It is November of your MS2 year. You are buried under path and pharm, half-ignoring the constant murmur of “Step 2 matters now” from the class above you. Residency feels far away, but not that far. You keep hearing the same vague advice: “Do research,” “Get involved,” “Be a team player.” None of it tells you what to do this month, this week, today.
So let us fix that.
From mid‑MS2 to early MS3, you are laying the foundation for your residency application. Not polishing. Not peaking. Building the base you will stand on when ERAS opens. This is the 9–12 month window where smart, targeted moves compound; scattered, last‑minute flailing does not.
Below is a time‑anchored, stepwise guide: what to do, when to do it, and what can wait.
Big Picture: What “Strong Base” Actually Means
Before we go month-by-month, you need the target.
By early MS3, a competitive residency application base should include:
- Solid exam performance trajectory (Step/Level + key shelf potential)
- At least one ongoing or near-complete research/project line
- One or two meaningful clinical or service commitments (not 10 random clubs)
- Early specialty exploration with a short list of serious possibilities
- A professional reputation at your school: reliable, prepared, not a ghost
If you want a quick sense of where you must be more aggressive vs. where “average” is fine, use this:
| Target Area | Highly Competitive (Derm, Ortho, ENT) | Moderately Competitive (EM, Anes, OB) | Less Competitive (FM, Psych, Peds) |
|---|---|---|---|
| Board Performance | Top quartile, strong Step 2 | Solid pass, aim above average | Reliable pass, rising trend |
| Research Output | 2–3 projects, 1+ likely publication | 1–2 projects, poster/abstract | Any scholarly or QI project |
| Longitudinal Role | 1–2 leadership or deep involvement | 1+ consistent commitment | Some continuity (clinic, service) |
| Specialty Exposure | Shadowing + mentor in field | Shadowing + some contact | Exposure by early MS3 |
This is not perfection. This is the floor you are trying to hit by early MS3 so that the rest of MS3 and early MS4 can be about execution instead of panic.
MS2: Month‑by‑Month – From “Preclinical” to “Application‑Relevant”
November–December MS2: Quiet Setup Months
At this point you should be:
Locking in exam strategy
- Decide: Are you Step 1 pass/fail already? If yes, Step 2 will be your score signal.
- Start lifting your question bank volume slightly:
- 10–20 questions on weekdays, 20–40 on weekends.
- Not to “cram” but to build test-taking stamina and pattern recognition.
Scanning for research / scholarly projects
- Identify 2–3 departments that align with realistic specialty interests:
- Example: You think maybe IM, EM, or Anesthesia.
- Concrete action:
- Ask MS3/MS4s: “Who actually gets students on papers in [specialty] here?”
- Rank attendings by: productivity + approachability + student track record.
- Send 2–3 concise emails per week until you land at least one meeting.
- Identify 2–3 departments that align with realistic specialty interests:
Cleaning your professional footprint
- Create or fix:
- A simple, consistent email signature (MD Candidate, Class of 20XX).
- A CV draft with:
- Education
- Prior jobs
- Undergrad research
- Volunteer work
- Do not overthink formatting. But do it now so updates are painless later.
- Create or fix:
At this stage, do not join five new clubs. That is the classic mistake. One or two things you actually show up to? Fine. More than that is usually resume-padding theater.
January–February MS2: Commit and Start Producing
At this point you should be:
Formally attached to at least one project
- Goal by end of February:
- You know:
- Project title (even if working).
- Your role (data collection, chart review, manuscript drafting, etc.).
- The approximate timeline for a tangible product (abstract, poster, paper).
- You know:
- If by February you still hear only: “We’re waiting for IRB,” without any concrete tasks for you → line up a second option. IRB purgatory is how students end up with zero output.
- Goal by end of February:
Choosing 1–2 longitudinal involvements
- Good options:
- Student-run free clinic (monthly or biweekly).
- Longitudinal mentoring/tutoring (e.g., tutoring MS1s, pipeline programs).
- A defined role in a student organization (treasurer, clinic coordinator).
- Bad options:
- Six different committees where you only attend one meeting.
