The way most clinicians “crash” after nights is not just suboptimal. It is dangerous.
You know this already. The problem is not that you are unaware; the problem is that the system normalizes cognitive impairment and emotional dysregulation after consecutive night shifts as if they are personality traits instead of predictable physiological outcomes. What you have been missing is a structured, repeatable protocol for the 90–120 minutes after your final night that treats sleep transition like a clinical procedure, not an afterthought.
Let me walk you through it.
Why You Need a Protocol, Not Just “More Sleep”
After 3–5 consecutive nights, three things are happening simultaneously:
- Circadian misalignment
- Sleep pressure overload (homeostatic drive)
- Emotional and ethical vulnerability
Most people talk about the first two. The third one almost never gets named, yet it is the one that quietly corrodes professionalism and empathy.
You finish a string of nights and you are:
- More irritable with nurses, consultants, and yes, patients
- More likely to cut ethical corners (“I will defer that conversation,” “I am not calling the family now”)
- More prone to moral injury because you see yourself doing these things and feel powerless to stop
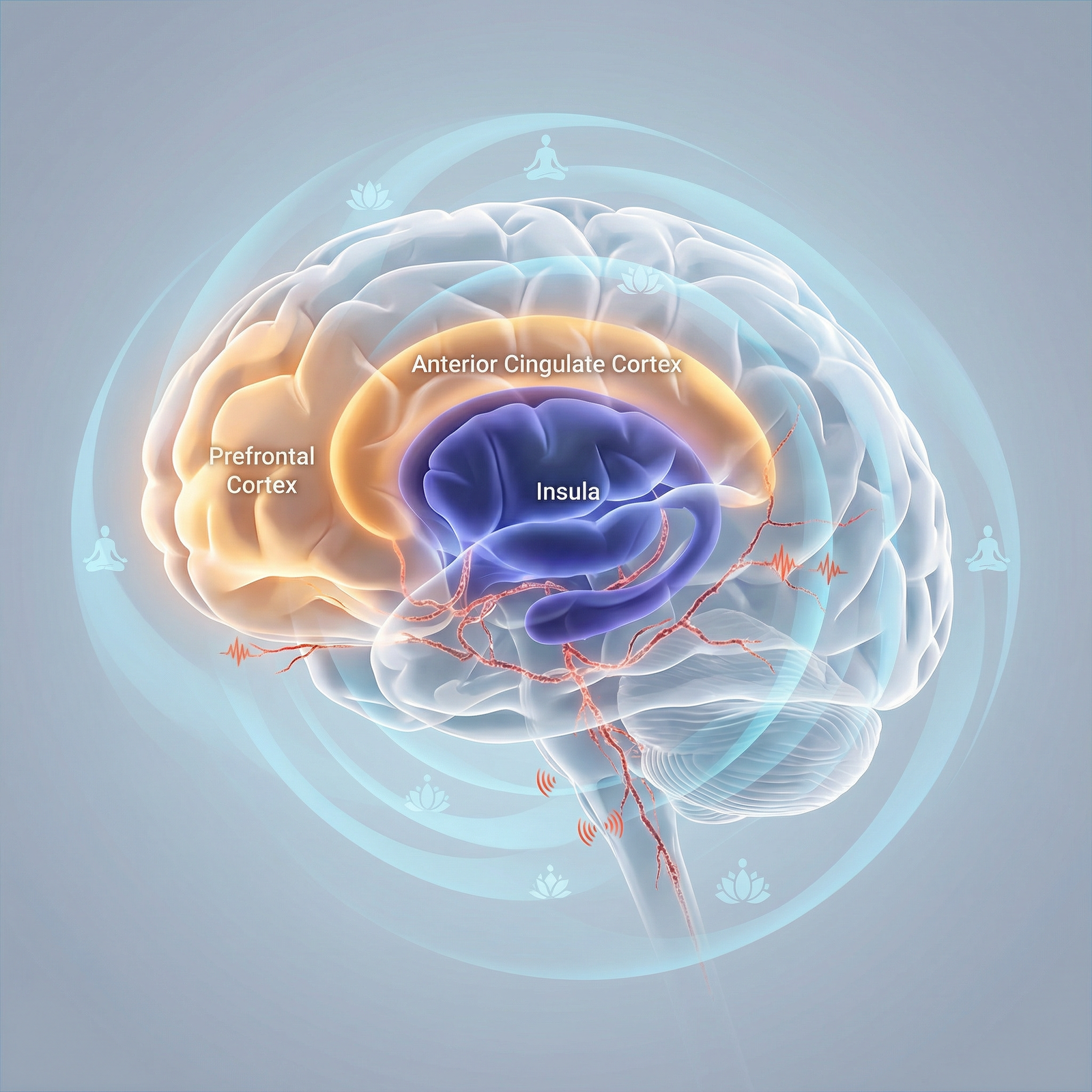
Sleep-transition mindfulness is not about being calm and spiritual. It is about reducing the lag between “off shift” and “restorative sleep,” and redesigning that window so you:
- Protect your immediate sleep quality
- Discharge built-up emotional load safely
- Reset your ethical compass before re-entering your normal life
That is the frame. You are not doing self-care. You are performing cognitive and ethical maintenance on a fatigued brain.
