The myth is that the smartest person in the room makes the best decision. In residency leadership, that is flat-out wrong. The people who can quiet their own minds on command make the best decisions. And program directors know it.
I’ve watched this up close in selection meetings, remediation hearings, and those awful “do we fire this resident?” conferences. The difference between the PD who sleeps at night and the one who burns out isn’t intelligence, or experience, or how many PubMed citations they have. It’s their ability to shut down the internal noise long enough to see clearly.
You’re not going to hear this at some shiny “leadership in medicine” workshop because most of what’s taught there is surface-level. What I’m going to walk you through is what actually happens behind closed doors when the stakes are high, careers are on the line, and everyone is tired, angry, or scared.
Top program directors have systems—mental and behavioral—to quiet their minds when it matters. They construct that calm. It is not an accident and it is not “just personality.”
Let’s pull back the curtain.
What Really Happens Right Before a High‑Stakes Call
There’s a pattern you only see once you’ve sat through enough of these meetings.
The agenda item looks harmless on paper: “Review Resident X status” or “Rank list finalization.” But everybody in that room knows something real is on the line. Someone’s career. Patient safety. The integrity of the program.
Here’s what you think happens:
Everyone calmly reviews the data. Rational discussion. Evidence-based decisions. Professionalism all around.
Here’s what actually happens in most programs that are run by stressed, reactive leadership:
- People walk in already pissed off from their day.
- The first loud, confident voice in the room frames the issue.
- Confirmation bias kicks in. Hard.
- One or two people get emotionally hooked—defensive, angry, self-righteous.
- Everyone else just wants the meeting to end.
In those programs, the decision is made by emotional inertia, not wisdom.
Now contrast that with the programs that consistently produce good residents, handle problems ethically, and rarely get sued or reported. Those program directors behave differently in the 10–20 minutes before the decision point. That’s the window they protect.