- Good options:
Beginning serious specialty exploration
- Narrow to 2–3 tiers:
- “Probably” (your current front-runner).
- “Backup but still like it.”
- “Reality check” / lifestyle option.
- Tactically:
- Shadow 1 half-day per month in each of 2 different fields before summer.
- Start asking residents: “What surprised you about your specialty once you started residency?”
- Narrow to 2–3 tiers:
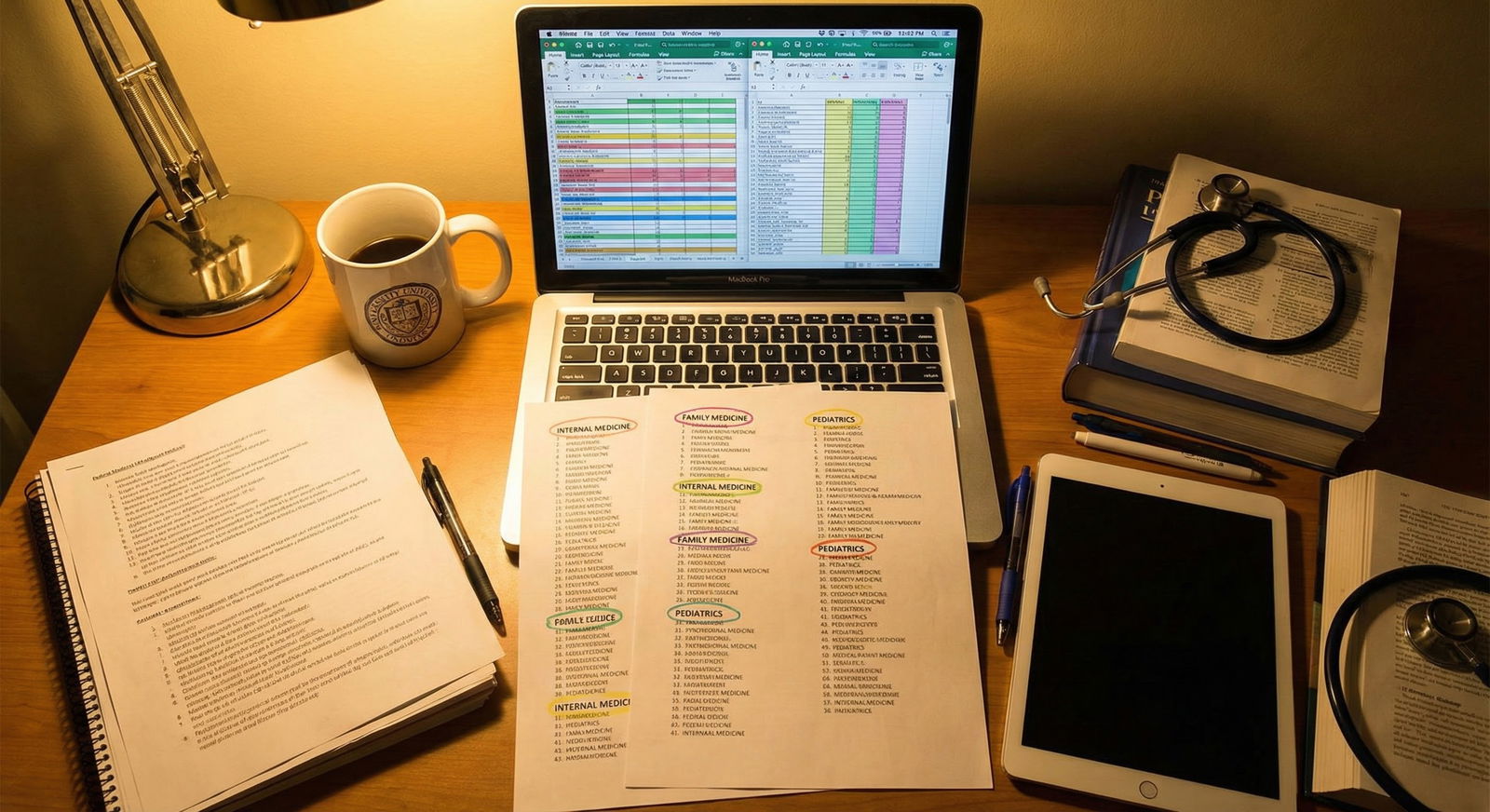
To visualize how your time should be tilting by late MS2:

| Category | Value |
|---|---|
| Coursework/Boards | 55 |
| Research/Scholarly Work | 20 |
| Clinical/Service Activities | 15 |
| Specialty Exploration | 10 |
If coursework is collapsing, pull back on extras. Passing your courses cleanly is non-negotiable. PDs do not care that you ran a clinic if you have remediation all over your transcript.