The Core Concept: Sleep‑Transition Windows
Think of the post-night period in three discrete windows:
- T0–15 minutes: Decompression and disengagement from clinical mode
- T15–45 minutes: Mind–body downshift, physiological braking
- T45–120 minutes: Protected pre‑sleep corridor and ethical reset
You will not always get the full 120 minutes. Fine. But you need a default structure that you can compress rather than improvising from scratch every time.
Here is a visual of a realistic 90‑minute version for a typical resident finishing at 8:00 AM:

| Category | Value |
|---|---|
| 0-15 min | 15 |
| 15-30 min | 15 |
| 30-45 min | 15 |
| 45-60 min | 15 |
| 60-90 min | 30 |
- 0–15: Physical exit + micro-decompression
- 15–45: Somatic downshift + sensory hygiene
- 45–90: Mindfulness protocol + pre-sleep routine
Let me break down exactly what to do inside each.
Step 1: Immediate Post‑Shift Protocol (T0–15)
This is the part everyone wastes scrolling Epic messages and doom‑scrolling WhatsApp.
Your only goals here are: exit, separate, and signal “off‑duty” to your nervous system.
1.1 Hard Stop Ritual at Sign‑Out (2–3 minutes)
When your sign‑out is done:
- Close your laptop fully. Do not leave it half‑open like you might keep working.
- Say one explicit boundary phrase (out loud or in your head):
“My responsibility for this shift is complete. The team now holds the work.” - Take three slow breaths: inhale through nose 4 seconds, exhale through pursed lips 6 seconds. On each exhale, consciously drop your shoulders.
I have seen this tiny ritual cut the “phantom responsibility” rumination by half. It is primitive but it works: your body needs a signal that the role has changed.
1.2 Corridor Mindfulness Walk (5–7 minutes)
From ward to locker room / car / train: this is your first protocol.
Walk in silence. Phone on silent, in pocket.
Use a simple sensory anchor called 5–4–3–2–1 on the move:
- Name 5 things you see (mentally, no need to talk out loud)
- 4 things you feel physically (shoes on floor, badge on chest, air on skin)
- 3 things you hear
- 2 things you smell
- 1 thing you are grateful you do not have to handle anymore this shift
This is not “gratitude journaling.” This is attentional re‑anchoring—to get your brain out of predictive, future‑oriented clinical mode and into present‑sensory mode.
1.3 Gatekeeper Rule for Phone Use
Before you look at your phone, set one rule:
“I will check only logistics: transport, safety, essential messages from family. No social media, no news, no non-urgent messages until I am in my sleep‑transition block.”
You are cognitively impaired. You are emotionally raw. The algorithm will win. Do not pretend you will “just check one thing” and stop.
Step 2: Somatic Downshift and Sensory Hygiene (T15–45)
This is where most people wreck their post‑night recovery. Bright cafeteria lights, heavy greasy food, venting in loud groups, then “I can’t fall asleep.”
You are trying to get a circadian‑confused brain to stop thinking it is midday.
2.1 Light Management: Treat It Like a Drug
After consecutive nights, light is not a neutral factor. It is medication.
- If you are going home to sleep immediately
You want to minimize bright light exposure. Use:- Dark sunglasses from hospital to home
- Brimmed cap if you are walking in bright sun
- Avoid sitting in brightly lit cafeterias
- If your schedule demands staying up a bit (e.g., childcare drop‑off)
Then be deliberate: 15–20 minutes of bright, outdoor light to keep you functional, then dim your environment again once home.
You are basically doing field pharmacology with photons.
2.2 Micro‑Nutrition, Not a Meal
Large, heavy meals when your gut thinks it is “night” are a good way to get reflux and horrible sleep.
Target: 200–300 kcal, high protein, low simple sugar, low volume.
Examples that actually work in real hospitals:
- One Greek yogurt + a handful of nuts
- Half a sandwich (turkey/cheese) + small apple
- Protein shake you brought yourself + a banana
Avoid “reward pancakes” and fries after the last night. That is not self-compassion, that is self-sabotage.
