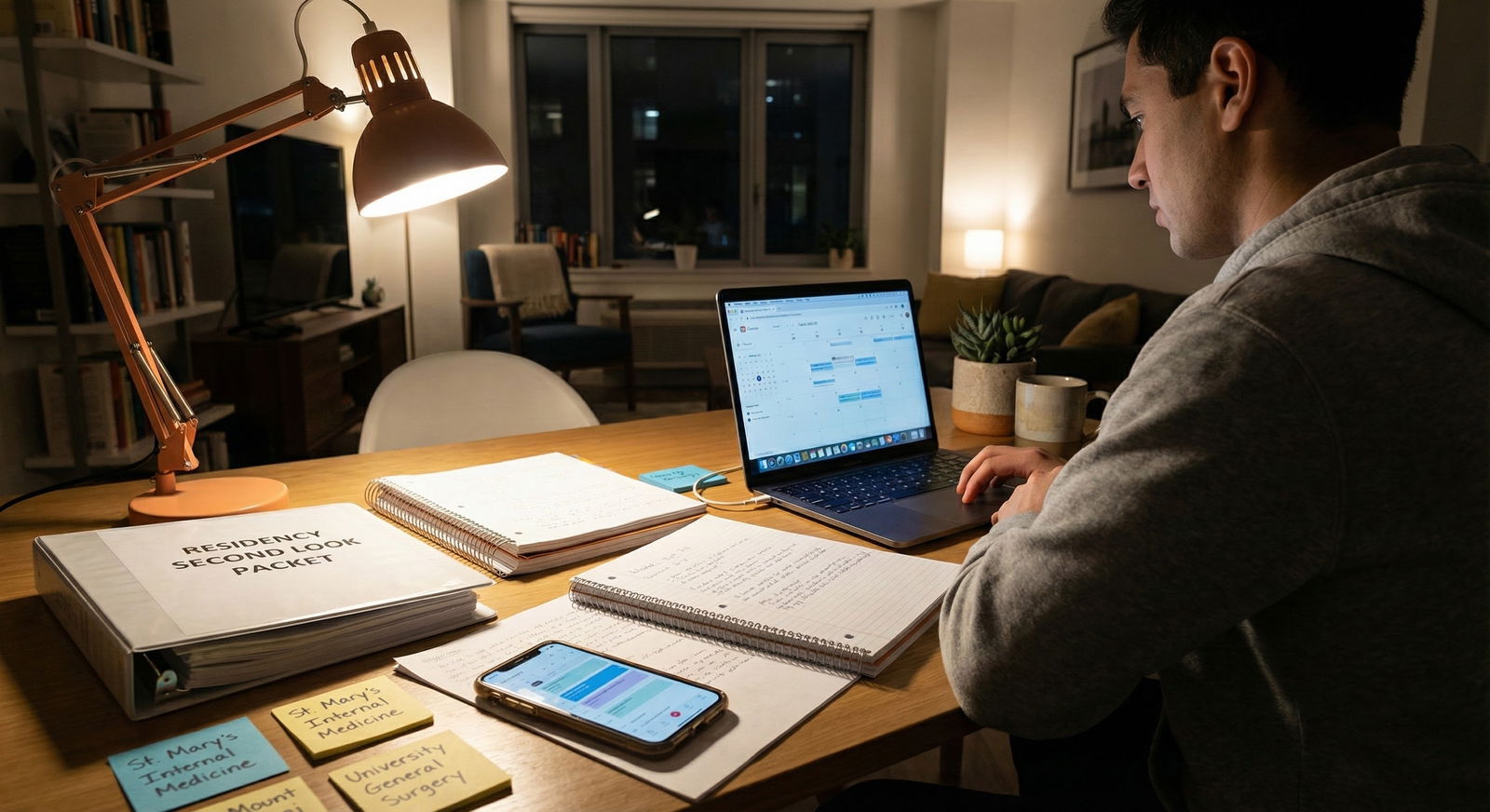
You’re on hour 11 of a 12‑hour ICU shift. One vent just alarmed, someone’s pressors are creeping up, and your phone buzzes: “Hi! Just confirming: can you make it for second look this Friday?” You’d totally forgotten you even requested it. You stare at the message and think, “There is no way in hell I can leave this service right now.”