March–April MS2: Bridge to Clinical Mindset
At this point you should be:
Shifting study to clinical reasoning
- Increase UWorld or equivalent to:
- ~20–40 questions per weekday.
- Focus more on:
- Timed blocks.
- Careful post-review with emphasis on mechanisms and management, not just memorized facts.
- Increase UWorld or equivalent to:
Securing at least one near-term product
- You want something that could realistically be on your CV by early MS3:
- Case report submitted.
- Local poster abstract accepted.
- Retrospective chart review data collection nearly done.
- Press your mentor if needed:
- “I would like to aim for X conference in the fall. Is that realistic with this project?”
- You want something that could realistically be on your CV by early MS3:
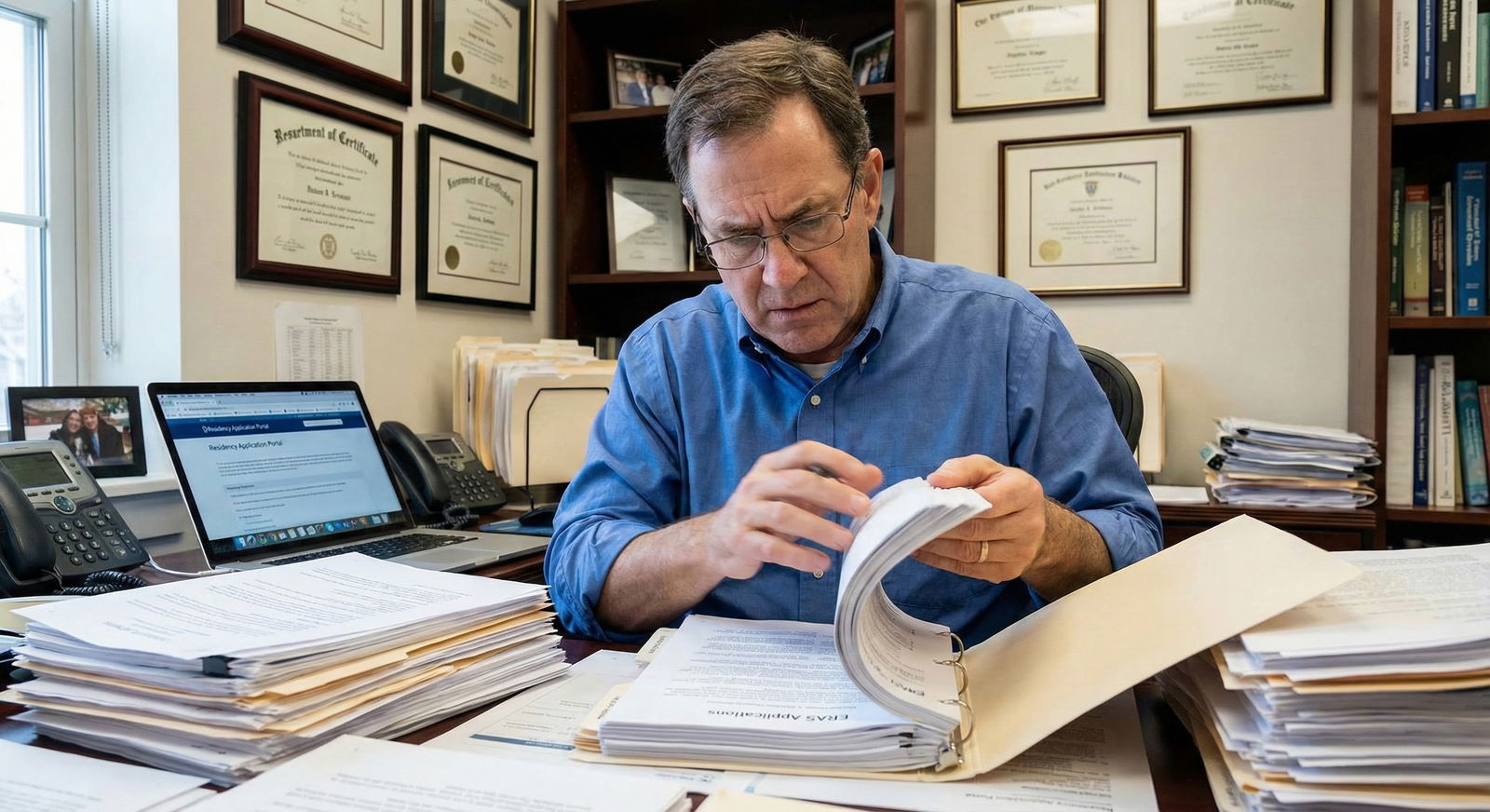
Meeting at least one potential letter-writer
- It may not be for a final LOR, but you want:
- One faculty member who knows your name.
- Has seen your work ethic on a project or in clinic/teaching.
- Ask for feedback early:
- “Are there specific skills I should focus on improving this spring so I can contribute more effectively?”
- It may not be for a final LOR, but you want:
Planning the first half of MS3 rotations intentionally
- Look at your school’s rotation order options.
- General rule:
- If you are undecided: start with broad fields (IM, FM, Surgery) to test fit.
- If leaning toward a competitive field: try to get that core or a related field before fall of MS3.
- Write down:
- What you must show on each early rotation (work ethic, adaptability, communication).
Drop any commitment that is clearly going nowhere and draining your time. Yes, even if it looks “good” on paper. Programs smell hollow involvement a mile away.
The Summer Pivot: Late MS2 to Start of MS3
Here is where people diverge sharply. Some enter MS3 with a focused, realistic plan. Others stumble in with no idea what matters.