I’ve watched several of them closely—internal medicine, surgery, anesthesia, EM, from community to big-name academic. The best all do some version of three things:
- They deliberately slow themselves down before the meeting.
- They structure the discussion so their own reactivity doesn’t drive it.
- They use simple, repeatable internal rituals to reset when emotions spike.
This is mindfulness in medicine, but not the soft, Instagram version. This is a tactical skill, used like a scalpel.
How They Actually Quiet Their Minds (Not the Fluffy Version)
Let’s get specific. These people are not sitting on yoga mats with candles in the resident workroom. They’re walking from a chaotic clinic to a conference room, with three pages of complaints in their hand, and a chief resident texting them about a code blue down the hall.
So what do they actually do in those few minutes?
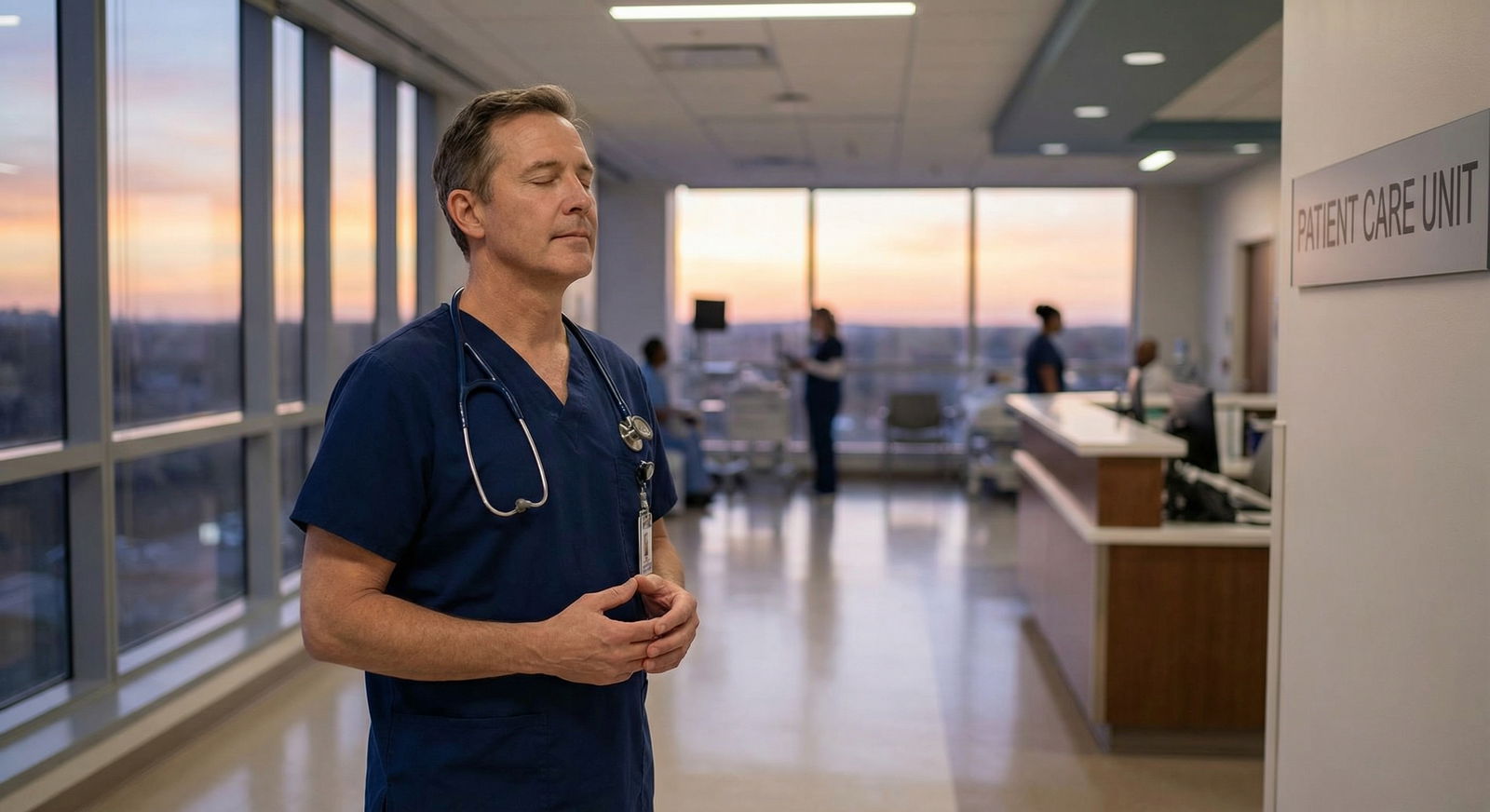
1. The 90‑Second Decompression Window
The best PD I know in surgery has a ritual I’ve seen him follow even when running 45 minutes behind: he insists on 90 seconds alone before a high-stakes meeting. Not five minutes. Not a half day retreat. Ninety seconds.
He closes the conference room door, leaves his phone facedown and off to the side, sits down, and does the same sequence every time:
- Feet flat on the floor
- Hands resting on thighs
- Eyes closed
- Three slow breaths, each one with a visible longer exhale
That’s it. But he’s consistent. Residents think he’s “just composed by nature.” He isn’t. I’ve seen him come in red-faced from the OR, sit, breathe, and after a minute and a half his voice drops half an octave and his jaw unclenches.
What’s happening under the hood? He’s hitting the brakes on his sympathetic nervous system. That longer exhale is not a wellness gimmick; it’s physiology. You know this from Step: parasympathetic activation, vagal tone, all the buzzwords. The difference is that he actually uses it.
And here’s the part people miss:
He treats that 90-second window as non-negotiable. If someone knocks, he waits. If his phone buzzes, he ignores it. The ritual comes first, then the decision.
Most trainees never learn this because they think, “I don’t have time.” Truth: you do. You’re just not willing to reserve it.
2. The “Name the Hook” Move
The strongest program directors are brutally honest with themselves about what’s hooking their mind.
