What’s the thing on your ERAS that makes a program director lean back, frown, and say, “We need to talk about this one”?
That’s what you’re really asking when you ask about “red flags.”
Let me be blunt: there are real red flags that sink people, there are “yellow flags” that can be managed with a good story, and there are things students think are red flags that PDs barely care about. You need to know which is which.
The Core Idea: What PDs Mean by a “Red Flag”
Program directors don’t use “red flag” for “not perfect.” They use it for: “This might hurt patients, blow up team dynamics, or make this resident unsafe or unreliable.”
So when they see something concerning, they’re asking:
- Does this suggest a pattern or a one-time issue?
- Does this touch professionalism, honesty, reliability, or safety?
- Has the applicant taken responsibility and improved, or are we seeing denial/blame?
You’re not getting rejected because you got one B in pharmacology. You’re getting rejected because your file suggests you might be difficult, unsafe, or chronically unreliable.
Let’s walk through what PDs actually consider red flags and what you can do if you have them.
High-Stakes Red Flags: The Ones That Really Matter
These are the things that routinely come up at rank meetings with language like “automatic no” or “we’d better have a very strong explanation.”
1. Professionalism Violations and Disciplinary Actions
This is the biggest category.
We’re talking about:
- Formal professionalism citations
- Unprofessional behavior reports
- Dismissal or suspension from medical school
- Being barred from clinical sites
- Police/legal issues related to behavior (assault, harassment, domestic violence)
These don’t just say “this person struggled.” They say “this person might hurt the team culture or patients.”
How PDs think about it:
- One professionalism issue, early, clearly remediated and owned? Possible yellow flag.
- Multiple issues, late in training, vague story, or blamey tone? That’s a true red flag.
- Anything involving harassment, discrimination, or lying? Huge problem.
If you have this:
- It must be disclosed honestly. Lying or “forgetting” to report something is worse than the underlying issue.
- You need a coherent, concise narrative: what happened, what you learned, proof of change.
- You want at least one letter that implicitly or explicitly says: “I trust this person’s professionalism now.”
2. Dishonesty, Misrepresentation, or “Shadiness”
Every PD I know would rather take a mediocre test taker than a dishonest superstar.
Red flags in this category:
- Inconsistencies between your application and what letter writers say.
- Exaggerated research claims (e.g., you list “first author” and the attending says you barely touched the project).
- Plagiarism in a personal statement or essay that gets caught.
- “Copy-paste” personal statements across specialties that conflict with what the program does.
- Altering grades, test scores, or dates.
Once a PD thinks “this person is dishonest,” you’re done at that program. Full stop.
If you’re tempted to stretch the truth: don’t. If you’ve already made a questionable claim, fix it now before applications go out. Better to look less impressive than untrustworthy.
3. Clinical Failure Without a Clear Recovery
Failing a core clerkship (especially IM, surgery, or OB) or being removed from a rotation gets noticed.
PDs look for:
- Pattern vs. one-off
- Specialty relevance (failing IM and applying to IM is different from failing psych and applying to radiology)
- How your school describes it in the MSPE
- Your performance after the failure
Failed Step exams and failed rotations are not equal. A failed rotation says: “On the ground, in the hospital, something went wrong enough to fail.”
If this is you:
- Don’t pretend it didn’t happen. If the MSPE mentions it, you must be ready to discuss it calmly in interviews.
- Emphasize what changed: schedule, study approach, health treatment, mentorship.
- You want strong, recent clinical letters saying: “Excellent on wards, takes feedback, no concerns about performance.”
4. Multiple Exam Failures or Big Score Drops
One failed USMLE/COMLEX attempt is common enough that many programs will at least read your file.
Multiple failures or big drops (e.g., failed Step 1, barely passed Step 2, or big downward trend in COMLEX) can scream:
- Poor test-taking ability
- Poor self-assessment or insight
- Problems under stress
That said, PDs separate:
- “Board-unstable” → Might not pass in-training exams or boards → Risk for the program’s accreditation stats.
- “Board-rescued” → Rough start but then strong Step 2, evidence of improvement, and clear explanation.