May–June MS2: Pre‑Clerkship Prep and Reputation Seeding
At this point you should be:
Finishing MS2 strong academically
- Close out exams without drama:
- No professionalism flags.
- No last-minute absences.
- How you end preclinical is how some faculty mentally tag you. “Reliable” or “last-minute excuse generator.”
- Close out exams without drama:
Doing selective clerkship prep
- You do not need to pre-study all of medicine.
- Do:
- Basics for your first rotation:
- Read through a short clerkship handbook (e.g., De Virgilio for Surgery basics, Step-Up for IM).
- Review common orders, notes, and SOAP format.
- Basics for your first rotation:
- Get:
- One good pair of shoes.
- A simple organizational system (small notebook, template notes, etc.).
Converting spring work into actual CV entries
- Update your CV with:
- Any accepted abstracts/posters (mark as “Accepted” with venue/date).
- New roles or clinic hours (with start dates and responsibilities).
- Keep a simple “log” document:
- Date
- Activity
- Hours or products
- This makes ERAS later a copy-paste job, not an archaeological dig.
- Update your CV with:
July–September: The First 3 Months of MS3
Now you are in it. Long days, pagers, notes. This is where students often stop thinking about the application entirely. That is a mistake.
At this point you should be:
Mastering the basics of being a good MS3
- On any service:
- Show up early.
- Know your patients cold.
- Volunteer for scut within reason.
- Your main deliverable these months is:
- Strong clinical evaluations.
- Shelf scores matter, but if attendings describe you as “checked-out, disinterested,” that is far worse than a mediocre shelf.
- On any service:
Tracking your performance trajectory
- After each rotation:
- Record:
- Narrative comments.
- Grades.
- Any mid-rotation feedback.
- Record:
- Look for patterns:
- Are you repeatedly told you are quiet on rounds?