2.3 8‑Minute Somatic Reset
You do not need yoga. You need to send your vagus nerve a clear “we are safe now” signal.
Use this 8‑minute sequence once you are home (or in your call room if you are napping there before driving):
Legs‑up‑wall or on a chair (3 minutes)
- Lie on your back, calves resting on chair seat or up the wall.
- One hand on chest, one on upper abdomen.
- Breathe: in 4 sec / out 6 sec. Eyes closed.
Progressive release for jaw, shoulders, hands (3 minutes)
- On an inhale, gently clench jaw, shrug shoulders, make fists. Hold 3 seconds.
- Exhale and release jaw, drop shoulders, open hands.
- Repeat 5–6 cycles.
Box breath taper (2 minutes)
- Inhale 4, hold 4, exhale 6, hold 2.
- If you feel more anxious rather than calmer, drop the breath holds and just do 4‑in / 6‑out.
This is not fancy. But if you do it consistently, your body starts to associate the sequence with off‑duty safety.
Step 3: The Sleep‑Transition Mindfulness Protocol (T45–120)
Here is where we get to the actual “mindfulness” piece. Notice I put this after the body work and light management. Doing mindfulness on a body that is still in fight‑or‑flight is like doing CBT in the middle of a code.
I use three linked components:
- Cognitive “shutdown” ritual (5–7 minutes)
- Compassion‑anchored debrief (8–10 minutes)
- Sleep‑proximal attentional practice (10–15 minutes)
You can compress or expand each, but keep the order.
3.1 Cognitive Shutdown: Externalize, Then Contain
The biggest sleep disrupter post‑nights is not coffee. It is looping thoughts: “Did I sign out that lab?” “What if that baby decompensates?” “I should have ordered…”
You are going to externalize then contain in under 7 minutes.
Step‑by‑step:
Two‑Column Brain Dump (3–4 minutes)
On paper, not in your phone. Two headings:- “Outstanding tasks / follow‑ups”
- “Ruminations / what‑ifs”
Under tasks, list anything you genuinely must follow up (e.g., “Email attending about culture result,” “Review EEG tomorrow”). Short, no details.
Under ruminations, everything else: “Should have pushed for earlier CT,” “Family looked angry,” “That consultant was dismissive.”Task Containment (2 minutes)
Draw a box around the “Tasks” column and write a specific time you will handle them:
“To be addressed: tomorrow 17:00–17:15.”
Then put the paper in a visible but closed place (drawer, folder). This is a cognitive contract. You are telling your brain: “We are not ignoring this; we are scheduling it.”Ruminations Reframe (1 minute)
At the bottom of the ruminations list, write:
“These are signs that I care and I am tired. I will review what actually needs learning when rested.”
You are not trying to argue with the thoughts. You are just parking them in a safer lot.
3.2 Compassion‑Anchored Debrief: Ethical Reset
This is the part that protects your long‑term professionalism.
After consecutive nights, your internal critic is loud and vicious. That critic, unchecked, becomes both burnout and ethical erosion. You normalize behaviors you used to find unacceptable.
We will use a brief, structured self‑compassion debrief tied explicitly to ethics.
Script (adapted for post‑night use):
Acknowledge shared humanity (2–3 minutes)
Sit or lie comfortably. Eyes closed if possible.Say mentally:
“Many clinicians feel this depleted after nights. Exhaustion is not a personal failure, it is a predictable state.”Then recall one colleague you respect who has admitted struggling on nights. Name them in your mind.
This interrupts the “everyone else handles this fine” narrative.Name the ethical pressure points (3–4 minutes)
Ask yourself, gently:- “Where did I come closest to not being the clinician I want to be?”
Maybe it was snapping at a nurse, rushing consent, avoiding a family, delaying a note.
For each, describe it in one neutral sentence in your mind:
“I spoke sharply to the nurse in the ED when my pager was going off.”Then add:
“That was an understandable response from an exhausted clinician, and I still want to do better.”This preserves both accountability and compassion.
- “Where did I come closest to not being the clinician I want to be?”
Re‑anchor to values (3 minutes)
Choose one professional value you care about: respect, thoroughness, honesty, presence, etc.Then a simple phrase linked to your next shift:
“On my next shift, I will prioritize [value] in one concrete way.”
Example: “I will take one extra minute when I feel irritated to ask the nurse what they are most concerned about.”
You are not doing a full moral inventory. You are preventing ethical drift. Small but critical difference.
3.3 Sleep‑Proximal Attentional Practice
This is the mindfulness piece that directly supports sleep onset after nights. Think of it as a bridge from “thinking” to “sleeping.”
