
From Nurse to Physician: A Late-Career Transition Success Story
Introduction: Redefining the Path to Physician
The traditional image of a future physician is often a college student in their early twenties, moving straight from undergraduate studies into medical school. But increasingly, medical education is enriched by professionals who come from non-traditional backgrounds—especially from nursing.
This article shares the story of Sarah, a registered nurse who made a late-career transition from nurse to physician. Her journey illustrates not only what is possible, but also how prior nursing experience can become a powerful asset in medical school, residency, and beyond. Along the way, we will explore:
- The motivations that drove her career transition
- The academic and logistical steps she took to prepare
- How her nursing background shaped her medical education and patient care
- Practical advice for other nurses considering a similar path
Whether you are a nursing student, an experienced nurse, or a career changer exploring medicine, Sarah’s story offers a detailed roadmap for navigating this challenging and rewarding nurse to physician transition.
The Catalyst for Change: From Bedside Nurse to Aspiring Physician
Discovering a New Professional Calling
After more than ten years as a registered nurse, Sarah was a skilled clinician, trusted by colleagues and patients alike. She worked primarily on a busy medical-surgical unit in a community hospital, where she:
- Managed complex post-operative patients
- Coordinated care among multiple specialties
- Educated patients and families about medications and discharge planning
Over time, she began to notice a pattern: her favorite parts of the job involved thinking through diagnoses, anticipating complications, and participating actively in medical decision-making. She loved when physicians would explain their reasoning at the bedside and invite her input.
Sarah realized that while nursing allowed her deep involvement in patient care, she often wanted to engage at a different level of responsibility—to:
- Formulate differential diagnoses
- Order and interpret diagnostic tests
- Initiate and adjust treatment plans
These interests went beyond professional curiosity; they represented a growing sense that she wanted to expand her scope of practice and become a physician.
The Subtle Constraints of a Role She Loved
Importantly, Sarah did not leave nursing because she disliked it. She found profound meaning in advocating for patients, managing crises, and supporting families. But she also felt the constraints of her role:
- She sometimes knew that a patient needed a change in management but could only suggest it, not order it.
- She wanted to understand the pathophysiology behind complex conditions at a deeper level.
- She was increasingly drawn to the intellectual challenge of medical diagnostics.
Watching physicians make time-sensitive decisions in the ICU and on the medical floors made her wonder: could she be in that role? Was it too late to pursue that path?
Navigating Doubts, Fears, and External Opinions
As with many non-traditional paths to medicine, Sarah’s biggest obstacles at first were internal. Questions swirled:
- “Am I too old to go back to school?”
- “Can I afford to leave a stable nursing salary?”
- “Will medical schools take me seriously as a late-career applicant?”
Her colleagues had mixed reactions:
- Some were thrilled and supportive, offering to write letters of recommendation.
- Others expressed concern: “Are you sure you want to start all over?” “Medical school debt is no joke.”
- A few assumed that nursing was a “final” career and saw a transition as unnecessary.