- Are your notes consistently “too long” or “disorganized”?
- Fix trends early. Do not wait until spring of MS3 when letters are already written.
- After each rotation:
Keeping at least one research or project ball rolling (lightly)
- You will not have massive time, but you can:
- Edit drafts in the evening once or twice a week.
- Do small data tasks on weekends.
- Respond quickly to mentor emails.
- Goal by early fall MS3:
- You have at least one thing that is submitted / accepted / clearly near completion.
- You will not have massive time, but you can:
Refining specialty preferences based on real experience
- After each rotation, ask yourself:
- Could I handle the worst day in this specialty repeatedly?
- Do I enjoy the bread-and-butter cases, not just the rare ones?
- Do I like the residents’ lives, not just the attendings’?
- This is not hypothetical anymore. You have data.
- After each rotation, ask yourself:
Use a simple mental scoreboard for each specialty you rotate through:

| Category | Internal Medicine | Surgery | Pediatrics |
|---|---|---|---|
| Pre-MS3 Expectation | 7 | 5 | 3 |
| After IM | 8 | 6 | 4 |
| After Surgery | 7 | 4 | 6 |
| After Peds | 7 | 4 | 7 |
No one else sees these numbers. They are just for you to avoid the “I thought I wanted X but never really compared it honestly” trap.
Week‑by‑Week Habits in Early MS3 That Pay Off Later
Now we zoom in. Because the difference between a “solid” and “standout” application is often consistency at the weekly level, not one big achievement.
Weekly Checklist (on any rotation)
Every week in early MS3, you should aim to:
Ask for micro‑feedback
- One resident or attending:
- “Is there one thing I could change this week that would make me more useful to the team?”
- Write it down. Implement it. Ask again a week later.
- One resident or attending:
Capture concrete patient stories
- Keep a de-identified list:
- Age, chief complaint, key learning point, your role.
- These become:
- Personal statement material.
- Interview answers.
- Evidence of actual reflection (PDs can tell).
- Keep a de-identified list:
Touch your scholarly work once
- Even 30–60 minutes per week:
- Editing a paragraph.
- Checking references.
- Cleaning a spreadsheet.
- Keeps momentum so you do not “lose” a whole project during MS3.
- Even 30–60 minutes per week:
Maintain your CV log
- Add:
- New teaching tasks (MS1 workshops, peer teaching).
- New roles (if you become chief of something).
- New conferences or local presentations.
- Add:
Here is a simple visual for what a “good” early MS3 week includes beyond showing up to clinic:

| Category | Value |
|---|---|
| Micro-Feedback | 1 |
| Patient Story Logged | 1 |
| Research Touchpoint | 1 |
| CV Updated | 1 |
Number “1” here = yes / completed that week. You want 3–4 bars “up” most weeks.
Day‑to‑Day: How This Feels on the Ground
To make this real, here is what a single day on an Internal Medicine rotation might look like when you are building your application base without burning out.
Sample Day: Early MS3 IM Rotation
- 5:30–6:00
- Arrive, pre-round on 2–3 patients, review overnight events and vitals.
- 7:30–11:00
- Rounds. Present confidently, take notes on decisions and teaching points.
- 12:00–12:30
- Noon conference. Write 1–2 key pearls in your notebook.
- 1:00–4:00
- Follow up labs, check in with patients, help with discharges.
- 4:00–4:15
- Ask the senior: “Is there one thing I could improve for tomorrow?”
- 5:00–6:00 (at home)
- 10–15 UWorld questions related to IM.
- 6:00–6:30
- Spend 20–30 minutes cleaning up a paragraph on your ongoing case report or checking data for your project once or twice per week.
That is it. No heroics. Just small, consistent deposits into different parts of your eventual ERAS application.
