
You just opened your NRMP email. You matched. Relief hits first. Then you see the line you half-ignored all season:
“Accreditation Status: Initial Accreditation.”
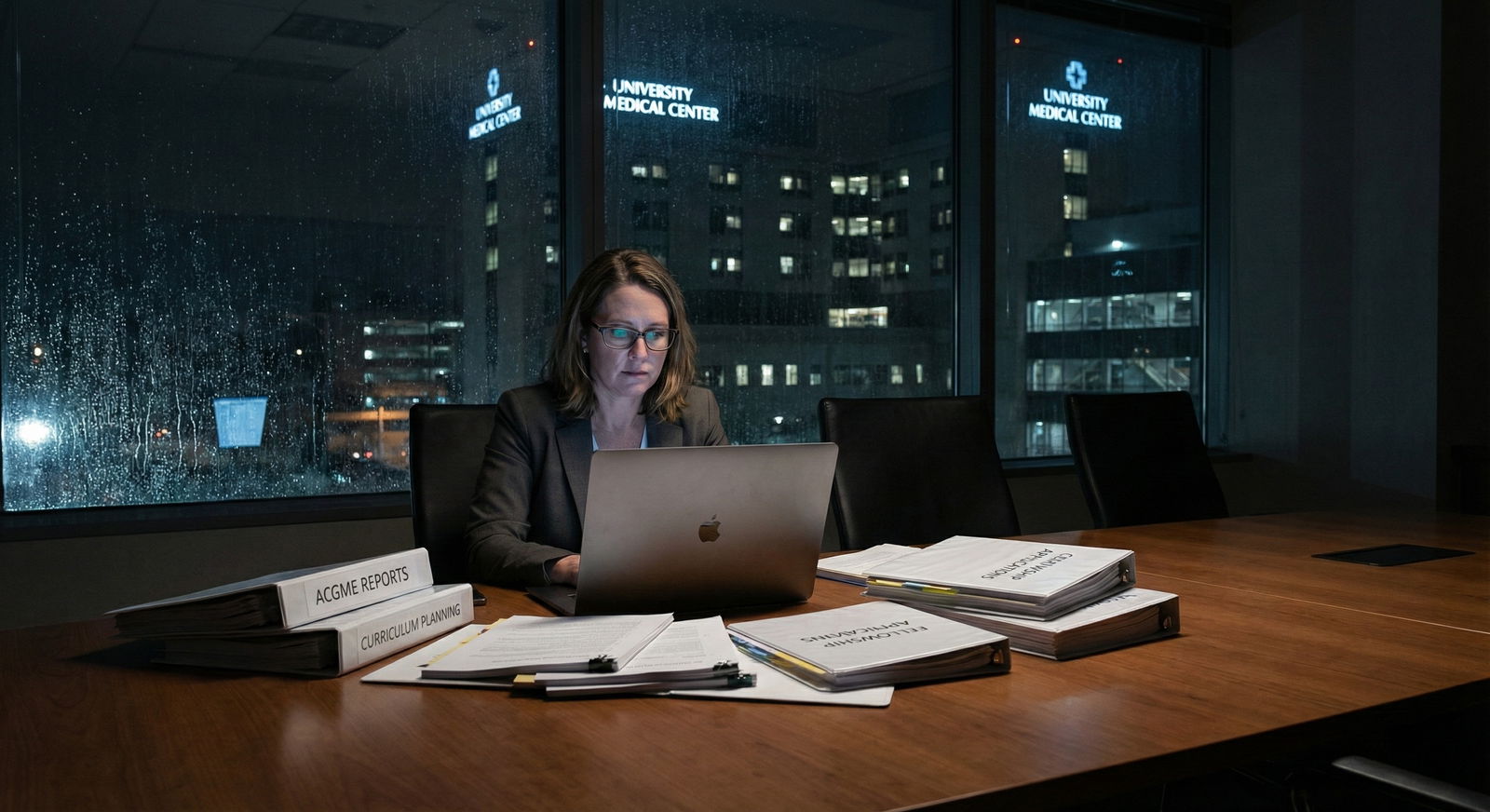
Now the relief is mixed with a knot in your stomach. You google the program. No alumni. Barely any website. PD’s LinkedIn shows they were fellowship faculty two years ago. Your classmates are posting about big-name institutions, and you’re trying to figure out:
Did I just sign up to be the guinea pig?
You did. And that’s not automatically bad. But it is different. You can’t treat this like matching into a 40‑year-old program that runs itself on autopilot. You need a plan.
Here’s your situation-specific checklist: what to do in the weeks and months after you match to a program still in Initial Accreditation.
1. Get Clear on What “Initial Accreditation” Actually Means
Before you decide whether to freak out, you need to understand the box you’re in.