| Category | Value |
|---|---|
| 0 fails | 10 |
| 1 fail | 45 |
| 2 fails | 75 |
| 3+ fails | 90 |
If this is you:
- Step 2/Level 2 CK/CE becomes your redemption arc. You want that score as strong as you can reasonably get it.
- Have a short, non-dramatic script: “I underestimated X / studied incorrectly / had untreated condition Y. I changed A, B, C, and that’s reflected in my later performance.”
- Avoid sounding like: “The test was unfair / my school didn’t prepare me.” That reads as blame, not growth.
5. Big, Unexplained Gaps or School Changes
PDs do notice when you disappear for a year and it’s not mentioned. They also notice multiple school transfers.
What raises eyebrows:
- Year-long (or longer) unexplained gaps in training.
- Multiple leaves of absence with no clear pattern or explanation.
- Being dismissed and then re-entering another school without context.
- Transfers mid-clinical years with vague rationale.
A gap of a few months? Not a big deal. A year or two with zero explanation in ERAS and nothing in the MSPE? That’s a problem.
Acceptable narratives (if genuine):
- Medical leave (with recovery and stable current functioning).
- Significant family crisis where you were a primary caregiver.
- Visa/financial catastrophe that you stabilized.
- Personal medical condition that is now well-managed.
Unacceptable approach: “I took some time off, but I’d rather not get into it.” That’s interview poison.
Behavioral and “Vibe” Red Flags
Some red flags don’t live on paper. They show up in how you present yourself or how other people describe working with you.
6. Toxic Team Behavior and Personality Concerns
MSPEs and letters don’t say “this person is toxic.” They say things like:
- “Can be very direct; sometimes perceived as abrasive.”
- “Best when working independently.”
- “Has required more feedback on communication than most students.”
- “We discussed the importance of timeliness and follow-through.”
PDs decode that as: this student may be difficult to work with.
On the interview side, behaviors that trigger concern:
- Talking badly about your school, classmates, or faculty.
- Blaming everyone else for your problems.
- Arguing with interviewers or sounding entitled (“I deserve…”).
- Inflexible about schedules, call, locations in a demanding specialty.
If you’ve gotten feedback that “people find you harsh,” assume there’s a risk here. You can fix a lot by:
- Practicing answers out loud with someone blunt enough to call you out.
- Watching your tone when discussing negative experiences — keep it factual, not resentful.
- Emphasizing growth: “I’ve worked on…” with specific examples.
7. Poor Communication Skills (Especially for Patient-Facing Fields)
If you’re going into family med, peds, psych, EM, OB — your communication skills matter as much as scores.
Red flags:
- Incoherent personal statement.
- Clunky, confusing answers on interview day.
- Inability to clearly explain reasons for specialty choice.
- Letters hinting that you struggled with patient communication or documentation.
If English isn’t your first language, PDs don’t expect perfection, but they do expect patients and nurses to understand you. If that’s a concern, invest serious time in practicing spoken English in a clinical context.
“Soft” Application Problems That Can Act Like Red Flags
These aren’t classic red flags, but they absolutely get you filtered out or dropped on rank lists.
8. Sloppy or Generic Applications
PDs read a lot of “I just want to help people” and “ever since I was a child” garbage. You don’t get rejected for clichés alone. You get rejected when the whole application screams “low effort.”
Things that look bad:
- Personal statement clearly written for a different specialty.
- Wrong program name or city in your PS or supplemental (“I’d love to train at [OTHER HOSPITAL]…”).
- Massive typos, inconsistent formatting, half-completed sections.
- No specific reasons for interest in the program or region.
This doesn’t say “red flag” so much as “they’re not serious” or “they’re careless.” Result is the same: you drop on their list.
9. No Evidence You Understand the Specialty
Programs don’t want someone who will quit or switch because they didn’t understand the job.
Potential “yellow” flags:
- No home rotation or sub-I in the specialty you’re applying to.
- Minimal or no letters from that specialty.
- Personal statement that could apply to any field.
For competitive specialties, this can look like: “backup applicant, not committed.” For primary care fields, it’s more: “Will this person be happy with this work?”
Solution: show pattern. Electives, sub-Is, letters, relevant experiences, and a PS that clearly fits this field.
Not-Actually-Red-Flags (But You’re Probably Worried About Them)
Let me cut through some anxiety:
- One or two shelf scores below average? Not a red flag.