One PD in IM I worked with would literally write at the top of her notes, before discussion:
- “I’m angry about last week’s no-show”
- “I like this resident personally”
- “I’m afraid of the complaints committee”
She didn’t do this to be poetic. She did it because unacknowledged emotion runs the show.
This is mindfulness stripped of all the spiritual packaging. It’s cognitive labeling: I’m angry, I’m anxious, I feel protective. When you name it, it loosens its grip.
I’ve watched her in ranking meetings say, out loud, “I’m aware I really like this applicant and I’m worried that’s coloring my judgment. So let’s hear from others before I talk.” That’s psychological judo. She neutralizes her own bias in front of the room, and it changes the tone immediately.
The weak PDs? They pretend to be “objective” while everyone can see they’re clearly taking it personally. That’s how you get retaliatory remediation plans and insane expectations that would never fly if they were calm.
3. The 4‑Question Ethical Filter
There’s a quiet trick that faculty almost never explain to residents: the mental checklist the good ones run before they lock in a high-stakes decision.
A strong program director I know in EM has something he calls his “Ethics in 60 Seconds” scan. He doesn’t advertise it, but you can see him pause, stare at the table for a moment, and you know he’s running it.
It’s four questions, always in this order:
- If this were my own kid as the resident, would I accept this decision?
- If this were my own family member as the patient, would I accept this decision?
- If this becomes public—email, legal record, or Twitter—can I defend not just the outcome, but the process?
- Am I making this to end my discomfort, or to do the right thing?
That fourth one stings. Because a lot of “decisive leadership” is just people trying to make their own anxiety stop.
This is where quieting the mind intersects directly with medical ethics. You can’t answer those four questions cleanly if you’re spun up, angry, humiliated, or rushing. Your brain will rationalize whatever helps you feel less bad in the moment.
The best PDs force a micro-pause and run that ethical filter. They don’t call it mindfulness, but that’s exactly what it is.
The Hidden Structures That Support a Quiet Mind
Let me tell you a secret most faculty will not spell out:
Top program directors design their environment so they don’t have to rely on willpower to stay calm.
They aren’t superhuman. They’re smart enough to know they’re not.
How They Set Up the Room (Literally)
The physical setup of the room is not an accident.
I’ve seen high-functioning programs do things like:
- Put data up first, opinions later. They start with the evaluation grid, milestones, written feedback, timelines. Nobody launches into “I just feel like…” until after everyone has seen the same raw material.
- Assign a facilitator (often an APD or chief) whose explicit job is to slow the discussion and call timeouts when it gets heated.
- Remove phones from the table. Not because of distraction only, but because the constant buzzing keeps everyone’s nervous system on high alert.
The PD who cares about their own mental stillness will walk in early, check the projector, lay out printouts, and literally arrange the seat order so adversarial people are not sitting directly opposite each other. This isn’t pettiness; it’s aggression prevention.
They are building a container that lets them stay calm. The ones who don’t? Their meetings are chaos, and their decisions look like it.
Pre‑Commitment to Process
Another quiet trick: the best leaders pre‑commit to a decision process before they know which way they personally want it to go.
For example, in a remediation case:
- They’ll agree up front: “We need at least two separate, documented patient safety events in this category before we escalate to probation.”
- Or: “We won’t move to dismissal without an outside review from another department.”
- Or: “Ranking will prioritize clinical performance over interview ‘vibes’ when those conflict.”
That pre-commitment means that when their emotions flare—maybe they’re angry about an email the resident sent, or smitten with a charismatic applicant—they have a prebuilt guardrail. They don’t have to “be mindful” in the moment as much, because the structure is doing some of the work.
Your future self will thank you if you learn this early.
Personal Rituals Top PDs Use That Nobody Talks About
You’ll never see these in a faculty development PowerPoint, but they’re everywhere behind the scenes if you pay attention.

| Category | Value |
|---|---|
| Brief breathing | 80 |
| Written reflection | 45 |
| Silent walk | 50 |
| Peer consult | 60 |
| Formal meditation | 20 |
These numbers are a rough approximation from what I’ve seen anecdotally: informal, quick rituals dominate. Long, formal meditation? Rare but powerful.