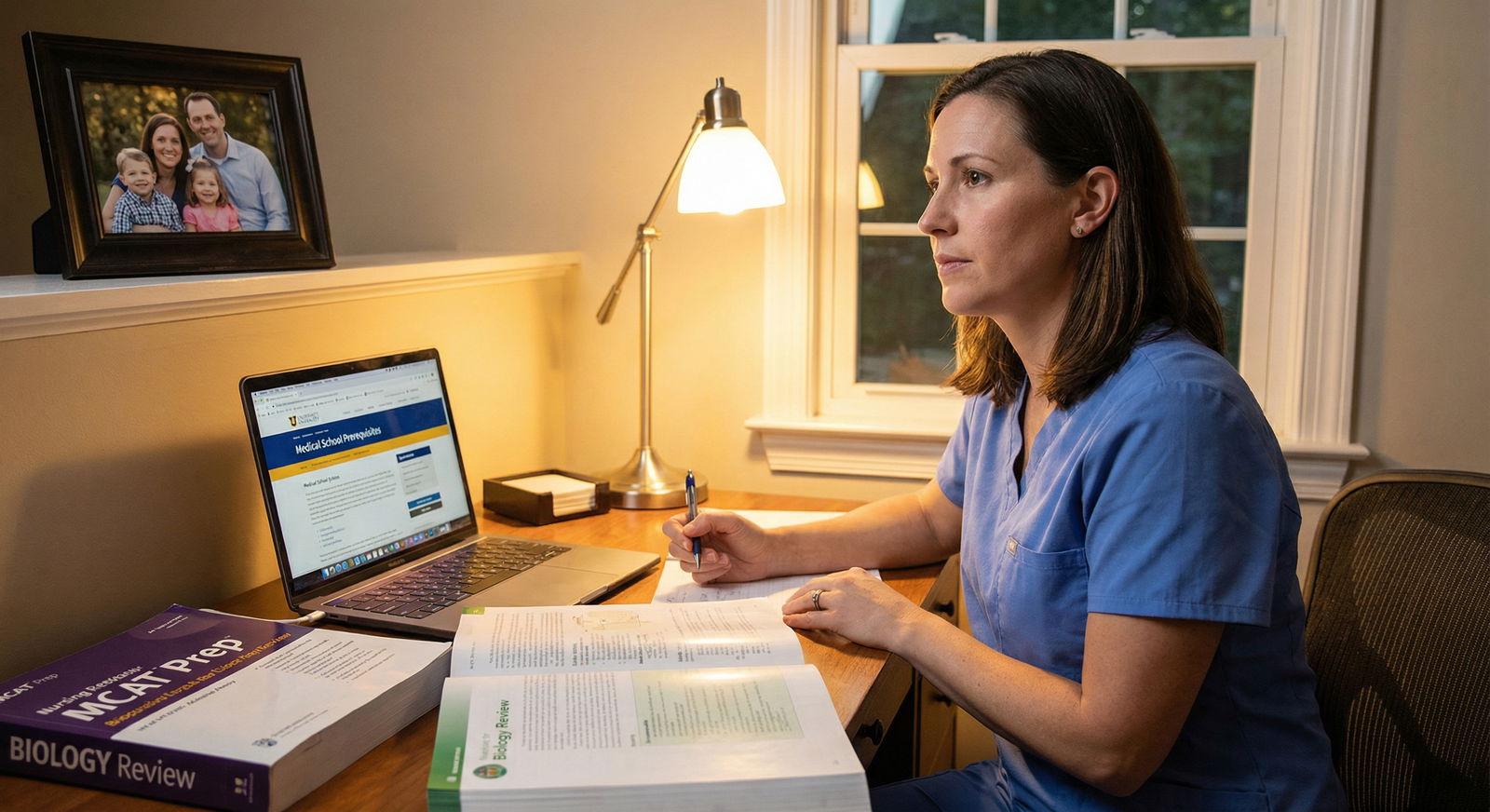
Sarah also had real-life obligations: a mortgage, a partner, and two young children. The idea of full-time medical education for years felt risky. But she ultimately recognized that the regret of not trying would be heavier than the challenges ahead.
She began to research stories of other nurses who had successfully become physicians and found reassurance in their examples (including resources like From Nurse to Physician: Bridging the Gap). Their journeys helped her reframe fear as a normal part of growth in any major career transition.
Preparing for the Journey: Academic, Financial, and Emotional Planning
Understanding Educational and Admissions Requirements
Transitioning from nursing to physician begins with a clear understanding of medical school prerequisites. While every institution differs slightly, Sarah discovered that she needed to ensure:
A qualifying bachelor’s degree
- Her BSN fulfilled the basic degree requirement.
- She confirmed that her program was from an accredited institution accepted by medical schools.
Completion of core science coursework
Many nursing programs do not include the full premed sequence or may not emphasize certain lab components. Sarah reviewed each target school’s requirements and identified gaps such as:- Two semesters of general chemistry with lab
- Organic chemistry with lab
- Physics with lab
- Additional higher-level biology (e.g., genetics, cell biology)
Competitive MCAT score
Even with years of clinical experience, she needed a strong MCAT score to demonstrate academic readiness in foundational sciences and critical reasoning.