| Category | Value |
|---|---|
| Initial | 3 |
| Initial Continued | 2 |
| Continued | 10 |
| Probation | 1 |
| Withdrawal | 0 |
That chart is generic, but it captures the vibe: Initial Accreditation is an early-phase status, not a red flag by itself.
Here’s the blunt version:
- Initial Accreditation = The ACGME has reviewed the application and decided the program meets standards on paper and in early implementation. It’s allowed to recruit and train residents.
- It is not probation. Probation is a warning for established programs that screwed up.
- Initial programs get more frequent ACGME oversight early on. That can actually protect you if you know how to use the system.
The key risk is timing: you’re betting the program will progress to Continued Accreditation (or at least stay accredited) through your training. Most do. Some stumble.
So your first move is not to panic. It’s to gather data.
Action for this week: download and skim the ACGME FAQ for your specialty about new programs. It will answer most of the structural questions and calm about 30% of your anxiety.
2. Do a Post-Match Deep Dive on the Program
You’re not auditioning anymore—but you are deciding how defensive or aggressive you need to be in protecting your training.
You need to know three things:
- Who is actually running this?
- What is the institutional track record with other programs?
- What does the early-scuttlebutt look like?
A. Map the leadership and their leverage
Go beyond the glossy ERAS blurb.
Look up:
- Program Director (PD)
- Associate PDs
- Department Chair
- DIO (Designated Institutional Official) — often buried on the GME office page
Then figure out:
- Has this institution successfully built other residencies/fellowships in the past 5–10 years? Example: if they started FM, IM, and EM and all now have Continued Accreditation, that’s reassuring.
- Is your PD relatively senior (e.g., previously core faculty at a respected program) or brand new attending two years out?
You’re looking for signs that the PD can:
- Pull in resources
- Push back on hospital admin nonsense
- Recruit credible faculty
If everyone looks green and there’s no strong department chair, put a mental “higher risk” flag on the situation—not to scare yourself, just to be realistic about how much you’ll need to self-advocate.
B. Check the institution’s GME ecosystem
This is where people skip steps and get burned.
If the hospital already has:
- Multiple other residencies with solid reputations
- A functioning GME office with a real staff (not one part-time coordinator buried in HR)
- Active GMEC (GME Committee) minutes and policies online
…you’re in a better situation than a standalone, first-ever program where they’re learning GME from scratch.
At the same time, some big brand names run chaotic new programs. I’ve seen a major academic center completely under-resource a new specialty because it wasn’t a financial priority.
So: track record matters, but it’s not everything. Still, you want to know whether you’re joining:
- A teaching culture building their nth program
- Or a hospital figuring out what a “resident” is
Action for this week: make a simple one-page “program dossier” for yourself: PD background, chair background, GME office size, other residencies present, hospital type (community, tertiary, academic partner).
3. Clarify the Accreditation Timeline Relative to Your Training
You need to know where your class sits on their ACGME timeline. That determines how nervous you should be.
Ask directly (email PD or coordinator):
- What year did the program receive Initial Accreditation?
- When is the next ACGME site visit or review planned?
- Have you already had any ACGME reviews since starting residents? Any major citations?
Your mental model should look something like this:

| Period | Event |
|---|---|
| Launch - Year 0 | Initial Accreditation granted |
| Launch - Year 1 | First resident class starts |
| Early Oversight - Year 2 | Focused or full ACGME visit |
| Early Oversight - Year 3 | Decision on Initial Continued or Continued |
| Stabilization - Year 4-5 | Continued Accreditation expected if standards met |
Now overlay your own training length:
- 3-year program (IM, Peds, FM): you might be there for the full shift from Initial → Continued.
- 4+ year programs (Surgery, EM with prelim year elsewhere, etc.): you’re likely to see the transition one way or another.
Important but rarely said: even if a program’s status changes mid-training, existing residents are typically protected. ACGME doesn’t love stranding trainees. They either:
- Allow you to finish,
- Or place you elsewhere if training must cease.
Is that comfortable? No. But there’s a backstop.
Action for this week: send a short, professional email to the coordinator: “Could you share where the program is currently on the ACGME review timeline and when the next review is expected?” Save the response.
4. Assess Rotations, Volume, and Faculty Now — Not In October
What makes or breaks you isn’t the label “Initial Accreditation.” It’s whether you get:
- Enough reps
- Enough supervision
- Enough feedback
You need to quietly audit three things:
A. Rotation plan vs actual practice
Programs often sell a gorgeous rotation schedule on paper. The question is: are they actually delivering it?
Ask for:
- A sample PGY-1 schedule from the current class
- A full list of clinical sites and whether agreements are already executed, not “planned”
Then look for red flags:
- Heavy reliance on “planned” away rotations that aren’t finalized
- Overstuffed inpatient months with unclear clinic exposure (for primary care-based fields)
- ICU or key subspecialty rotations that hinge on outside hospitals that have never hosted residents before
If a big chunk of your education depends on “should be ready by July,” be cautious. That’s where residents end up as service workers instead of learners.