The “Walk the Hall Once” Rule
One PD in pediatrics I respect has a rule: if a decision could end someone’s training or fundamentally change their life, she must walk at least one hospital corridor alone before voting.
She doesn’t scroll, doesn’t check labs, doesn’t talk. She just walks the same loop: out of the conference room, down past the PICU, through the lobby, back up the stairs. Three to five minutes tops.
Why? She says, “I need my body to catch up with my brain.” That walk lets her feel the floor under her feet, notice that her heart rate is up, her shoulders are tight. She’ll often realize, mid-walk, that what’s really bothering her is something entirely different—an argument with the DIO, a bad morbidity and mortality last week, whatever.
By the time she re-enters the room, that emotional static has turned down from a nine to a four. Then she can think.
You can replicate this as a resident before hard family meetings, code status conversations, or when you’re about to write a scorched-earth email. One corridor. No phone. Notice your body.
The “Two Sentences on Paper” Trick
Another almost invisible habit: brief written reflection right before or after a serious decision.
A strong PD in anesthesia I know keeps a tiny notebook in his pocket. Before a tough meeting, he’ll write two quick lines:
- “What’s my job in this meeting?”
- “What would ‘I did my duty’ look like here?”
Then he answers in a couple words. “Job: protect patients / be fair to trainee / uphold program.” “Duty: clear expectations, honest feedback, no surprises.”
Does that magically erase all bias? Of course not. But it anchors his mind. It pulls him away from “how do I not get yelled at by the dean” and back to core professional identity.
You don’t need his notebook. A notes app entry or a scrap of paper does the job. The point is the externalization. Once you write down your intention, your brain’s less likely to get hijacked.
Strategic Silence in the Room
The strongest PDs use silence like a tool.
Here’s what I mean. In a heated discussion about putting a resident on probation, less experienced leaders will talk more when anxious. They fill the air, try to convince, justify, defend. The room’s energy escalates.
Seasoned PDs do something opposite. At the exact moment when the discussion is white-hot, they… stop. They look down at their notes. Or at the clock. Or simply let five seconds pass without saying a word.
Those five seconds are not accidental. They’re a reset. In that pause, a couple things happen:
- Other people catch their breath and sometimes self-correct.
- The emotional wave crests and breaks instead of building.
- The PD has space to feel their own body—tension, heat, heartbeat—and not be ruled by it.
Silence is how they quiet both the room and themselves. You can practice that too. When you feel the urge to jump in and “fix it” immediately, count one slow breath before speaking. It will feel like forever. It’s actually about two seconds. That’s often enough.
Where Mindfulness and Medical Ethics Actually Meet
Let’s stop pretending these are separate topics. Every ethics case you’ve discussed in a classroom—justice, nonmaleficence, autonomy—gets distorted when the decision-maker’s mind is flooded.
A noisy mind does at least three predictable unethical things:
- Protects self over truth. Anxiety pushes leaders toward the path that reduces their own risk, even when it’s unfair to the resident or patient.
- Punishes instead of teaches. Anger turns remediation into retribution. You see “we’ll teach them a lesson” plans that have no educational value.
- Rationalizes shortcuts. Tired, rushed people skip due process, documentation, second opinions—then backfill justification later.
I’ve seen PDs reverse course on a dismissal decision after a single night’s sleep and a calmer conversation. Same facts. Different mind.
The ones who are consistently ethical don’t rely on “being a good person.” They build habits that keep their nervous system from hijacking their principles.
There’s a reason burnout and ethical erosion travel together. A burned-out leader’s baseline is already revved up. Without deliberate quieting practices, every tough call gets made from a place of threat perception. That’s how programs drift into toxic culture “without meaning to.”
If you care even vaguely about being an ethical physician leader down the line, you can’t ignore this. Mindfulness isn’t bonus wellness. It’s an ethical tool.