Actionable Tip for Nurses
If you are considering this transition, gather syllabi and transcripts early and compare them against multiple medical schools’ prerequisites. Many nurses discover they need a post-baccalaureate program or standalone science courses to fill gaps.
Creating a Personalized Academic Roadmap
Sarah outlined a 2–3 year plan to become a competitive applicant:
Year 1–2: Prerequisite Courses and MCAT Preparation
- Took evening and weekend science courses at a nearby university while working part-time as a nurse.
- Scheduled protected study time during the week for MCAT prep.
- Used her clinical background as an anchor to understand the real-world relevance of physiology, pharmacology, and pathology.
Year 2–3: Application Cycle
- Prepared personal statements emphasizing her nursing experience and growth.
- Collected letters of recommendation from physicians, professors, and her nurse manager.
- Continued working per diem or part-time to support her family.
This long-range planning helped make the financial and time commitment feel more manageable.
Financial and Lifestyle Planning for a Career Transition
A late-career transition into medicine has major financial implications:
- Loss of full-time nursing income for several years
- Tuition and fees for prerequisite courses, MCAT, and medical school
- Potential relocation costs for medical school and residency
Sarah and her partner sat down to:
- Calculate their baseline living expenses
- Build a realistic budget for the premed and medical school years
- Create an emergency fund before she reduced her work hours
- Explore federal loans, scholarships, and need-based aid
They also discussed changes in family roles—her partner would shoulder more childcare and household responsibilities while Sarah devoted time to study and medical education.
Building a Strong Support System
Recognizing that she could not do this alone, Sarah invested deliberately in relationships and mentorship.
Mentorship from Physicians and Educators
She approached physicians she had worked with and asked:
- “What qualities make a strong medical student and resident?”
- “How can I best position my nursing experience in an application?”
- “Would you be willing to let me shadow you and possibly write a letter of recommendation?”
Most were enthusiastic and supportive. Their guidance helped her understand the culture of medical education, the realities of training, and the expectations of residency programs.
Peer and Family Support
Sarah also:
- Joined online communities and forums for non-traditional and nurse-to-physician applicants.
- Connected with other nurses taking premed courses or studying for the MCAT.
- Scheduled regular check-ins with her partner to reassess workload, stress, and family needs.
This network provided emotional support, accountability, and reassurance during particularly difficult stretches.
Leveraging and Expanding Clinical Experience
Although she had years of bedside experience, Sarah recognized that admissions committees still value structured, physician-focused exposure to medicine.
She:
- Shadowed internists, hospitalists, and family medicine physicians to understand their day-to-day roles.
- Observed in clinic and inpatient settings to compare the different rhythms of care.
- Asked physicians to explain their clinical reasoning as they examined patients and made management decisions.
These experiences:
- Clarified that internal medicine aligned well with her love of complex problem-solving and longitudinal patient care.
- Gave her specific patient stories to discuss in interviews.
- Demonstrated to admissions committees that her decision to pursue medicine was informed and realistic.
The Medical School Experience: Adapting as a Non-Traditional Student
Standing Out in the Application Process
By the time Sarah applied, her application presented a compelling narrative:
- A decade of nursing experience across acute and step-down units
- Leadership roles as a charge nurse and preceptor
- Prerequisite science coursework with strong grades
- A competitive MCAT score supported by real-world clinical insights
Her personal statement emphasized:
- How nursing had shaped her understanding of patient care, empathy, and systems-level barriers
- Specific moments when she realized she wanted to be responsible for diagnosis and treatment decisions
- Her commitment to bridging nursing and medicine through respectful interprofessional collaboration
Admissions committees responded positively. During interviews, faculty frequently asked:
- “How will your nursing background influence your approach as a physician?”
- “What challenges do you anticipate as a non-traditional student?”
Her authentic reflections and concrete examples won over several programs, and she was accepted at multiple medical schools.
Adjusting to the Pace and Culture of Medical Education
The first year of medical school was a shock—even for someone accustomed to 12-hour shifts and complex patient loads. The volume of information, pace of coursework, and pressure of continuous assessments required a major shift in learning strategy.
