes and incomplete charts.
- Reasonable time in chart per encounter, no wild swings.
That means building simple, repeatable behaviors:
- Finish the note before the patient leaves whenever possible. Even a structured skeleton with key elements is better than a blank canvas at midnight.
- Set a personal rule: nothing leaves clinic with >2 unsigned notes unless there’s a truly good reason.
- Create 2–3 rock-solid templates for your highest-volume visit types. Refine them until they’re fast and compliant.
You’re not trying to be perfect. You’re trying to avoid standing out negatively on any of the standard graphs.
2. Tame Your Inbox Footprint
Your inbox is one of the fastest ways to get quietly flagged as “unreliable” or “overwhelmed.”
Do this:
- Establish 2 fixed times per day where you reliably clear the bulk of messages. Early AM and last half-hour of the day work well.
- Ruthlessly delegate what’s appropriate to staff or pooled inbox workflows. Not every refill requires your click.
- Use smart phrases for common patient messages so your click-and-type load is consistent and fast.
From the data perspective, this creates:
- Predictable response times
- Low outliers (not many >72-hour waits)
- An image of consistency and reliability
Those graphs get thrown up in service line meetings more than you think.
3. Make Friends With Order Sets and Templates—Strategically
You do not have to love them. But you’d better know how to use them when it matters.
Why? Because leadership equates “uses standardized workflows” with “scalable and safe.”
Pick your spots:
- For the common conditions your organization has built pathways for (sepsis, chest pain, diabetes, CHF), use their tools. Even if you tweak them.
- Customize a copy of key order sets instead of building everything from scratch each time.
- Use macro-templates that bake in required documentation for billing and quality (smoking status, med rec, screening, etc.).
From a metadata standpoint, this makes you look:
- Aligned with organizational priorities
- Onboard with quality initiatives
- “Model-able” to others (translation: promotion material)

| Step | Description |
|---|---|
| Step 1 | EHR Click Patterns |
| Step 2 | Analytics Dashboards |
| Step 3 | Quality and Productivity Meetings |
| Step 4 | Informal Reputation |
| Step 5 | Committee Invitations |
| Step 6 | Leadership Roles |
| Step 7 | Promotion Narrative |
That pipeline is real. I’ve watched it play out for years.
4. Control Your After-Hours Signature
The reality: everyone has some pajama time. But patterns matter.
If your logins show:
- Nightly charting at 9–11 pm
- Weekend bursts of cleanup every week
- Spikes after new workflows roll out that never settle down
You get labeled, quietly, as someone who is either burnt out or unable to manage clinic time. Neither is a great platform for “I’m ready to be promoted.”
Try this:
- Cap yourself. For example, “no routine charting past 9 pm on weeknights, and no more than 1 hour on weekends.”
- Shorten notes during the day rather than “doing it right” at 11 pm. Perfect documentation that kills your home life is not a win.
- When new workflows roll out, proactively ask for help early if your metrics tank. Let someone document that you engaged and improved.
That last part matters: committees like to see that you respond to feedback and adapt. EHR metrics provide the “before/after” story.
Using Your Data to Your Advantage
Here’s something almost no one does: request your own data.
You’re allowed to ask informatics or quality teams:
- For your average chart closure times over the last year
- For your time-in-chart by encounter type
- For your inbox response time distributions
- For your after-hours usage trends
You don’t have to frame it as “I want ammo for promotion.” You say: “I’m trying to improve my efficiency and understand my patterns.”
Once you have it:
- Identify 1–2 areas where you’re an outlier in a good way. High same-day closure rate, for example.
- Fix or at least improve 1 obvious weak spot over 3–6 months.
Then, when your CV is being updated or you’re talking with your division chief, you can say:
“We pulled my data last year—my same-day closure rate is consistently >85%, and I reduced my after-hours time by about 30% since July by streamlining templates.”
That’s the kind of sentence that ends up quoted in letters and reviews. It links your name with “data-aware, self-improving, efficient.” That is promotion fuel.
The Part No One Tells You: Politics and Perception
Let me be blunt.
EHR data does not exist in a vacuum. The same pattern will be interpreted differently based on:
- Whether you’re already seen as a “rising star”
- Whether your chief likes you
- Whether your service line is drowning or thriving
I’ve seen this double standard in action:
- Rising star: “They’re doing a lot of work from home at night—dedicated.”
- Problem child: “They can’t manage their time; always behind.”
Same graph. Different story.
So your job is twofold:
- Make sure the raw numbers don’t give anyone easy negative talking points.
- Build enough relational capital—teaching, collegiality, committee contributions—that people are primed to read your data generously.
The EHR clickstream is evidence. But people pick the story they want that evidence to tell. Do not make it easy for them to pick the wrong one.
FAQs
1. Can EHR data actually stop me from getting promoted?
Yes, indirectly. Rarely will someone say, “We’re not promoting you because of your chart closure rate.” What happens instead is: your chief or chair has a vague impression of you as disorganized, slow, or risky—impressions heavily influenced by EHR metrics shown in leadership meetings. That impression then weakens their enthusiasm when they advocate for you, which is how promotions quietly stall.
2. Should I worry that my every click is being “surveilled”?
You should assume your patterns are visible, not that someone is watching each click in real time. No one has time for that. But if there’s a concern—safety event, complaint, outlier pattern—audits can and do drill down deep. The smart approach is not paranoia; it’s being intentional so that when that spotlight swings your way, the story your data tells matches the professional image you want.
3. Is there any benefit to being highly efficient in the EHR beyond my own sanity?
Absolutely. Efficient, stable EHR metrics are a quiet but powerful credential. They get you tapped for optimization projects, pilot programs, and workflow committees. Those roles lead to titles—“Associate Medical Director of Informatics,” “Quality Lead for Ambulatory”—that carry serious weight in promotion dossiers, especially at academic and large integrated systems.
4. How early in my attending career do these patterns start to matter?
Much earlier than you think. Within your first 6–12 months, you’ll generate enough data for leadership dashboards to form an initial profile of you. That profile tends to stick. It’s much easier to start off with solid habits and a clean data picture than to dig yourself out of a three-year narrative that you’re “always behind” or “not good with systems.”
You’re already leaving a trail in the EHR. The question is whether that trail makes you look like a future leader—or a permanently overwhelmed workhorse.
With that awareness in place, you’re ready to think about the next step: how to turn that invisible data reputation into explicit leadership roles and formal titles. But that’s a story for another day.




