What You Can Steal Now as a Student or Resident
You’re not a program director yet, but you’re already making high‑stakes decisions—just on a different scale.
- Do I call this attending at 2am?
- Do I speak up about this near miss?
- Do I fail this student who’s unsafe but likeable?
- Do I push back on a family demanding non-beneficial care?
You don’t need a title to use the same mental mechanics.
Here’s the stripped-down version you can start using tomorrow:
- Take 3 slow breaths before any hard conversation or order. Exhale longer than you inhale. Out breath is the off switch.
- Name one emotion silently. “I’m scared.” “I’m annoyed.” “I’m exhausted.” That’s mindfulness 101, without the incense.
- Ask one ethics question. The fastest one is: “If this were my family, would I be okay with this plan?” If the answer is no, pause.
- Build a 60‑second ritual. A tiny walk, a sip of water at the window, a note on paper. Something you repeat so your body starts to associate it with “calm, then decide.”

| Step | Description |
|---|---|
| Step 1 | Trigger - High stakes decision |
| Step 2 | Step away for 60 seconds |
| Step 3 | 3 slow breaths |
| Step 4 | Name emotion silently |
| Step 5 | Ask ethics question |
| Step 6 | Seek second opinion |
| Step 7 | Make decision and document |
| Step 8 | Still unclear |
This is exactly what top PDs are doing, just scaled and refined over years. You do not need to wait a decade to start.
The Part Nobody Admits: Sometimes They Fail
Let me be honest. Even the best program directors blow it.
They lose their temper in meetings. They push through a decision they regret. They let a toxic senior resident skate because they’re too tired to fight. They hold a grudge. They’re human.
But here’s the difference: the good ones notice when their mind wasn’t quiet, and they change something.
I’ve seen PDs call follow-up meetings just to say, “I was too heated last time; we need to revisit this.” I’ve watched them apologize to residents for the way a decision was communicated, even if the decision itself stood.
That’s what a serious mindfulness practice in medicine actually looks like. Not perfect composure. Just a relentless commitment to come back to clarity, again and again.
You won’t hear this language at grand rounds, because it sounds vulnerable, and many academic cultures punish that. But this is what sustains the people who make hard calls for a living.
And if you plan on being one of them someday, you’d better start training that muscle now.
FAQ
1. Do program directors really have time for this, or is this just theory?
They make time. Or they burn out and make bad decisions, and eventually someone else replaces them. The quieting practices I’ve described are measured in seconds to a few minutes—90‑second breathing, a short hallway walk, a quick ethics scan. The PDs who claim they’re “too busy” are usually the ones whose meetings spiral and require more time later to clean up the fallout. The ones who last 10–20 years in those roles all, without exception in my experience, have some kind of deliberate pre‑decision ritual, even if they’d never call it “mindfulness.”
2. How do I practice this without looking weird or “soft” in a surgical or high-intensity culture?
You don’t need to announce anything. You pause at the computer before entering the order, take three slow breaths while staring at the screen. You step into the stairwell for 30 seconds between seeing the lab result and calling the family. You jot a two-word note on your list before a difficult page. From the outside, it looks like you’re just thinking—which is exactly what you’re supposed to be doing. The loudest “no mindfulness” people are often the ones pacing in circles, ranting, and making impulsive calls. You don’t need to convert them. You just need to not become them.
3. What if I quiet my mind and still don’t know what the right decision is?
Welcome to actual leadership. A quiet mind doesn’t guarantee certainty. It gives you the best possible starting point to weigh options instead of reacting blindly. When you’ve done your micro‑ritual and still feel torn, that’s your cue to pull in help: senior residents, another attending, ethics consult, risk management. The signal you’re looking for isn’t “I feel 100% sure.” It’s “I can explain my reasoning, my process was fair, and I wasn’t just trying to make my own discomfort stop.” With that foundation in place, you’re ready for the next layer of growth—learning how to own your decisions publicly and stand in them when they’re challenged. But that’s a story for another day.



