If that’s you—on ICU, on nights, drowning in pages, and still trying to do second looks—you’re not alone. Programs assume you’re “available” because interviews are technically over. Your schedule says otherwise. Let’s get concrete about how to manage this without burning bridges or burning out.
Step 1: Decide If the Second Look Is Actually Worth It
Start here. Not with your calendar. With the brutal question: “Is this second look worth the chaos it will cause?”
You’re on ICU or night float. That means:
- Swapping is painful
- You’re exhausted
- Coverage is tight
- Sick patients do not care about your rank list
So filter your second looks hard.
Ask yourself three things for each program:
- Is this program realistically in my top 3–5?
- Am I missing critical information that will actually change my rank order?
- Do they seem like a place that values “face time” and might move me up if I show?
If you can’t say “yes” to at least 2 of those, you probably skip it.
Here’s how I’d think about it:
Second look probably worth it:
- You’re torn between two similar programs in the same city.
- You never saw the hospital or city in person.
- You had a very short or awkward interview day (virtual, rushed, bad tech).
- Faculty explicitly said: “Second looks are welcome; come see our ICU/ED/etc.”
Second look usually not worth it:
- Program is already clearly low on your list.
- You mainly want to “show interest” but you’d go there only if everyone else rejected you.
- You’re on a brutal block (ICU, nights, q2–3 call) with no realistic coverage.
You don’t get bonus points for attending every second look. You get tired. And sloppy. And more likely to screw something up with a swap.
If a program isn’t realistically moving into your top 3 after that visit, you can usually let it go.
Step 2: Understand What Kind of Second Look They’re Offering
Not all “second looks” are built the same. You need to know what you’re trying to schedule before you blow up your ICU week.
Common formats:
| Type | Time Cost | Flexibility |
|---|---|---|
| Half‑day structured visit | 3–5 hours | Low |
| Informal half‑day shadow | 3–6 hours | Medium |
| Quick tour + coffee | 1–2 hours | High |
| Evening social only | 1–3 hours | High |
| Virtual follow‑up chat | 30–60 min | Very High |
The shorter and more flexible the format, the easier it is to wedge between calls, nights, or post‑call naps.
If their invitation is vague (“come by for a second look!”), reply and get specifics before involving your chief or scheduler:
“Thank you so much for the invitation—I'd love to visit if I can make scheduling work with my ICU/night float rotation. Can you share what the second look day typically includes and the time window you’re using?”
Once you know if it’s a full morning vs a quick tour, you can realistically see where it could fit around your shifts.
Step 3: Map Your Reality – Hour by Hour
Do not guess. Pull up your actual schedule.
You’re on ICU or nights, so wiggle room comes from 3 possible zones:
- Pre‑shift window
- Example: Nights 7p–7a → you could maybe do something 1–4 p.m. if you sleep strategically.
- Post‑shift drag
- Example: Off at 7a → you might stretch and do a 9–11 a.m. thing if you can nap afterwards.
- Golden days off
- The rare true day off or post‑call day that’s not destroyed by fatigue.
Be honest about your physiology. I’ve watched people try to do this:
- Work 7p–7a
- Grab coffee
- Drive 45 minutes to program
- Second look 9a–1p
- Drive back and “nap”
- Work 7p–7a
They looked wrecked. It did not make a good impression.
If you can’t show up alert and semi‑human, skip it or push for a virtual conversation.
Step 4: Talk to Your Chiefs/Elective Director the Right Way
How you ask matters. You’re not the first to request time for interviews or second looks, but coverage is real.
First, decide if you actually need shift coverage or just shift adjustment.
- Coverage: You will be physically absent for a full shift or major portion
- Adjustment: You can flip or trade shifts to open a block of hours
Then approach your chief or scheduler with:
A narrow ask
“I’d like to attend a 3‑hour second look at Program X on [date]. The visit is from 9–12. I’m on nights that week.”A proposed plan
“If possible, I’m hoping to switch that night with [Name] or move my pre‑call day. I’ve already checked with them and they’re open to discussing it if you approve.”Evidence you’re not trying to disappear
“I’ll make sure my notes, sign‑outs, and ICU tasks are fully prepped before I go/after I return.”
