You’re post-call from a surgery rotation. You scrubbed four cases this week, assisted on two, and watched about eight from the corner while clutching a retractor. Somebody asks you, “So how many lap choles have you seen so far?”
You pause. Because you honestly do not know. You think… maybe six? Or was that on your last rotation?
If you are even slightly considering surgery, this is the moment to stop pretending you’ll “remember later” and start tracking your early OR case exposure like a grown-up.
Here’s how to do it right.
The Point: Why Track OR Case Exposure As A Student?
Let me cut through the fluff. As a student, no one’s going to credential you based on your case log. But tracking cases still matters for three very concrete reasons:
- You need to know what you’ve actually seen and done, not just what feels impressive in your memory.
- You’ll use it to tell specific, credible stories in personal statements, interviews, and letters.
- It trains the habits you’ll absolutely need in residency when case logs suddenly become non‑optional and audited.
I’ve seen this play out every year:
- MS3 who wants gen surg: “I love the OR; I’ve done a ton of cases.”
- Me: “Give me numbers.”
- Them: “Uh… a lot?”
That does not fly in applications, and program directors can smell vagueness from a mile away. Clean tracking = clean narrative.
So yes—you should be tracking. And you should track in a way that is:
- Fast (30–60 seconds per case)
- Consistent (same fields every time)
- Searchable (so you can pull patterns later)
Let’s build that.
What Exactly Should You Track? (Do Not Overcomplicate This)
Most students either go way too vague (“hernia surgery”) or way too detailed (full op note recreation). Both are useless.
You want a minimal data set that tells you:
- What the case was
- How you were involved
- Who can vouch for you
- What you learned
Here’s a practical template.
| Field | Why It Matters |
|---|---|
| Date | Shows recency and volume trends |
| Institution/OR | Context for where you trained |
| Attending | For letters and credibility |
| PGY level(s) | Shows team structure |
| Service/Specialty | Patterns of exposure |