- Some “High Passes” instead of all “Honors”? Not a red flag.
- No research for primary care fields? Usually not a red flag.
- Being from a lower-ranked med school? Not a red flag by itself.
- Changing specialties once, early? Manageable.
These can limit your competitiveness at top programs or hyper-competitive specialties, but they’re not “why did this person fail the match?” issues.
How Program Directors Actually Process Red Flags
Here’s roughly how it plays out in real life:

| Step | Description |
|---|---|
| Step 1 | Application Received |
| Step 2 | Score/fit based review |
| Step 3 | Usually screen out |
| Step 4 | Deeper file review |
| Step 5 | Consider interview with caution |
| Step 6 | Any obvious red flags? |
| Step 7 | Safety/professionalism issue? |
| Step 8 | Evidence of growth? |
You’re not getting tossed after one glance just for being imperfect. You’re getting tossed if:
- There’s a clear major issue AND
- There’s no convincing evidence you’ve addressed it or grown from it.
When PDs defend keeping you in the pool despite a concern, they say things like:
- “Yes, they failed Step 1, but look at Step 2 and their clinical comments.”
- “They were honest and reflective in the interview about the LOA.”
- “Their letter from the PD absolutely vouches for their professionalism now.”
Your job: give them ammunition to say those things.
What To Do If You Know You Have a Red Flag
Here’s how you stop a red flag from controlling your entire narrative.
1. Classify It Honestly
Is it:
- Professionalism / behavior?
- Academic / exams?
- Health / personal life?
- Communication / team dynamics?
You need to know what bucket it falls into to address it correctly.
2. Tighten Your Story
One of the biggest mistakes I see: applicants ramble, overshare, or get defensive.
Your explanation should be:
- Brief: “Here’s what happened.”
- Accountable: “My part in this is X.”
- Concrete: “Here’s what I changed.”
- Outcome-focused: “Here’s how my later performance reflects that change.”
If you can’t explain it in under 60–90 seconds verbally, it’s too long.
3. Build a “Redemption Arc” in Your Application
You don’t fix a red flag with one sentence in your PS. You fix it with a pattern:
- Strong, recent clinical evaluations in the same domain you struggled with.
- Board scores trending up after a failure.
- Letters that explicitly mention your reliability, professionalism, or improvement.
- A personal statement that doesn’t dwell in guilt but clearly shows perspective and growth.
| Red Flag | What PDs Want to See Next |
|---|---|
| Failed Step 1 | Strong Step 2, recent solid rotations |
| Professionalism citation MS2 | Clean MS3/MS4 record, strong PD letter |
| Leave of absence for health | Stable performance after return |
| Failed core clerkship | Honors in same or related field later |
4. Choose Programs Strategically
Some programs are ultra-risk-averse. Others are more willing to take a chance on someone with a backstory and strong recent performance.
You increase your odds by:
- Applying broadly, especially to community and mid-tier academic programs.
- Targeting places that emphasize “holistic review” (and actually mean it).
- Not overreaching into hyper-elite or board-obsessed programs if you have multiple academic red flags.
What You Can Fix Right Now (And What You Can’t)
You can’t go back and erase a failure or a professionalism incident. You can absolutely:
- Stop creating new red flags with late or sloppy materials.
- Clean up your personal statement and make it specific and error-free.
- Get letters from people who know you well and can speak to your growth.
- Prepare your explanation so you don’t sound defensive or blindsided.

| Category | Value |
|---|---|
| Addressed clearly | 70 |
| Minimized vaguely | 35 |
| Ignored completely | 10 |
One More Subtle Point: Some PDs Love a Comeback Story
Not all, but some.
I’ve heard variations of: “I’d rather have the person who failed once, owned it, and clawed their way back, than the robot who’s never been tested.”
If your red flag is real, your job isn’t to pretend to be perfect. It’s to convincingly show:
- Insight: you understand what went wrong.
- Ownership: you’re not blaming everyone else.
- Change: you’ve put systems and supports in place.
- Stability: your last 12–24 months look solid.
If your recent trajectory is strong and you communicate like a grown-up, you’ll be surprised how many programs are still willing to rank you.


