The way most students memorize microbiology buzzwords for Step 1 is lazy—and it is exactly why they miss the harder questions.
Buzzwords are not the problem. Treating them as trivia is.
If you stop at “rose spots = Salmonella Typhi” and never wire that to virulence factors, immune evasion, and organ-level pathology, you will get crushed by two-step and three-step vignettes. Step 1 now lives in that space: mechanism-heavy, system-integrated, and much less forgiving of shallow recall.
Let me walk you through how to convert microbiology buzzwords into mechanisms, and then into reliable answer choices. Pattern recognition with teeth.
1. How Step 1 Actually Tests Microbiology Now
Step 1 no longer asks, “What is the organism?” as often as before. It asks:
- Why is this patient’s lab abnormal?
- What specific virulence factor explains this symptom?
- What is the most likely complication, given this micro–host interaction?
- Which drug or deficiency made them susceptible?
Buzzwords are still there, but they are bait. They hint at a mechanism you must know cold.

| Category | Value |
|---|---|
| Organism ID only | 10 |
| Organism + virulence/mechanism | 45 |
| Organism + treatment/resistance | 25 |
| Host factor/immunity focus | 20 |
You want to train your brain like this:
- Hear buzzword → immediately call up organism.
- From organism → pull its structure, virulence factors, and key host response.
- From mechanism → predict labs, complications, drugs, and risk factors.
If you are only doing step 1 of that chain, you are doing pre-2010 Step 1 prep in 2026.
2. Gram-Positive Patterns: Toxins, Shapes, and Immune Evasion
Let me break down the high-yield Gram-positives by their “pattern” on exams, and how to immediately pivot from buzzword to mechanism.
Staphylococcus aureus – From Abscess to Toxin Logic
Buzzwords people memorize:
- Catalase positive, coagulase positive
- Clusters of Gram-positive cocci
- Golden colonies
- Post-influenza pneumonia
- Rapid-onset vomiting after picnic mayonnaise
What Step 1 is really asking you about:
- Protein A (binds Fc region of IgG) → prevents opsonization and phagocytosis.
- Coagulase → fibrin clot formation, walls off abscesses.
- Toxins:
- Exfoliative toxin → scalded skin syndrome (targets desmoglein-1).
- Toxic shock syndrome toxin-1 (TSST-1) → superantigen → massive T-cell activation → cytokine storm.
- Enterotoxins (preformed) → rapid food poisoning (1–6 hours).
Mechanism bridge example:
- Vignette: Woman with tampon use, fever, hypotension, diffuse erythematous rash involving palms and soles, subsequent desquamation.
- Buzzword: Tampons, diffuse rash, hypotension.
- Organism: S. aureus.
- Mechanism Q: What is the mechanism of the toxin?
- Answer: Cross-links MHC II and T-cell receptor outside the antigen-binding site → polyclonal T-cell activation → IL-1, IL-2, IFN-γ, TNF-α surge.
You must have that superantigen mechanism ready to deploy, not just “TSST-1 = S. aureus”.
Streptococcus pyogenes (Group A Strep) – M Protein and Immune Confusion
Step 1 loves GAS for three reasons: molecular mimicry, post-infectious disease, and exotoxins.
Buzzwords:
- Bacitracin sensitive
- PYR positive
- Honey-colored crusted lesions (impetigo)
- Sandpaper rash, strawberry tongue
- “Flesh-eating bacteria” – necrotizing fasciitis
Mechanism points:
- M protein:
- Major virulence factor.
- Anti-phagocytic.
- Molecular mimicry with human myosin → rheumatic fever (mitral > aortic).
- Streptolysin O:
- Oxygen-labile, hemolysin.
- Basis for ASO titer → post-strep diagnosis.
- Exotoxin A (superantigen) → scarlet fever, toxic shock-like syndrome.
- Immune mechanisms:
- Post-strep glomerulonephritis: immune complex deposition (type III).
- Rheumatic fever: type II hypersensitivity (antibody-mediated cytotoxicity).
Exam connection:
- If they give you a child with hematuria and periorbital edema after impetigo, they are testing:
- GAS impetigo → nephritogenic strains → immune complexes in glomeruli → complement consumption (↓ C3).