You have two main options depending on your brain’s default mode: visual or somatic.
Option A: Body‑Based Anchor (good for restless thinkers)
Duration: 10–15 minutes, done lying in your sleep position.
Position
Get into your actual sleep position. Not sitting up for “meditation,” then changing. The body should learn: these cues = sleep.Narrowed body scan
Forget the 45‑minute MBSR scans. You are doing a 3‑zone scan:- Face/jaw
- Chest/shoulders
- Hands
Cycle 3–4 times:
Attention on the zone, notice tension, consciously soften on the exhale.Breath‑count practice
Inhale, exhale = count 1. Up to 10, then back to 1.
When (not if) your mind wanders, notice “thinking” and gently restart at 1.
Goal is not “10 flawless breaths.” Goal is to repeatedly practice the micro‑movement: notice → label → return. That is mindfulness.
If, after 10–15 minutes, you are more wired, stop. Pushing longer in that state can backfire. Quietly shift to a neutral sensory anchor like a fan sound or white noise.
Option B: Imagery Anchor (good for ruminative replay of cases)
If your mind keeps replaying the night (the code, the angry family, the difficult handoff), trying to focus on breath sometimes makes it worse. Use a competing visual task.
Duration: 10–15 minutes
Script:
- Choose a familiar, neutral place: your childhood kitchen, a specific hiking trail, a familiar beach.
- Mentally “walk through” in slow motion, engaging all senses:
- What do you see on your left? On your right?
- What are 3 distinct sounds?
- One smell?
- Each time the mind jumps to hospital content, say “work” quietly in your mind, then re‑locate yourself back in the scene.
This is not dissociation. You are giving your visual cortex a harmless job while the rest of your brain powers down.
Environmental Guardrails: The Non‑Negotiables
Even the cleanest mindfulness sequence fails if your environment is screaming “daytime.”
Here are the structural pieces I have seen matter most, across residents and attendings.
| Priority | Description |
|---|---|
| Light control | Blackout curtains / eye mask |
| Noise control | Earplugs / white noise |
| Phone boundaries | Phone out of reach, on DND |
| Temperature | Slightly cool room (17–20 °C) |
| Social boundaries | Household informed, “do not knock” |
Light and Noise
- Blackout curtains or a solid eye mask. If I had to pick one investment for a night‑shifter, it is curtains.
- White noise (fan, app, machine) to mask daytime household noise.
- Earplugs if you tolerate them.
Phone and Digital Hygiene
This one is straightforward: do not bring the arsonist into the fire‑prone forest.
- Phone on Do Not Disturb, physically away from the bed (across the room or in another room).
- Only emergency bypass allowed: partner / kids’ school / whoever is truly critical.
If you are thinking “But I relax by scrolling,” be honest: has that ever actually shortened your sleep latency after nights?
Social Contracts
If you live with others, formalize a post‑nights treaty:
- A sign on the door (simple: “Post‑night sleep — please text not knock”).
- Prohibited actions: vacuuming outside door, loud calls on speaker in next room, “quick questions” about chores in your first sleep cycle.
You are not being high‑maintenance. You are doing harm reduction.
Ethical Dimension: Fatigue, Accountability, and Self‑Deception
Let us address the ethics head‑on.
You will see two bad patterns around nights:
- The martyr narrative: “Real doctors just push through.”
- The entitlement narrative: “I suffer, so I am allowed to be an ass.”
Both are ethically lazy.
Your fatigue does not erase accountability. It does change the standard of what is reasonably preventable versus system‑induced.
Sleep‑transition mindfulness protocols sit at that junction:
- You cannot fix unsafe scheduling.
- You can absolutely reduce preventable cognitive sludge and emotional spillover.
What does this look like in practice?
- Fewer avoidant behaviors: not skipping family updates because “I am too fried.”
- Less misdirected anger: noticing irritation as a fatigue symptom rather than moral failure of the nearest nurse.
- More timely recognition of impairment: “I am not safe to drive yet; I will nap in the call room 20 minutes and do my somatic reset.”
If you routinely ignore your own post‑night state, you end up doing quiet damage: curt conversations, sloppy notes, bitterness toward patients. Over years, that becomes character, not just context.
So yes, there is a moral obligation to manage your transitions as best you can.
Putting It Together: A Concrete 60‑Minute Protocol
Let me give you a tight, realistic 60‑minute sequence you can trial after your next 3+ night block. Assume you get out at 8:00 AM and reach home around 8:20.