However, Sarah soon recognized advantages from her nursing background:
- Clinical context for basic science: Concepts in physiology, pharmacology, and pathology were easier to anchor because she had seen real patients with heart failure, sepsis, and COPD.
- Comfort with patient interaction: Standardized patient encounters and early clinical skills workshops felt familiar rather than intimidating.
- Time management under pressure: Years of juggling multiple acutely ill patients translated into strong organizational skills and resilience during exam weeks.
She had to adapt her study methods—moving from memory-heavy studying to active learning strategies like spaced repetition, practice questions, and group discussions—but her professional discipline served her well.
Balancing Medical School with Family and Personal Life
As a mid-career student, Sarah’s responsibilities extended far beyond the classroom. Unlike many of her younger classmates, she:
- Attended school events and parent-teacher conferences
- Filtered study schedules around children’s bedtimes and weekend activities
- Shared household responsibilities with her partner
To maintain balance, she:
- Created weekly schedules that blocked out specific times for studying, family, exercise, and rest.
- Set realistic goals for each study session to avoid endless, unfocused hours.
- Communicated openly with faculty when family emergencies arose, advocating for herself professionally and respectfully.
Growing Resilience and Preventing Burnout
The stress of exams, clinical skills assessments, and future career decisions is intense in medical education—even more so when layered on top of a major career transition.
Sarah adopted deliberate strategies to protect her well-being:
- Mindfulness and reflection: Short daily mindfulness sessions and journaling helped her process emotions, especially imposter syndrome and comparison with younger classmates.
- Physical activity: Even 20–30 minutes of walking or light exercise several times a week helped maintain energy and focus.
- Community: She made time to connect with peers—both traditional and non-traditional students—to share experiences and normalize struggles.
Over time, the doubts that had once seemed overwhelming began to fade. She saw objective evidence of her competence through exam scores, clinical feedback, and, most importantly, patient interactions.
From Classroom to Clinic: Training as a Physician with a Nursing Foundation
Clinical Rotations: Where Nursing and Medicine Converge
Third-year clinical rotations were where Sarah’s prior nursing experience truly shined. On the wards and in clinics, she:
- Seamlessly navigated hospital workflows, EMRs, and interprofessional communication.
- Anticipated nursing concerns, current and future orders, and patient education needs.
- Built rapport quickly with patients, drawing on years of bedside communication.
Faculty and residents noticed:
- Her notes often included thoughtful nursing considerations and discharge planning elements.
- She treated nurses and allied health professionals as true partners in patient care.
- She was comfortable in high-acuity situations and remained calm in emergencies.
During her internal medicine rotation, she felt especially at home—synthesizing complex data, thinking through differentials, and discussing management strategies with her team. This confirmed her decision to pursue internal medicine residency.
Choosing a Specialty: Why Internal Medicine Fit
Sarah considered several fields—family medicine, emergency medicine, and anesthesiology—but ultimately chose internal medicine because it allowed her to:
- Work closely with complex, multi-morbid patients
- Engage in detailed diagnostic reasoning
- Build longitudinal relationships in outpatient settings if she chose primary care later
Her nursing background had already prepared her for:
- Interpreting vital sign trends and recognizing subtle changes in clinical status
- Understanding social determinants of health and barriers to follow-up care
- Coordinating among multiple specialists to advocate for patients’ needs
These strengths aligned naturally with internal medicine’s emphasis on comprehensive, patient-centered care.
Match Day and the Start of Residency
On Match Day, surrounded by classmates, family, and faculty, Sarah opened her envelope and learned she had matched into a well-regarded internal medicine residency program. The moment marked:
- The culmination of years of sacrifice, study, and perseverance
- A formal shift from student to physician-in-training
- The continuation—not abandonment—of her identity as a nurse, now integrated into her role as a physician
During residency, attendings and peers quickly recognized her as:
- A team member who understood the workloads and challenges of nursing staff
- An advocate for safe staffing, clear communication, and collaborative care
- A physician who prioritized bedside presence and patient education
Far from starting “from scratch,” she had built a physician identity on a strong foundation of nursing practice and patient care.