- This is not the same as rheumatic fever mechanism.
So when you see “sandpaper rash” and “strawberry tongue,” you should mentally hold:
- Superantigen toxin (exotoxin A) → widespread cytokine release.
- But long-term sequelae (like rheumatic heart disease) are due to M protein antibodies. Different mechanisms, same bug.
Streptococcus pneumoniae – Capsule and IgA Protease
Buzzwords:
- Lancet-shaped, Gram-positive diplococci
- Optochin sensitive, bile soluble
- Rusty sputum
- “Most common cause of community-acquired pneumonia / meningitis in adults / otitis media in children”
- Splenectomy risk
Mechanism bridge:
- Polysaccharide capsule:
- Anti-phagocytic.
- Asplenic patients (sickle cell, surgical splenectomy) lose splenic clearance → recurrent infections.
- IgA protease:
- Cleaves secretory IgA.
- Aids mucosal colonization (nasopharynx) → pneumonia, sinusitis, otitis media.
When Step 1 asks: “Which virulence factor allows this organism to colonize the nasopharynx?” for a community pneumonia vignette, answer is IgA protease, not “capsule” (which is more about survival in the bloodstream and evasion of phagocytosis).
3. “Classic Buzzword Organisms” Rewired by Mechanism
You already know the names. The question is whether you know what they actually do.
Neisseria: IgA Protease, LOS, and Complement
Neisseria meningitidis and N. gonorrhoeae share some core features.
Shared buzzwords:
- Gram-negative diplococci, kidney-bean shaped.
- Oxidase positive.
- Produce IgA protease.
Differences:
- N. meningitidis:
- Maltose + glucose fermentation.
- Capsule.
- Waterhouse–Friderichsen (adrenal hemorrhage, DIC, shock).
- N. gonorrhoeae:
- Glucose only.
- No capsule.
- Antigenic variation of pili → recurrent infection, no long-term immunity.
Mechanism they love:
- Complement deficiency (C5–C9) → recurrent Neisseria bacteremia.
- So if you see a teenager with repeated episodes of Neisseria infections, they are asking about MAC (membrane attack complex) defects.
Host–pathogen bridge:
- LOS (lipooligosaccharide) triggers TNF-α → septic shock.
- IgA protease allows colonization of mucosa (nasopharynx for meningitidis, genital tract for gonorrhoeae).
If they show you a purpuric rash, hypotension, and bilateral adrenal hemorrhages, they might ask:
- Why is this patient particularly susceptible? Answer: Terminal complement deficiency.
- What factor of the organism causes the shock? Answer: LOS, not “exotoxin”.
Listeria monocytogenes – Intracellular Actin Rockets
Buzzwords:
- Tumbling motility.
- Intracellular movement via “actin rockets”.
- Contaminated unpasteurized dairy, soft cheeses.
- Neonatal meningitis, meningitis in immunocompromised.
- Grows at cold temperatures (cold enrichment).
Mechanism:
- Facultative intracellular:
- Escapes phagolysosome into cytoplasm.
- Uses host actin polymerization to move from cell to cell, avoiding extracellular exposure.
- Cell-mediated immunity crucial:
- T-cell and macrophage response.
- Impaired in neonates, elderly, pregnant women, immunosuppressed → susceptibility.
Bridge:
- So if they ask about “defense mechanism most important in clearing this organism,” answer is T-cell–mediated immunity / intracellular killing, not antibody.
That “actin rocket” buzzword should automatically trigger: intracellular, cell-mediated immunity, risk in T-cell defects and pregnancy.
4. Toxin-Driven Organisms: From Buzzword to Biochemistry
These are the questions that separate memorization from understanding. Toxin questions are almost always mechanism questions.
Corynebacterium diphtheriae – EF-2 and Pseudomembranes
Buzzwords:
- Grayish pseudomembrane in throat.
- Severe pharyngitis, bull neck.
- Immigrant child without vaccinations.
- Elek test for toxin.
Mechanism:
- Diphtheria toxin:
- Inactivates elongation factor-2 (EF-2) via ADP-ribosylation.
- Halts host protein synthesis.