Here’s a simple email template you can tweak:
Hi [Chief/Scheduler],
I’ve been invited for a second look visit at [Program] on [date]. The visit is scheduled from [time–time]. That week I’m on [ICU/night float schedule].
I’m interested in this program as one of my top choices and would like to attend if we can make coverage work. I’ve spoken briefly with [Co‑resident Name], who is willing to explore a swap on [specific shift] if you think that’s reasonable.
If this isn’t feasible given current staffing or patient volume, I completely understand and will cancel with the program. I wanted to ask before I commit or decline.
Thanks for considering this, [Your Name]
Key point: give them an easy “no.” That honesty goes a long way. And sometimes the answer really will be no on ICU or nights. You accept that.
Step 5: When You’re Really Stuck – Ask for Modifications
There’s a middle ground between “go” and “don’t go”: “go differently.”
If you cannot get clean time off, reply to the program honestly and specifically. Programs are way more flexible than applicants assume, especially if you’re transparent.
Try something like:
I’m currently on a busy ICU/night float block and it may be difficult to get a full morning off safely. I’m really interested in your program and would still love a chance to talk with residents or see a bit more of the hospital.
Would it be possible to:
– Join for a shorter portion of the second look day, or
– Do a brief late‑afternoon visit, or
– Set up an additional virtual conversation with a resident or faculty member?I don’t want to compromise patient care on my current rotation, but I also don’t want to miss learning more about your program.
You’re signaling three things:
- You actually care about the program.
- You care about patient care on your current rotation.
- You’re trying to solve the problem, not dump it in their lap.
I’ve seen PDs respond with: “Just Zoom with our chief for 30 minutes” or “Come by for coffee at 4 p.m. before your night shift.” Those are wins.
Step 6: Don’t Blow Up Your Sleep Architecture (Completely)
If you’re on nights and hell‑bent on going, you need an actual plan so you don’t show up like a zombie.
Here’s a simple pattern that works better than the “white‑knuckle wakefulness” approach:

| Category | Value |
|---|---|
| Normal Night | 8 |
| Second Look Day | 5 |
For a 9a–12p second look during nights:
- Night before:
- Work 7p–7a as usual
- Morning:
- Sleep 7:30–8:30 a.m. (power nap)
- Visit:
- Second look 9–12
- Light snack, hydrate, caffeine
- Afternoon:
- Sleep 1–5 p.m. (core block)
- Evening:
- Work 7p–7a
You’re splitting one solid sleep into two blocks. Not ideal, but safer. If you know you’re one of those people who absolutely cannot fall back asleep once you wake, this is your sign not to schedule a morning second look during nights. Aim for an afternoon visit before your shift instead.
On ICU days (7a–7p), your options are worse. Most of the time, second looks during an ICU block are simply not compatible unless you have a true day off or post‑call.
Step 7: Set Expectations With the Program So You Don’t Look Flaky
If your schedule is fragile, you need to protect your reputation up front. The worst look: cancelling last‑minute because “ICU is busy” (it’s always busy).
When confirming:
I’m excited to visit. I’m currently on an ICU/night float block, so my schedule can occasionally change at the last minute for patient care. I expect to make this work, but if anything unpredictable arises, I’ll let you know as early as possible.
You’ve:
- Flagged your situation
- Shown you understand patient care comes first
- Bought yourself some goodwill if disaster hits
If you do need to cancel:
I’m very sorry for the late change. Our ICU service has had an unexpected surge in critically ill patients and my coverage options fell through. I don’t feel comfortable leaving my team short‑staffed in this situation.
I remain very interested in your program and would still appreciate any opportunity for a brief virtual or future conversation if possible.
Reasonable programs will not punish you for this. If they do, that tells you something about them that should affect your rank list.
Step 8: Use Alternatives When You Can’t Physically Go
Sometimes you simply can’t leave. Either because:
- You’re on a no‑vacation, no‑swap block
- Coverage is unsafe
- You’re already at your human limit
Fine. That does not mean you stop gathering data.
Here’s what you do instead:
Email 2–3 residents you actually met or liked during interview day.
Ask very targeted questions:- “What surprised you about the ICU culture after you started?”
- “How do nights feel here—do you feel supported or solo?”