| Procedure name | What you actually saw/did |
| Your role | Observer / Assistant / Primary task |
| Key skills/tasks | Concrete abilities, not buzzwords |
You can add more later if you want, but start with this core.
Concrete example entry:
- Date: 2026-01-08
- Hospital: County General, OR 4
- Attending: Dr. Lee
- Service: General Surgery
- Procedure: Laparoscopic cholecystectomy
- Your role: Assisted – camera, retraction, clipped cystic duct
- Key skills: Port placement anatomy, Calot’s triangle identification, safe clipping technique
That’s it. That’s already more than 99% of students can produce from memory six months later.
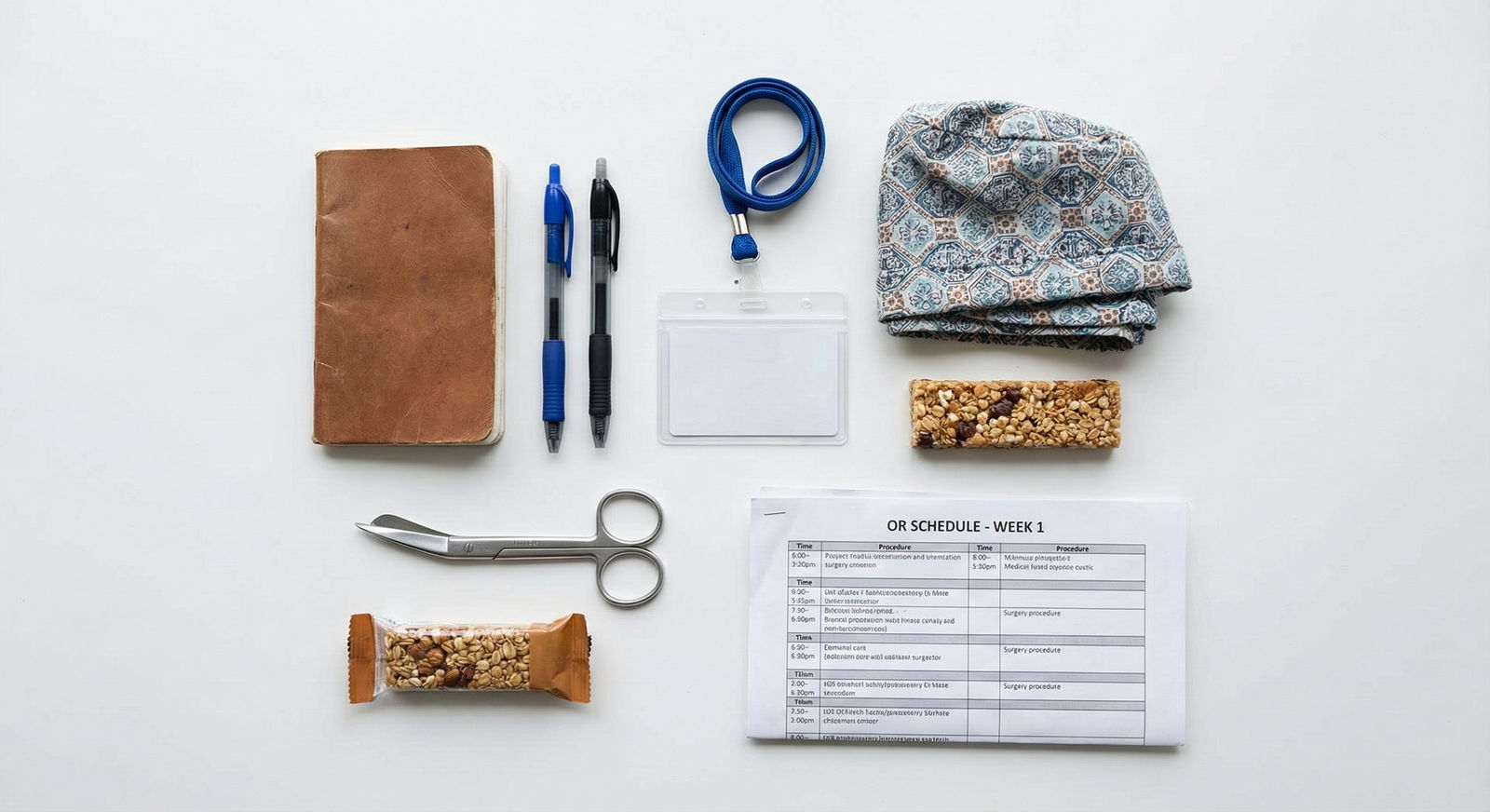
Where Should You Track It? (Apps, Spreadsheets, or Pen-and-Paper)
There is no single perfect tool. There is only the one you will actually use after a 14‑hour day when you’re hungry and annoyed.
Option 1: Notes + Later Transfer (Most Realistic)
What works best for most students:
- Immediately after the case (even in the locker room), jot quick notes in your phone:
- “1/8 CGH OR4 – Dr Lee – Lap chole – camera/retractor – Calot’s triangle teaching”
- Once a day (or once every few days), transfer these into a cleaner log (spreadsheet, Notion, etc.).
This “scratch then formal” workflow respects reality. You will not carefully fill a detailed form at 9:30 p.m. outside the OR. You will type a one-liner into your phone.
Just don’t leave it at the one-liner stage forever.
Option 2: Spreadsheet (Best All‑Around Choice)
A simple Google Sheet or Excel file is enough for the entire clinical phase.
Columns = the fields from the table above. Add filters so you can sort by service (e.g., vascular) or attending (e.g., potential letter writer).
This lets you answer questions like:
- “How many ortho cases have I actually seen?”
- “Which attendings have seen me operate more than once?”
- “Do I have any real exposure to minimally invasive vs open?”
And you can turn those into quick stats later.

| Category | Value |
|---|---|
| General | 35 |
| Ortho | 18 |
| OB/GYN | 12 |
| Vascular | 5 |
| Neurosurg | 3 |
Those numbers inside a personal statement or interview? Much stronger than “I spent a lot of time in the OR.”