- Necrosis in pharynx → pseudomembrane.
- Systemic effects → myocarditis, arrhythmias, neuropathies.
Step 1 style:
- They might show a child with pharyngitis, cardiac arrhythmia, and a history of not being vaccinated and then ask:
- “The toxin produced by this organism acts through which mechanism?”
- Answer: ADP-ribosylation of EF-2 → inhibition of protein synthesis.
- “The toxin produced by this organism acts through which mechanism?”
You must connect “pseudomembrane” and “vaccine-preventable pharyngitis” to fundamental protein synthesis biochemistry.
Clostridium botulinum vs. C. tetani – Same Target, Different Direction
Both toxins hit SNARE proteins and block neurotransmitter release. But Step 1 wants directionality.
Buzzwords:
- C. tetani:
- Puncture wound.
- Lockjaw (trismus), risus sardonicus, opisthotonus.
- C. botulinum:
- Floppy baby, honey ingestion.
- Diplopia, dysphagia, descending paralysis.
- Canned foods.
Mechanism:
- Tetanospasmin:
- Blocks release of inhibitory neurotransmitters (GABA, glycine) from Renshaw cells in spinal cord.
- Disinhibition → sustained muscle contraction (spastic paralysis).
- Botulinum toxin:
- Blocks release of ACh at neuromuscular junction.
- Leads to flaccid paralysis.
Pattern:
- Both: proteases that cleave SNARE proteins required for vesicle fusion.
- Exam Q: “Which neurotransmitter is affected?” or “Which mechanism explains their symptoms?”
You see “floppy baby” → infant botulism → honey ingestion → underdeveloped gut flora → spores germinate → toxin production → presynaptic blockade of ACh release.
Vibrio cholerae and ETEC – cAMP and Secretory Diarrhea
If you do not immediately see “hypersecretion” when you read “Gs activation,” fix that now.
Vibrio cholerae:
- Buzzwords:
- Profuse rice-water diarrhea.
- Contaminated water, natural disaster, developing regions.
- Mechanism:
- Cholera toxin permanently activates Gs → ↑ adenylate cyclase → ↑ cAMP.
- Increased Cl⁻ secretion via CFTR in gut and decreased Na⁺ reabsorption → massive watery diarrhea.
Enterotoxigenic E. coli (ETEC):
- LT (heat-labile) toxin:
- Like cholera, activates Gs → ↑ cAMP.
- ST (heat-stable) toxin:
- Activates guanylate cyclase → ↑ cGMP → decreased NaCl reabsorption.
Step 1 angle:
- You will see questions like: “A toxin produced by this organism increases cAMP levels in enterocytes. What is the effect on ion transport?”
- You answer: Increased Cl⁻ secretion and decreased Na⁺ reabsorption.
The pattern: watery (secretory) diarrhea + “travelers” + mechanism = cAMP/cGMP changes.
5. Fungi and Parasites: Buzzwords Tied to Host Immunology
Students either over-memorize random species or under-learn the immune patterns. You should focus on classic path + immune defect.
| Host Issue | Organism Pattern | Mechanism Focus |
|---|---|---|
| Neutrophil dysfunction (CGD) | Catalase-positive bugs | H₂O₂ handling, oxidative burst |
| T-cell deficiency (HIV, steroids) | Intracellular (TB, fungi, Listeria) | Cell-mediated immunity failure |
| Asplenia (sickle, surgical) | Encapsulated bacteria | Impaired opsonization, splenic clearance |
| Complement C5–C9 deficiency | Neisseria | Impaired MAC |
Candida vs. Aspergillus – Pattern of Disease = Mechanism
Candida:
- Buzzwords:
- Thrush in HIV (CD4 < 200).
- Esophagitis in severely immunosuppressed (CD4 < 100).
- Diaper rash.
- Immunity:
- Local mucocutaneous infection: T-cell mediated immunity (HIV, steroids).
- Systemic candidemia: neutrophils.
Aspergillus:
- Buzzwords:
- Acute-angle branching, septate hyphae.
- Neutropenic patient.
- “Fungus ball” in old TB cavity.
- Allergic bronchopulmonary aspergillosis (asthmatics, CF).