B. Patient volume and case mix
You’ll hear PDs say, “We’re very busy here.” That means nothing by itself.
Ask senior residents (if they exist) or early faculty:
- “On a typical ward month, what’s your cap, and do you usually hit it?”
- “How many procedures do interns typically get on a busy ICU month?”
- “For EM/surgery/OB-type fields: how many [deliveries, resuscitations, operative cases] does a PGY-2 roughly log in a year?”
You’re not trying to interrogate. You just want to know whether the hospital’s clinical reality can support what the ACGME requires.
| Area | Concrete Question |
|---|---|
| Wards | Do you usually run at or near cap on busy services? |
| ICU | How many procedures did you log as a PGY-1? |
| Clinic | How many half-days per week do you really get? |
| OR/ED | Are you primary operator or observer most days? |
| Teaching | Do attendings actually staff and teach on rounds? |
C. Faculty depth and stability
You want:
- Enough core faculty to cover key areas
- Faculty who actually want to teach, not just tolerate residents for RVUs
If the program has:
- 2–3 core faculty for a whole specialty,
- Heavy dependence on locums,
- Or a revolving door of young faculty burning out—
—expect instability, clinic cancellations, and constant schedule panic.
Action for this month: on your second or third contact with the program, ask if you can connect with 1–2 current residents (or incoming upper levels) for a 20-minute call. Prepare targeted questions, not vague “what’s it like” chatter.
5. Understand Your Rights and Recourse If Things Go Sideways
You need to know, in advance, what your options are if the program:
- Fails to progress to Continued Accreditation,
- Or turns out to be drastically different from what was promised.
This isn’t about being dramatic. It’s about not Googling in tears at 2 a.m. after a disaster.
Mechanisms you should know:
ACGME Resident Survey
You’ll fill this out annually. It matters. A lot. When entire classes tank supervision/education responses, ACGME shows up.Internal GME reporting paths
Every institution with ACGME programs must have:- A GME office
- A GMEC
- A process for residents to raise concerns (often anonymous or semi-anonymous)
ACGME Resident Portal for concerns
Residents can report concerns directly to ACGME. These are taken seriously, especially in early-phase programs.Transfer possibilities
Transfers are rare but real. They tend to happen when:- Accreditation is at risk,
- Or educational promises are not being met in major ways.
Don’t threaten transfer in week 2 because you don’t like the call schedule. But if major structural promises evaporate (core rotations disappear, key sites never materialize), you quietly start documenting and exploring.
Action for this month: find and bookmark your institution’s GME policies page. Specifically locate: duty hour policy, supervision policy, resident grievance process.
6. Plan How You’ll Protect Your Education from Day 1
New programs are busy. Leadership is juggling:
- Building schedules
- Negotiating with clinical sites
- Putting out fires you’ll never hear about
In established programs, the structure protects you. In a new one, you have to help protect your own training.
Here’s how.
A. From day one, keep a simple log
Not a novel. Just a running document with:
- Rotations & actual hours
- Key procedures/skills
- Significant deviations from what you were told (e.g., “Cardiology month turned into cross-cover because they had no faculty.”)
This is not for drama. It’s so that if you need to have a serious conversation in PGY-2 about gaps in your training, you’re bringing data, not vibes.
B. Be uncomfortably specific during check-ins
You will get periodic meetings with PD or faculty. Do not waste them on generic “it’s going fine.” Instead:
- “On my last ICU month, I got to intubate once, and I’d expected more. What is the plan to get me procedure numbers up to ACGME minimums?”
- “We were told we’d have half-day continuity clinic weekly; it’s been every other week due to staffing. Is that temporary, or will schedules be adjusted?”
When you’re specific, good PDs respond. Mediocre ones hand-wave. That distinction matters.
C. Build your own supplement plan early
New programs often underdeliver in:
- Research infrastructure
- Subspecialty exposure
- Exam prep culture
So you preempt it:
- Line up an online QI or research project with a mentor outside your hospital if needed.
- Join national specialty organizations early (they often have resident sections with free resources, webinars, mentors).
- Get a serious board review resource from PGY-1, not PGY-3.

| Category | Value |
|---|---|
| Research | 30 |
| Subspecialty exposure | 25 |
| Didactics | 25 |
| Clinical volume | 20 |
Action for the first 3 months of intern year: identify one area your program is clearly strong in, and one where it’s weak. For the weak area, design one concrete supplement: a textbook plan, a mentor, a niche clinic, a virtual course.
7. Handle Reputation, Fellowship, and Future Job Concerns Rationally
The fear in your head is probably something like: “Will anyone take me seriously if my residency is from a brand-new program?”