Option 3: Dedicated Case Log/Note Apps
Some students love:
- Notion or Evernote templates
- Apple Notes with consistent headings
- Surgical case log apps (most are built for residents, not students, but some are usable)
My rule: if adding a case takes more than 60 seconds, you won’t keep it up during busy rotations. Test drive your system for one week. If you fall behind, it’s too heavy.
How Detailed Should You Be About Your Role?
This is where students either underplay or wildly overinflate.
Do not write “performed appendectomy” when you held a camera and cut a couple of sutures. That’s dishonest and obvious.
Break your “role” into tiers that actually reflect student reality:
- Observer – scrubbed or unscrubbed, mostly watching
- Minor assistant – retraction, suction, camera
- Active assistant – placing ports, suturing, tying, stapling, skin closure
- Performed specific step – “Closed skin,” “Stapled anastomosis under guidance,” “Cut mesentery under direction”
Log the highest level you truly achieved that case. One honest line:
“Assisted – held camera and retracted; closed two skin incisions”
Is far more credible than:
“Assisted with complex laparoscopic case”
Because when a program director asks, “What can you do in the OR right now?” you can pull real answers from your log: close skin reliably, run a bowel, handle camera in laparoscopy, basic knot tying.
That’s how you separate yourself from the “I love surgery” crowd.
How Often Should You Log? (And How Many Cases To Aim For)
Frequency matters more than volume. If you wait until the end of a 4‑week rotation to “catch up,” you’ll forget half of it.
Aim for:
- Mini‑log right after each case (in your phone)
- 10–15 minutes once or twice a week to clean up the log
As for volume: there’s no magic number, but you’re trying to build a base, not a credential file.
Reasonable exposure goals by the end of MS3 if you’re surgery‑curious:
- 30–50 general surgery cases total
- 10–20 OB/GYN (if your school has a core)
- 10–20 ortho or other subspecialties depending on rotations
Do not worship these numbers. They’re rough anchors, not requirements. But if you want to apply gen surg and your total OR log shows 12 cases at the end of MS3, something is off. Either in your exposure, or in your tracking.
What About ACGME Categories and CPT Codes?
Short answer: as a medical student, you do not need to log by CPT or ACGME case category.
That’s resident world.
If you’re extra motivated and want structure, you can loosely group cases:
- Abdominal (appys, choles, hernias, bowel resections)
- Breast/endocrine
- Vascular
- Trauma
- Ortho, etc.
But don’t waste your time trying to memorize or match ACGME minimums. They do not apply to you yet.
Your job now is to:
- Recognize common cases
- Track what you’ve seen and done
- Build patterns you can talk about coherently
You can always convert your log into more formal categories later if someone actually asks. Spoiler: they usually don’t.
How To Use Your Case Log Strategically
This is the real payoff. The log is not a sticker collection. It’s a tool.
Use it for:
1. Personal Statements
Instead of writing, “I love operating,” you can say:
“By the end of my core year, I had participated in over 40 general surgery cases, including 15 laparoscopic cholecystectomies and 7 appendectomies. What stayed with me most was…”
Specific. Credible. Anchored in reality.
2. Program Questions: “So what have you seen in the OR?”
You can answer:
“I’ve logged about 65 total cases so far. Roughly 35 in general surgery, 15 in OB/GYN, and 10 in ortho. My most hands‑on exposure has been with laparoscopic cholecystectomies and inguinal hernia repairs, where I routinely handle the camera and assist with closure.”
You sound like someone who pays attention and can be trusted with responsibility.
3. Letters of Recommendation
You can go to Dr. Lee and say:
“I’ve scrubbed 8 cases with you: 5 lap choles, 2 appendectomies, and one open hernia. In the last few I’ve been closing skin and occasionally placing ports. I’m hoping for a letter that speaks to my performance in the OR.”
That’s a much stronger ask than a vague “We worked together a lot.”
4. Career Decisions
Sometimes your log tells you the truth before you admit it.