Mechanism:
- Strongly associated with neutrophil dysfunction (chemotherapy, chronic granulomatous disease).
- Invades blood vessels → infarction, hemorrhage.
If they give you a neutropenic leukemia patient with fever and pulmonary nodules, your brain should go right:
- Neutrophil defect → Aspergillus risk → angioinvasive fungus → hemoptysis, infarction.
Protozoa with Pathognomonic Buzzwords That Mean Mechanism
Toxoplasma gondii:
- Buzzwords:
- Ring-enhancing lesions in HIV patient with low CD4.
- Raw meat, cat feces, congenital triad (chorioretinitis, hydrocephalus, intracranial calcifications).
- Mechanism:
- Intracellular protozoan → cell-mediated immunity crucial.
- Reactivation in AIDS when CD4 plummets → brain abscesses.
Plasmodium falciparum:
- Buzzwords:
- Irregular fever spikes.
- Cerebral malaria.
- Banana-shaped gametocytes.
- Mechanism:
- Infected RBCs adhere to capillary endothelium due to surface proteins → microvascular occlusion.
- Brain, kidney, lungs at risk.
So when you see travel to Africa, hemolysis, anemia, periodic fevers, you also think:
- Hemoglobinopathies (e.g., sickle trait) protect by altering RBC environment → impaired parasite growth.
6. Step 1–Style Mechanism Qs Built on Buzzwords: Concrete Examples
You need to see how these questions are actually written.

| Step | Description |
|---|---|
| Step 1 | Recognize Buzzword |
| Step 2 | Identify Organism |
| Step 3 | Recall Key Virulence/Structure |
| Step 4 | Map to Host Response or Defect |
| Step 5 | Predict Labs/Complication/Drug |
Example 1: Gram-Positive Rod and Neurologic Symptoms
Vignette:
- A 3-month-old infant presents with constipation, poor feeding, and generalized weakness. The parents mention they have been giving the baby homemade honey. Physical exam shows hypotonia (“floppy baby”). EMG shows decreased compound muscle action potentials with repetitive stimulation. Which of the following best describes the mechanism of the toxin responsible for this condition?
Buzzwords → Organism:
- Floppy baby + honey → infant botulism → Clostridium botulinum.
Mechanism choices likely:
- A. Blocks release of inhibitory neurotransmitters in spinal cord.
- B. Inactivates EF-2 via ADP-ribosylation.
- C. Blocks release of acetylcholine at neuromuscular junction.
- D. Degrades cell membranes via lecithinase.
Correct:
- C. Blocks release of ACh at neuromuscular junction.
Bridge:
- You did not just see “honey” and circle “C. botulinum.” You linked it to presynaptic blockade of ACh and flaccid paralysis.
Example 2: Encapsulated Organism in Asplenic Patient
Vignette:
- A 25-year-old man with sickle cell disease presents with fever, productive cough, and pleuritic chest pain. Sputum Gram stain shows Gram-positive, lancet-shaped diplococci. He is treated appropriately but is at high risk for future infections with similar organisms. Loss of which of the following functions explains his susceptibility?
Buzzwords:
- Sickle cell disease → functional asplenia.
- Gram-positive, lancet-shaped diplococci → Streptococcus pneumoniae.
Mechanism they want:
- Spleen’s primary job in this context is to clear opsonized encapsulated organisms. They are testing:
- Impaired clearance of opsonized bacteria (particularly encapsulated) due to absence of splenic macrophages and marginal zone B-cell function.
Wrong choices will say:
- Decreased neutrophil chemotaxis.
- Decreased IgA production.
- Decreased complement synthesis (liver does that).
Correct conceptual link:
- Asplenia → risk of encapsulated organisms: S. pneumoniae, H. influenzae type b, Neisseria meningitidis, etc.
7. How to Study Micro for Mechanisms, Not Just Flashcards
Let me be very specific because I have watched people waste months here.
Strategy 1: For Every Organism, Build a “Mechanism Card,” Not Just a Name Card
For each pathogen:
- Structure:
- Gram status, shape, capsule, spores, envelope (for viruses).
- Reservoir and transmission.
- Virulence factors and their precise mechanism.