Reflection, Identity, and Inspiration for Other Nurses

A Fulfilled, Integrated Professional Identity
Looking back, Sarah does not see her career as “leaving nursing for medicine” but as an evolution of her calling to patient care. Her nursing background remains central to how she practices as a physician:
- She maintains a strong emphasis on bedside communication and education.
- She intentionally involves nurses in care planning and values their insights.
- She mentors residents and students to respect nursing expertise and collaborate effectively.
She also acknowledges the costs—financial strain, missed social events, and periods of intense fatigue—but feels that the ability to diagnose, treat, and guide complex medical decisions has been deeply fulfilling.
Advice for Nurses Considering Medical School
For nurses and other healthcare professionals thinking about transitioning to a physician role, Sarah emphasizes:
Your Nursing Experience Is a Major Strength
- You understand real-world patient care, hospital systems, and interprofessional teamwork.
- Admissions committees value this maturity and perspective.
Do a Thorough Reality Check
- Shadow extensively. Talk honestly with physicians at different stages (residents, attendings).
- Understand the training timeline, hours, and potential impact on your family and finances.
Plan, Don’t Rush
- Create a multi-year academic and financial plan.
- Give yourself adequate time for prerequisite courses and MCAT preparation.
Invest in Mentorship and Community
- Seek mentors who understand both nursing and medicine.
- Join communities of non-traditional applicants to share resources and encouragement.
Expect Self-Doubt—but Don’t Let It Decide for You
- Doubts are normal, especially during exams or difficult rotations.
- Return to your “why”: your motivation to deepen and expand your impact on patient care.
Her story stands as a powerful example that a late-career transition from nurse to physician is not only possible, but can create exceptionally empathetic, competent, and collaborative physicians.
FAQ: Nurse to Physician Career Transition
Q1: Is it realistic to transition from nursing to medical school later in life (30s, 40s, or beyond)?
Yes. Many medical schools welcome non-traditional applicants, including experienced nurses, because they bring maturity, clinical insight, and strong patient care skills. Age is less important than academic readiness, clear motivation, and the ability to handle the demands of training. You should, however, thoughtfully consider the length of training and long-term financial implications.
Q2: How can nurses practically prepare academically for medical school?
Start by reviewing prerequisites for several medical schools and comparing them to your nursing coursework. Common steps include:
- Completing additional sciences (full chemistry and physics sequences, often with labs)
- Taking advanced biology courses such as biochemistry or genetics
- Building a multi-month MCAT study plan using practice exams and question banks
Post-baccalaureate premed programs can be helpful, but many nurses succeed using a mix of university courses and self-guided MCAT preparation.
Q3: Does nursing experience make medical school or residency easier?
It does not make the content less demanding, but it changes how you experience it. Nursing gives you:
- Comfort with patient interaction and clinical environments
- A practical understanding of workflow, documentation, and interprofessional dynamics
- Insight into patient experiences and system-level barriers
You will still need to master large volumes of biomedical science and adjust to the different responsibilities of a physician. However, your background can significantly enhance your effectiveness in clinical rotations and residency.
Q4: What medical specialties are often a good fit for former nurses?
Former nurses can succeed in any specialty, but many are drawn to:
- Internal medicine for complex problem-solving and coordination of care
- Family medicine for continuity and holistic patient care
- Pediatrics if they have prior pediatric or NICU experience
- Emergency medicine or critical care if they come from ED or ICU nursing
Ultimately, your clinical interests, lifestyle goals, and training experiences should guide your choice, not just your nursing background.
Q5: How can nurses highlight their experience effectively in medical school applications?
Frame your nursing experience around:
- Specific patient stories that shaped your decision to pursue medicine
- Examples of leadership, teaching, or quality improvement projects
- Situations where you collaborated closely with physicians and contributed meaningfully to clinical decisions
- Skills like communication, resilience, cultural humility, and systems-based thinking
Letters of recommendation from physicians who have seen you in action, as well as from nurse leaders or educators, can powerfully reinforce your narrative.
By thoughtfully planning your academic path, leveraging your nursing experience, and building a strong support system, a nurse to physician transition can transform not only your career, but also the way you contribute to patient care and the broader healthcare team.




