| Step | Description |
|---|---|
| Step 1 | Sign out complete |
| Step 2 | 3-breath boundary + corridor walk |
| Step 3 | Travel home with light control |
| Step 4 | Small snack + water |
| Step 5 | 8-minute somatic reset |
| Step 6 | Cognitive shutdown on paper |
| Step 7 | Compassion debrief |
| Step 8 | Body-based or imagery anchor in bed |
| Step 9 | Sleep |
Example timeline:
08:00–08:10
Sign‑out boundary ritual, corridor sensory walk, phone used only for transit.08:10–08:20
Travel home with sunglasses, minimal chatter.08:20–08:30
Small snack + hydration, bathroom, change into sleep clothes.08:30–08:38
8‑minute somatic reset (legs‑up, tension‑release, box‑taper breathing).08:38–08:45
Cognitive shutdown on paper (two columns, task containment, ruminations note).08:45–08:53
Compassion debrief (shared humanity → name pressure points → one value reset).08:53–09:08
In bed, body‑based or imagery anchor.
By 9:10 you are either asleep or at least not actively sabotaging your physiology with screens, bright light, and tense rumination.
You will not execute this perfectly. That is fine. Target: do 70 percent of it, 70 percent of the time. The benefit is cumulative.
Advanced Moves For Specific Problems
“My Heart Is Racing; I Am Too Wired to Sleep”
Classic high‑sympathetic state. Do not double down on breath‑focus—it can feed the anxiety.
Use:
- 5 minutes of paced walking in a dim room, matching breath to 4 steps in / 6 steps out. Then
- 10 minutes of imagery anchor lying down.
If your heart rate is genuinely high (100+ at rest) and you feel physically ill, this is medical, not just psychological. Get evaluated.
“I Keep Dreaming Nightmares About the Shift”
That is your consolidating memory system doing clean‑up. You cannot stop the dreams completely, but you can reduce intensity.
- Before sleep: pick one neutral image to “plant” (e.g., your hiking trail scene) and run it for 2–3 minutes.
- On waking from a nightmare: sit up, feet on floor, name 3 objects in room out loud, then 5 slow exhale‑heavy breaths. Then back to a short imagery anchor before sleeping again.
“My Family Thinks I Am Overreacting”
Then you have a communication problem, not just a sleep problem.
Spell it out once, clearly:
“After 3 nights, my brain is functioning like I am legally drunk. This 90‑minute block when I get home is the difference between me staying safe and me making errors. I need your help protecting it.”
If needed, put it in writing on the fridge. You are not being fragile. You are being responsible.
FAQ (Exactly 4 Questions)
1. Is it realistic to do all this as an intern with terrible schedules?
You will not hit every step after every set of nights, especially on brutal rotations. That does not invalidate the protocol. Start by protecting two things: the 8‑minute somatic reset and the 5–10‑minute in‑bed attentional practice. Those alone, done consistently, change your baseline. Layer in the cognitive shutdown and compassion debrief when you have slightly more time.
2. What if I only have a short window before I need to stay awake (e.g., switching back to days)?
If you are flipping quickly back to days, the goal shifts from “max sleep now” to “strategic nap plus circadian realignment.” Do a compressed version: corridor walk, 5‑minute somatic reset, 5‑minute imagery anchor, then a 60–90 minute nap in as dark a room as possible. After waking, get strong bright light exposure and some movement. You can still use the compassion debrief later that day before your main nighttime sleep.
3. Can I just use an app like Headspace or Calm instead of all this?
Guided apps are fine as supplements. They are not a protocol. Most are not designed around night‑shift physiology, circadian misalignment, and ethical load. Use an app track if it helps you stick to the body‑based or imagery anchor section, but keep the structural pieces: light control, somatic reset, cognitive shutdown, and value‑anchored debrief. The app should fit inside your protocol, not replace it.
4. How do I know if I need professional help beyond these practices?
Red flags: persistent inability to sleep even on non‑clinical days, significant anxiety or panic about going to work, intrusive memories that feel like re‑living events, or a consistent pattern of serious errors or near‑misses that you attribute to fatigue alone. If any of these apply, see occupational health, your primary care clinician, or a mental health professional experienced with shift workers. Mindfulness protocols are powerful, but they are not a substitute for treatment of major depression, PTSD, or medical sleep disorders.
Key takeaways:
Treat your post‑night window like a clinical procedure, not a vague intention. Combine light control, somatic reset, cognitive shutdown, and a brief, values‑anchored mindfulness practice. You are not just chasing more sleep; you are protecting your judgment, your relationships, and your ethics across a career that will keep asking you to function in physiologically stupid conditions.



