- Host immune response: what arm of the immune system matters most?
- Classic risk factors and host defects (HIV, neutropenia, asplenia, complement deficiency).
- Hallmark clinical disease patterns.
- One to two key complications.
Example for S. aureus, on a single side:
- Protein A → binds Fc of IgG → no opsonization.
- Coagulase → fibrin clots → abscess formation.
- TSST-1 → superantigen → massive cytokine release → hypotension, rash.
- Post-influenza pneumonia.
- MRSA → altered PBP (mecA) → β-lactam resistance.
You drill this, then the buzzwords become doors to mechanisms, not dead-end facts.
Strategy 2: Group Organisms by Shared Mechanism or Virulence Theme
Stop studying them alphabetically. Study like this:
- Superantigen producers:
- S. aureus (TSST-1), S. pyogenes (exotoxin A, C).
- ADP-ribosylating toxins that inhibit protein synthesis:
- Corynebacterium diphtheriae (EF-2), Pseudomonas aeruginosa exotoxin A (EF-2).
- cAMP mediators:
- Vibrio cholerae, ETEC (LT), Bordetella pertussis (inhibits Gi).
- Intracellular pathogens (cell-mediated immunity):
- Listeria, Mycobacteria, Salmonella Typhi, many viruses, Toxoplasma.

| Category | Value |
|---|---|
| Superantigen producers | 2 |
| Protein synthesis inhibitors | 3 |
| cAMP-modulating toxins | 3 |
| Capsulated bacteria | 5 |
| Intracellular pathogens | 6 |
When you group like this, questions that feel “new” on test day actually look like old friends with new clothes.
Strategy 3: Tie Every Buzzword in First Aid/Sketchy Back to One Mechanism
If you cannot answer “What specific mechanism makes this true?” for each cute visual or phrase, you do not actually know it.
- “Satellitism” (H. influenzae growing near S. aureus):
- Needs factor V (NAD⁺) and factor X (heme) → S. aureus provides factor V via hemolysis.
- “Currant jelly sputum” (Klebsiella):
- Massive inflammation and necrosis due to thick polysaccharide capsule, aspiration in alcoholics → hemorrhagic mucus.
This is the difference between passive watching and active wiring.