Let me be blunt:
Outside of ultra-competitive fellowships and snobby private groups, no one cares about the age of your program as much as they care about you and your letters.
But. You need a strategy if you care about competitive next steps.
If you’re aiming for fellowship
You can absolutely match into fellowship from a new program—if you do the following:
- Nail your in-training exams (ITE).
- Get at least one letter from someone with a recognizable name in your specialty (sometimes outside your home institution).
- Show that you sought out extra exposure if your program is light in your intended subspecialty.
That might mean:
- Away electives at established centers in PGY-2/3.
- Attending national conferences early. Presenting posters, even small ones.
Programs reviewing your application will ask themselves:
- Did this resident rise above the baseline of their environment?
- Are there trusted people vouching for them?
If the answer is yes, your “Initial Accreditation” program is a footnote, not a roadblock.
If you’re going straight to practice
Employers mostly care about:
- Board eligibility/certification
- References
- Procedural competence / autonomy
If your program delivers solid clinical training and you’re not a problem child, you’ll be fine. The hiring committee at a community group is not searching ACGME history to see if your program was initially accredited in 2023.
Action for this year: decide (even roughly) whether you’re fellowship-bound or not. If yes, identify one external mentor or contact in that field by the end of PGY-1.
8. Watch for True Red Flags vs Normal Growing Pains
Not every annoyance is a sign the program is failing. New programs are messy. Expect:
- Schedule hiccups
- Overloaded first few months as they balance coverage
- Some faculty who are still learning how to teach effectively
Those are growing pains.
True red flags look more like:
- Chronic duty hour violations with no attempt to fix them
- Persistent lack of supervision on high-acuity patients
- Promised core rotations that simply never materialize
- Intimidation or retaliation when residents raise concerns
- Repeated late or incorrect pay/benefit issues tied to “they still do not know what to do with residents”
If you see a pattern of those, that’s when you:
- Document,
- Use internal GME channels,
- And, if needed, reach out to ACGME.

9. Build Your Support Network Outside the Program
The most overlooked protective factor for residents in new programs: community outside their institution.
You need:
- At least one mentor not employed by your hospital.
- A peer group where you can sanity-check whether what you’re experiencing is normal.
Options:
- Medical school alumni in your specialty at other programs.
- National resident member groups (ACP, AAFP, ACEP, etc.).
- Online communities (with caution) where residents discuss program issues—use them for pattern recognition, not drama.
When you’re in a brand-new program, it’s easy to start thinking “maybe this is just how residency is.” Sometimes yes. Sometimes absolutely not. External voices help you sort that out.
Action for the next 2 months: schedule one 30-minute Zoom or phone call with a resident you trust at a more established program in your specialty. Ask them how their rotations, supervision, and didactics look in detail. Use that as a comparison point.
10. Mindset: You’re Not Just a Trainee, You’re a Co-Builder
Here’s the piece nobody tells you in the glossy recruitment talks:
You are not only training there. You are building that program.
That means:
- Your feedback shapes policies.
- Your habits shape culture.
- Your successes or failures become the story PDs tell to the next applicant class.
If that sounds exhausting, I get it. But it’s also leverage. In a 40-year-old powerhouse, you’re resident #612. In a brand-new program, you’re part of the foundation.
So, decide:
- What do you want the program to look like for the interns who come after you?
- Where are you willing to push? Where will you compromise?
I’ve seen first and second classes transform programs:
- They pushed for protected didactic time—and got faculty buy-in.
- They fought for fair call distribution instead of “interns do everything.”
- They modeled sane, respectful behavior in a culture that could’ve gone malignant.
You can also burn out and disengage. That’s always an option. But if you’re stuck there for 3–7 years, shaping it to be less miserable is usually worth the effort.

| Category | Value |
|---|---|
| Schedule design | 80 |
| Curriculum changes | 70 |
| Culture/norms | 90 |
(Those numbers are conceptual, but you get the point: your voice is louder in a new place.)
Your Concrete Next Step Today
Do this now, not “later”:
Open a blank document and title it:
“[Your Specialty] Residency – Initial Accreditation Game Plan.”
Then add three headings:
- What I Know (facts about the program’s status, leadership, timeline)
- What I Need to Find Out (rotation details, volume, supervision, GME processes)
- How I’ll Protect My Training (log system, mentor plan, external resources)
Under each heading, write 3–5 bullet points.
That document becomes your anchor. You’ll update it as you get answers. You’ll bring it into PD meetings. You’ll use it to catch problems early instead of in PGY-3 when they’re baked in.
You matched. That part’s done. Now your job is to make sure this new, initially accredited program actually turns into the training you deserve—because no one is going to care about your education as much as you do.