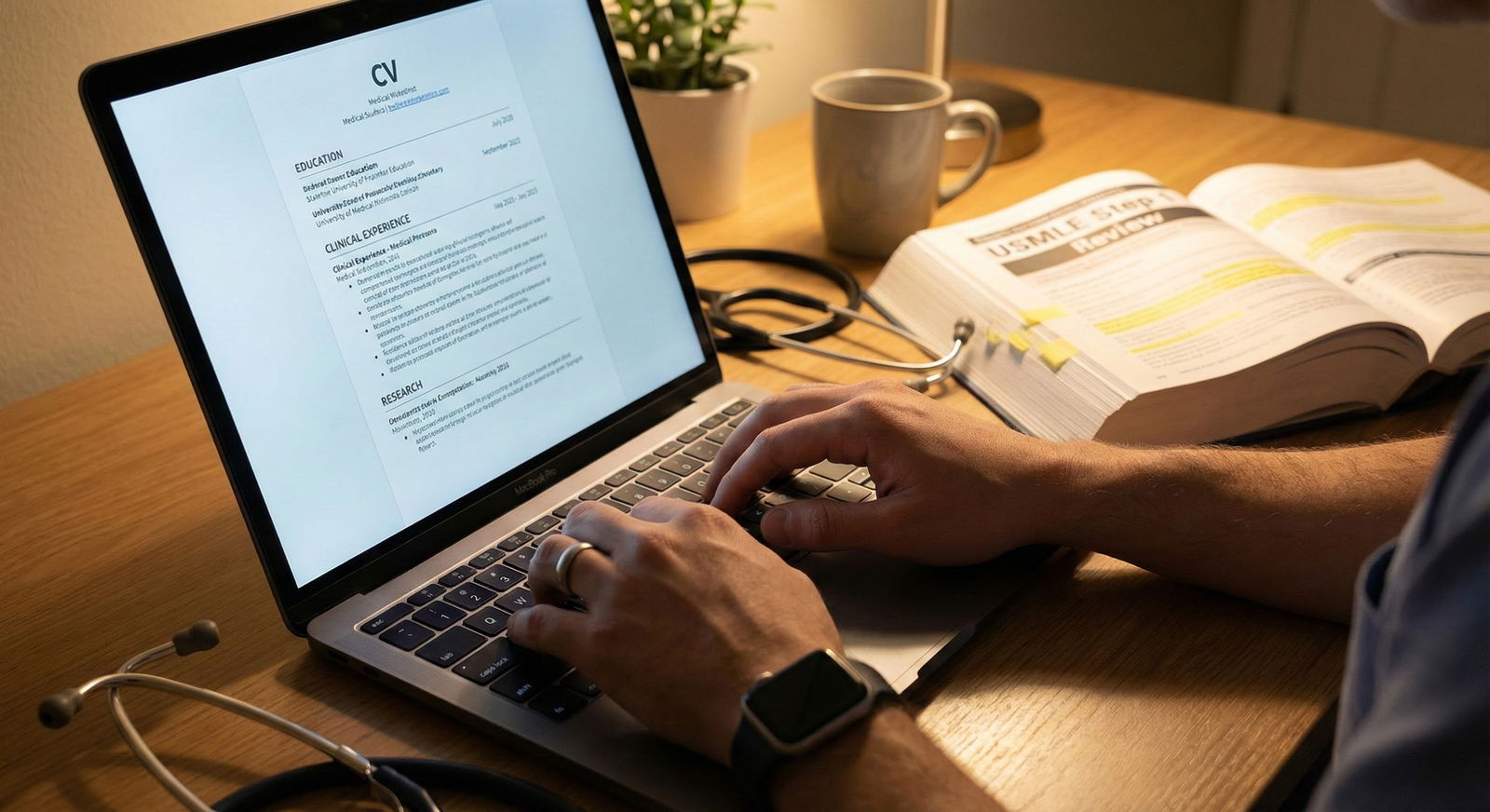
Today’s next step: open your ERAS (or whatever draft you’re using) and identify the one thing you’d most worry about if you were a PD. Write a 5–7 sentence, honest, non-defensive explanation of it. That’s your starting script—refine that before you touch anything else.



