FAQ (Exactly 5 Questions)
1. Do I still need to memorize all the classic microbiology buzzwords for Step 1?
Yes, but only as entry points. Buzzwords are hooks; they are not the content. You must use each buzzword to immediately recall the organism, its key virulence factors, and how it interacts with the host immune system. If you cannot connect “floppy baby” to presynaptic blockade of ACh and SNARE cleavage, you have not gone far enough.
2. How much pure organism identification does Step 1 still test?
There are still straightforward ID questions, but they are a minority. Most questions use organism ID as a starting point and then ask about mechanism, complications, treatment, or host risk factors. Expect two- and three-step questions like “organism → virulence factor → clinical consequence,” not isolated “name the bug” trivia.
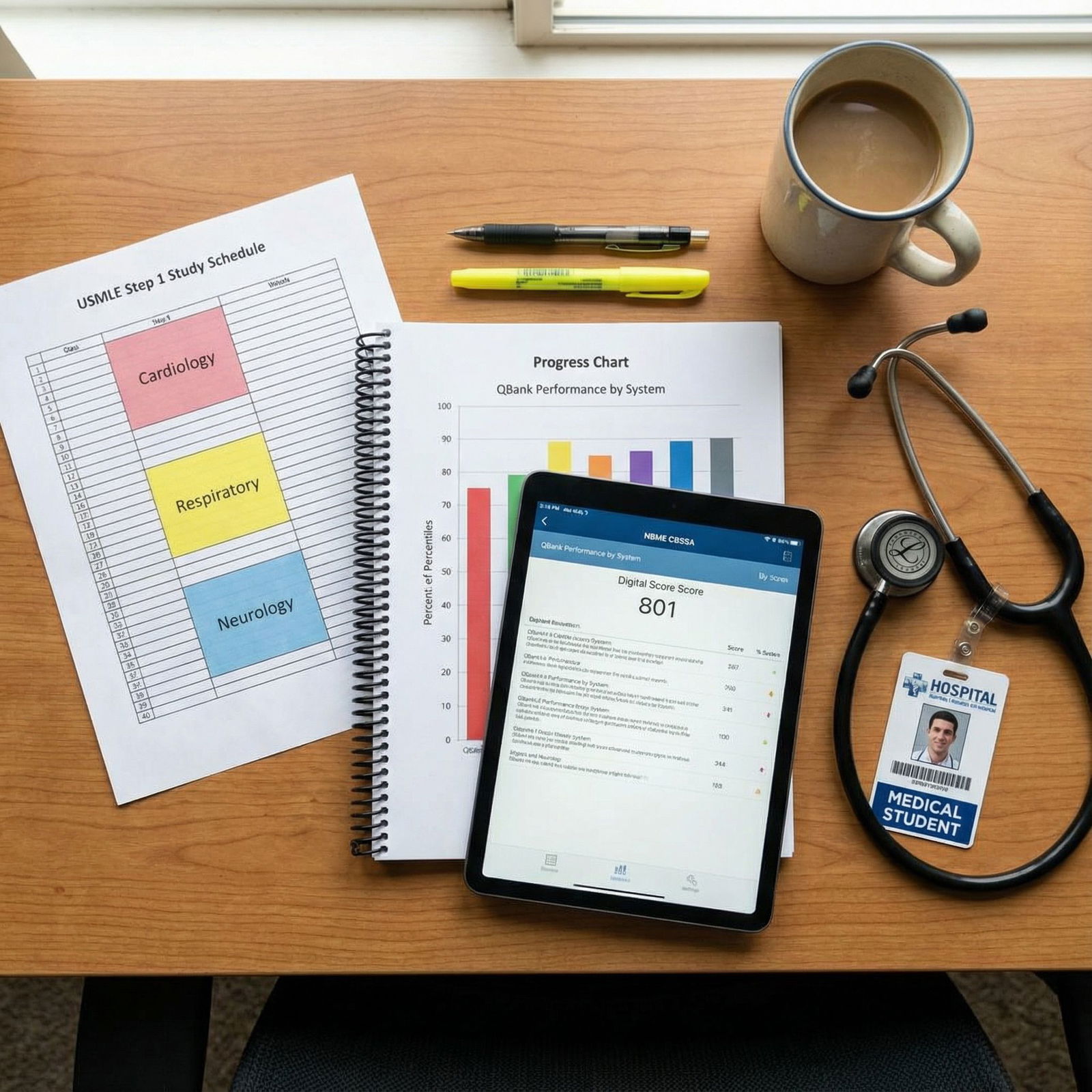
3. What is the single highest-yield way to review micro in the last month before Step 1?
Stop adding new bugs. Instead, take the top ~40 organisms that show up everywhere (S. aureus, S. pyogenes, S. pneumoniae, Neisseria, Listeria, TB, E. coli, Pseudomonas, Clostridium species, major viruses, etc.) and for each one, write out:
- One-line ID.
- One-line main virulence factor and mechanism.
- One-line key host defect or risk factor.
- One-line hallmark disease pattern. Drill that repeatedly with timed questions (UWorld/Amboss) to force the mechanism recall under pressure.
4. How do I integrate immunology with microbiology for better pattern recognition?
Any time you see a host defect—HIV with low CD4, neutropenia from chemo, asplenia, complement deficiency—ask yourself which broad micro groups that selects for. Train on those patterns. For example, T-cell defects → intracellular pathogens and fungi; neutrophil defects → catalase-positive bacteria and Aspergillus; asplenia → encapsulated organisms. Then, when a vignette gives you the immunologic problem, you are already halfway to the organism and the expected complications.