To see where these daily pieces stack up over time:

| Period | Event |
|---|---|
| Late MS2 - Identify mentors & projects | Nov MS2 |
| Late MS2 - Commit to 1-2 longitudinal roles | Jan MS2 |
| Late MS2 - Secure concrete project tasks | Feb MS2 |
| Spring MS2 - Plan MS3 rotation order | Mar MS2 |
| Spring MS2 - Aim for first abstract/poster | Apr MS2 |
| Transition to MS3 - Finish preclinical strong | May MS2 |
| Transition to MS3 - Light clerkship prep | Jun MS2 |
| Early MS3 - Focus on evaluations & shelves | Jul-Sep MS3 |
| Early MS3 - Maintain research momentum | Jul-Sep MS3 |
| Early MS3 - Refine specialty choices | Aug-Sep MS3 |
Common Mistakes in This Phase (And What To Do Instead)
You are not special. You will be tempted by the same bad ideas everyone else is.
Overloading with meaningless positions
- Mistake: Signing up as “co-chair” or “liaison” for four organizations with no actual duties.
- Better: One role with clear responsibilities and tangible outcomes (e.g., “Expanded free clinic session hours by 20%”).
Chasing last‑minute research in late MS3 instead of starting now
- Mistake: Realizing in March MS3 you have zero publications and desperately emailing 15 attendings.
- Better: Start a small but real project in MS2, even if it is just a well-done case report. Build from there.
Ignoring the impact of narrative comments
- Mistake: Focusing exclusively on shelf scores while your evaluations read “quiet, disengaged.”
- Better: Prioritize professional behavior and presence on the team. Shelf scores matter, but written comments often decide letters.
Being opaque with your mentors
- Mistake: Never telling faculty you might be interested in their specialty, then expecting them to read your mind.
- Better: Around your second contact or midway through a rotation, say: “I am seriously considering [specialty] and would value your advice on how to be a strong applicant.”
Quick Self‑Audit: Where You Should Be Now
Use this as a blunt checkpoint. If you are behind, fine—but stop pretending you are not.
By end of MS2, you should be able to say “yes” to most of these:
- I have:
- At least one active scholarly project with a clear product goal.
- One or two longitudinal roles I actually show up for.
- A draft CV that I update every few months.
- I know:
- 2–3 specialties that I am realistically considering.
- At least one faculty member or resident who knows me by name and work ethic.
By 3 months into MS3, you should also be able to say:
- I have:
- Completed at least one core rotation without professionalism issues.
- Specific positive feedback statements I could quote if asked “What are your strengths clinically?”
- At least one patient story that changed how I think about medicine.
- I am:
- Touching my research or project work at least once a week or every other week.
- Starting to see which specialties fit me, not just my Step predictions.
If several of these are “no,” do not catastrophize. Pick the easiest “no” and turn it into a “yes” in the next 2–3 weeks. Then move to the next.
FAQ (Exactly 2 Questions)
1. I am late MS2 with zero research. Is it already too late to be competitive?
No, but you no longer have time to waste on vague promises. You need projects with short timelines and clear roles. Prioritize:
- Case reports on interesting patients you can identify quickly with a willing attending.
- Retrospective chart reviews where data has largely been pulled and analysis or writing is the main task.
- Educational or QI projects tied to existing curricula or clinics.
The bar is not “Nature paper.” The bar is: Can you show that you started something, followed through, and produced a concrete scholarly product before MS4?
2. My classmates are all gunning for derm/ortho/ENT; I just want IM or FM. Do I need to do all this too?
You do not need the same volume of output, but you do need the same habits. Internal Medicine and Family Medicine programs still care about:
- Consistent clinical performance and professionalism.
- Some demonstration of intellectual curiosity (any scholarly or QI work).
- Evidence that you understand the specialty and will not burn out.
So yes, build the same base—research, involvement, self-awareness—but you can relax about squeezing three publications into 12 months. Depth and reliability will matter more for you than raw numbers.
Key points to walk away with:
- From mid‑MS2 to early MS3, your mission is to build a base: ongoing project, longitudinal role, clean academics, and realistic specialty exploration.
- Small, weekly habits—asking for feedback, logging experiences, touching your projects—compound far more than one heroic push in late MS3.
- If you are behind, do not panic. Cut dead weight, pick one concrete next step, and move. The timeline is tight, but you still have room to build something strong.



