| Category | Value |
|---|---|
| Gen Surg | 45,9 |
| OB/GYN | 18,7 |
| Ortho | 12,6 |
| Neurosurg | 4,3 |
| ENT | 6,5 |
(Each point could be [number of cases, interest rating 1–10]. If you’ve done 45 gen surg cases but rate your enjoyment at 3/10, that’s a signal.)
Your log can make it obvious you light up during certain cases and are bored in others. Listen to that.
Common Mistakes Medical Students Make With Case Tracking
Let me be blunt about what goes wrong:
Starting too late
Waiting until away rotations to start logging is a classic error. Start now, even if you only remember 10 cases from the last month.Over‑documenting, then burning out
If your system requires you to write mini‑essays, you’ll quit in a week. Stick to structured fields + one brief line of “key skills/teaching point.”Being vague about your role
“Helped with surgery” tells nobody anything. Write the most concrete action you performed.Never actually using the log
If you only collect entries and never review them, you miss half the value. Once a month, scan through and look for:- Which attendings know you best?
- What procedures have you seen the most?
- What don’t you have any exposure to yet?
Trying to impress with quantity alone
Residents and attendings are not blown away by “I logged 120 cases.” They care whether you learned anything and can articulate it.
Quick Setup Blueprint (Do This Once)
Here’s a simple, no‑nonsense way to set yourself up in under an hour:
- Create a Google Sheet called “Clinical OR Case Log.”
- Make columns:
- Date
- Hospital/OR
- Attending
- Service
- Procedure
- Role
- Key skills/teaching
- On your phone, create a pinned note called “OR scratch log.”
- After each case: write a one‑line entry in the scratch note.
- Twice a week: transfer entries into the Sheet, fleshing out “role” and “key skills.”
That’s sustainable. That’s all you need as a student.
FAQ (5 Questions)
1. Do I need to share my student case log with anyone (school, programs, etc.)?
Generally no. Medical schools rarely require formal OR case logs from students, and residency programs do not expect one. This is a personal tool. If a mentor asks for a sense of your exposure, you can share a summary (“About 50 gen surg, 15 OB/GYN”), but you do not need to hand over the raw spreadsheet unless you want feedback.
2. Should I track clinic visits or just OR cases?
If your question is specifically about OR exposure, focus on OR cases. If you’re considering a specialty and want a fuller picture of exposure (for example, clinic-heavy fields like ENT or plastics), you can add a separate tab for clinic experiences. Just don’t mix them—“OR” and “Clinic” are qualitatively different and should be logged separately if you track both.
3. How do I log combined or multiple procedures in one case?
Use the main operation that defined the case (e.g., “Lap chole with IOC” or “Open sigmoid colectomy with diverting ileostomy”). If there are truly distinct major procedures, you can either:
- List both in one line (“Lap chole + ventral hernia repair”), or
- Add two entries with the same date/attending but different “Procedure” fields.
For students, either is fine—consistency matters more than perfect categorization.
4. What if I forgot a lot of past cases—should I bother going back?
Yes, but do it aggressively approximate. Sit down for 20 minutes and write:
- “Approx 10 lap choles with Dr X on gen surg at County in Oct”
- “About 5 C‑sections on OB with Dr Y in Nov”
Then create entries like: - Date: 2025-10 (month only) – “~10 lap choles, observer/assistant”
Label them clearly as approximate. Going forward, start exact logging. Imperfect historical data is still better than nothing.
5. Will residency programs actually care that I tracked cases as a student?
They won’t care about the file itself; they will care about the kind of applicant it makes you. A student who can say, “I’ve logged about 70 OR cases, mostly gen surg and OB, and I’ve been closing skin and handling the camera regularly” sounds concrete and prepared. The log is invisible evidence that you’re organized, honest about your skill level, and serious about surgery. That does get noticed.
Open a notes app right now and title a new note “OR scratch log.” Next time you walk out of the OR, before you check your phone for messages, type one line about the case you just saw. That’s the habit that builds everything else.




