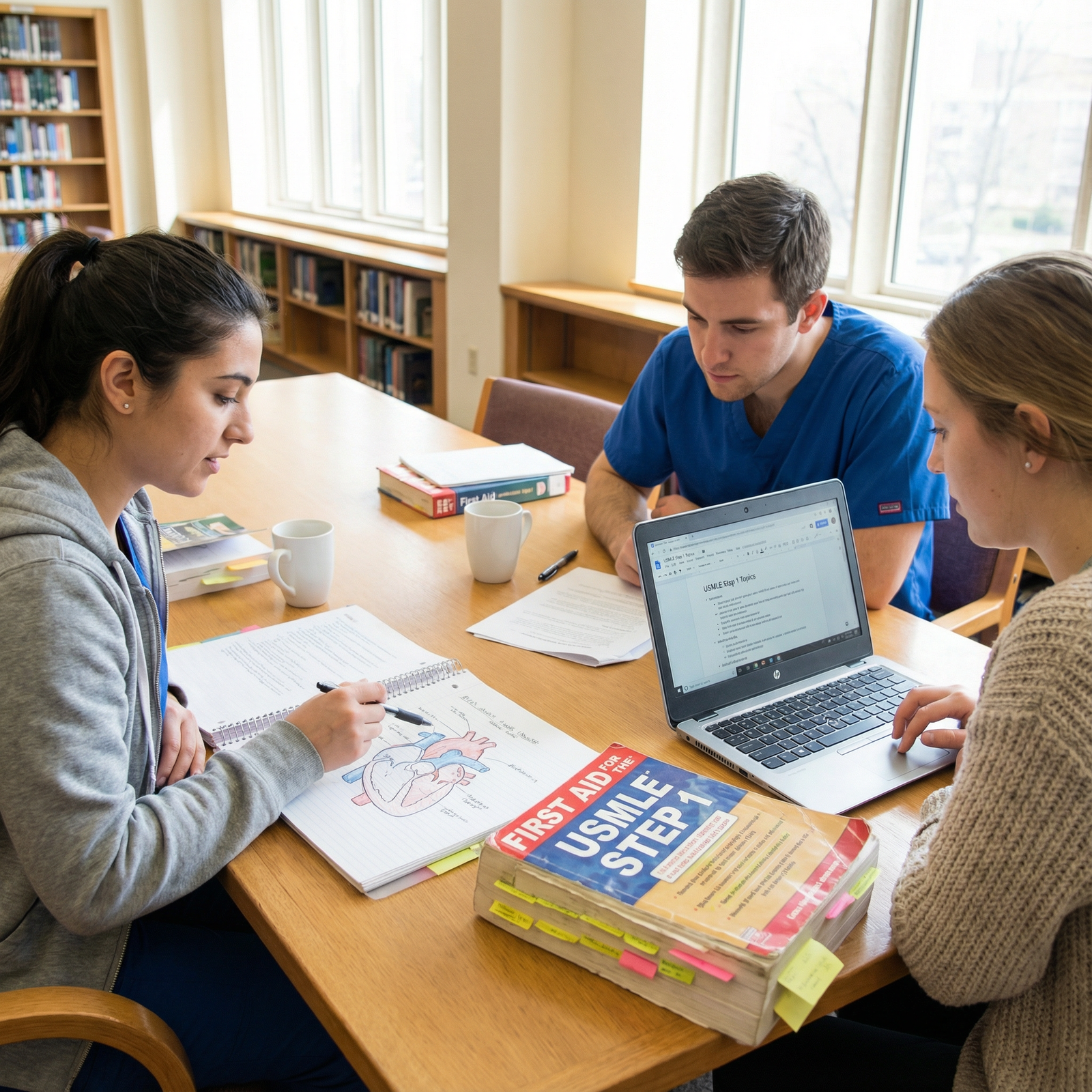
5. Are Sketchy/visual resources enough for mechanism-level micro questions?
They are a strong foundation, but not sufficient alone. Visual mnemonics give you the list of virulence factors and disease associations. You still need to explicitly connect each image element to its biochemical or immunologic mechanism using text-based resources (First Aid, Pathoma micro sections, UWorld explanations). The students who crush micro are the ones who watch Sketchy, then immediately annotate each story with “how” and “why” in words—not just “what.”
Key takeaway 1: Buzzwords are signals, not answers. For every classic phrase or image, know the organism, its virulence factor, and the exact mechanism in the host.
Key takeaway 2: Study micro by mechanisms and host defects—superantigens, cAMP, intracellular survival, encapsulation—so unfamiliar vignettes collapse into familiar patterns on test day.



