- “Would you pick this program again knowing what you know now?”
Ask for a brief follow‑up virtual with the PD or APD. Frame it around something specific:
- “I’m trying to decide between staying in‑state vs moving for training.”
- “I’m interested in critical care—could I talk with one of your intensivists?”
Stalk the details that matter:
- Call schedule (for interns and seniors)
- ICU structure (closed vs open, night coverage, fellow presence)
- Resident‑run vs attending‑centric culture
You’d be surprised how much you can learn in 2–3 short, focused conversations.
Step 9: Mental Math – How Much Does This Actually Move Your Rank List?
You shouldn’t be blowing up a night float schedule for every program. So ask:
- If this second look is outstanding, realistically how many spots up could this program move?
- If this second look is mediocre, how many spots down?
- What’s the cost in physical and cognitive energy?
I’ve seen people drag themselves to a second look, confirm what they already knew, and not change their rank list at all. Zero ROI.
Second looks are most powerful when:
- You’re truly stuck between 2–3 programs
- You have incomplete information (especially about resident culture)
- You need to see the city/environment in person to know if you’d be miserable
They are much less powerful when:
- You already “clicked” strongly on interview day and your gut is clear
- The program is obviously a backup geographically or academically
- You’re mainly going because you feel guilty not going
Do not trade ICU sanity for guilt.
Step 10: How to Behave on the Second Look When You’re Wiped
Let’s assume you’ve done the calculus, arranged coverage, and you’re there—sleep‑deprived but present.
A few survival rules:
Be upfront, not dramatic.
“I’m on nights/ICU this week, so I might be a tiny bit slower than usual—but I really wanted to see the program in person.”Protect your bandwidth.
Use breaks to hydrate, eat something simple, and sit down. Don’t try to be “on” every single second.Ask 2–3 high‑yield questions, not 20 scattered ones.
Good examples:- “What’s the hardest part of being a resident here that I wouldn’t see on interview day?”
- “When things get really busy in ICU/Nights, who actually shows up to help?”
- “If you had to change one thing about this program, what would it be?”
Watch how they treat residents who are clearly tired or on service.
If they roll their eyes about “complaining residents” or glorify suffering, you just got free data.
Step 11: After the Visit – Debrief Quickly While You Remember
You’ll go back to ICU or nights and your brain will flush everything that isn’t vents and vasopressors. So debrief the same day.
Right after you leave, jot down:
- 3 things you liked
- 3 things that bothered you
- Where this sits right now on your rank list (just a number)
Does not need to be formal. Just drop it in a Notes app:
Program X
- Residents seemed genuinely close, joked a lot.
- PD knew everyone’s interests in detail.
- ICU fellow seemed very hands‑on and chill.
– Call schedule rougher than described.
– ED/ICU boarders looked painful.
– Location felt more isolated than I imagined.
Current rank: #2 (above Y, below Z).
This is what you’ll come back to two weeks later when everything blurs together.
When You Absolutely Should Say No
Let me be blunt: some second looks are just not worth it while you’re on ICU or night float. Examples:
- You’d need to leave a short‑staffed ICU with 2–3 vented, unstable patients
- Your chief/scheduler looks you in the eye and says, “We really can’t lose you that day”
- Your sleep schedule is already trashed and you’re making small mistakes
- You’ve already attended multiple second looks and your rank list is basically locked
Saying “I can’t do a safe or responsible visit while I’m on ICU/nights, but I’d love to talk virtually” is a professional move. Not a weak one.
If a program can’t understand that, you’ve learned something valuable before committing 3–7 years of your life to them.
Quick Recap: What Actually Matters
Three things to hold onto:
Be selective.
Only fight for second looks at programs that can realistically jump on your rank list, not just graze it.Protect patient care and your own safety.
ICU and night float are not “optional” rotations. If you can’t leave without risking coverage or your own exhaustion, you skip or modify the plan.Communicate early and honestly—with your chiefs and the program.
Clear expectations and reasonable alternative asks (shorter visit, different time, virtual chats) will get you much further than silently suffering or cancelling at the last minute.
If you’re on a busy ICU or night float, you’re already proving you can handle real work. Do not let second looks turn into another full‑time job. Use them strategically, not reflexively.















