Myth vs Reality: Do New Programs Really Give You More Early Autonomy?
The belief that “new residency programs give you more autonomy” is mostly fantasy—and sometimes a dangerous one.
I’ve watched this myth spread like gospel in applicant group chats and Reddit threads. The story goes like this: old, big-name programs are “hand-holding” and rigid, while shiny new community or university-affiliated programs supposedly throw you into the fire on day one, making you “more prepared” and “more independent” by graduation.
It sounds appealing. It’s also deeply misleading.
You do not want unstructured autonomy. You want scaffolded autonomy with backup you trust. Those are not the same thing, and newness has almost nothing to do with which one you get.
Let’s pull this apart.
Where This Myth Comes From (And Why It’s So Sticky)
The core misconception comes from conflating three things:
- Resident-to-attending ratio
- Patient volume vs. faculty bandwidth
- Actual supervisory culture
New or smaller programs often advertise: “You’ll have more responsibility.” Applicants translate that as “more autonomy.” Residents on the ground often translate it as “more work and less backup.”
You’ll hear lines like:
- “At Big Academic U, the fellow does everything. At New Regional, the resident is the primary decision-maker.”
- “Smaller programs let you run the ICU early.”
- “You’ll be first assist on every case because there are no fellows.”
Sometimes there’s a grain of truth. Often it’s marketing spin.
Here’s the uncomfortable reality: a lot of what gets sold as “autonomy” in new programs is actually underdeveloped infrastructure plus undersupervision, not intentional, educationally sound independence.
What the Data Actually Shows (And What It Doesn’t)
There is no big RCT of new vs legacy residency programs and “autonomy scores.” But we do have several relevant data sources:
- ACGME surveys (resident-reported supervision, burnout, program quality)
- Case logs (for surgical and procedure-heavy specialties)
- Board pass rates and citations/accreditation histories
- Published work on supervision, error rates, and “entrustment” models
Put simply: autonomy is not strongly determined by program age. It is determined by culture, staffing, and case mix.

| Category | Value |
|---|---|
| Program Age | 20 |
| Supervision Culture | 85 |
| Service vs Education Balance | 80 |
| Case Volume/Mix | 75 |
| Presence of Fellows | 60 |
Is this exact percentage breakdown from a meta-analysis? No. But it reflects what the literature and real-world experience actually support: program age is a minor factor compared to how a program structures supervision and workloads.
The ACGME doesn’t care if a program is 2 years old or 50. It cares whether:
- Faculty are available and supervising at appropriate levels
- Residents report appropriate support, not chronic unsafe independence
- Educational goals are being met (not just service needs)
New programs can do this well. Old programs can fail at it. And vice versa.
The “More Autonomy” Pitch: What It Often Really Means
Here’s the dirty little secret: when a brand-new or rapidly expanding program tells applicants “you’ll have more autonomy,” they’re often papering over resource gaps.
I’ve heard versions of these scenarios repeatedly:
- PGY-1 on nights cross-covering 80+ patients with a teleradiology service and an attending “available by phone” who is also covering multiple units.
- New ICU service where the resident is “running the unit” because the intensivist is spread across several hospitals and not physically present most of the day.
- Orthopedic or general surgery programs where “you’re first assist on everything” because there’s one attending, no fellow, no PA, and a brutal add-on case queue.
Is that autonomy? Technically, yes. Is it good autonomy? Absolutely not.
Good autonomy means: you make decisions, but in a structure where someone experienced has intentionally entrusted that level of decision-making to you, based on your demonstrated competence, and they’re close enough—physically or functionally—to catch you before you harm someone.
Bad autonomy is: you’re alone because there’s no one else.
Those are not pedagogically equivalent.
How Autonomy Should Work (And How You Can Tell If It Does)
Modern medical education uses something called Entrustable Professional Activities (EPAs) and staged supervision. The idea is simple: you earn autonomy task by task, not by calendar date or program marketing brochure.
Real autonomy tends to look like this:
- PGY‑1: You manage bread-and-butter admissions, present plans, and get real-time feedback. You feel the responsibility but know your attending is engaged.
- PGY‑2: You start running portions of rounds, triaging admissions, doing more complex procedures. Attending lets you struggle a bit—but is there.
- PGY‑3+: You run codes, lead teams, call consults independently, and staff decisions. Attending still owns the license and the outcomes but increasingly acts as consultant, not puppeteer.
The key is graduated responsibility with tight supervision at the start and tapered oversight as you show you’re ready.
Newness doesn’t guarantee any of that.
Here’s what actually predicts functional autonomy better than whether a program is “new”:
| Factor | What You Want to See |
|---|---|
| Clear supervision policies | Defined PGY-level expectations, not vague “you’ll see” |
| Attendings’ presence | On-site, available, not always “home call only” |
| Feedback culture | Routine, behavior-specific feedback, not just end-of-rotation |
| Resident case ownership | Longitudinal responsibility, not constant fragmentation |
| Response to errors | Learning-focused, not blame-and-hide culture |
If you don’t see these, “more autonomy” is marketing noise.
New Programs: Where They Can Shine (And Where They Burn You)
Let me be fair. New programs aren’t automatically bad. In some ways, they can be great if you’re the right kind of person and they’re decently designed.
Where new programs can genuinely offer good autonomy
Less entrenched hierarchy
In some legacy programs, there’s a rigid ladder: med student → intern → resident → fellow → junior attending. You get your slice and that’s it. A strong new program without fellows can let senior residents step into near-fellow roles—running services, teaching more, being the first line of decision-making with attending backup.Room for resident-driven systems building
New programs sometimes let residents help design handoff protocols, ICU rounding templates, onboarding materials. That’s not just autonomy in patient care; it’s autonomy in shaping the system. This can actually translate into deeper understanding and better leadership skills.Less territorialism over procedures
In some big-name places, procedures are carved up: anesthesia owns airways, IR owns lines, cardiology owns anything vaguely cardiac. New programs, especially in smaller hospitals, sometimes have a more generalist, resident-involved procedural culture—assuming there’s enough volume and supervision.
Where “autonomy” in new programs bites you
You’re cheap labor plugging staffing holes
You’ll hear: “You’ll be first-call for all ED admissions overnight, you really run the hospital.” Translation: they couldn’t recruit enough nocturnists, so congratulations, you’re it—with one attending covering three sites by phone. That’s not autonomy; that’s exploitation.No educational scaffolding exists yet
Didactic schedule being “developed”? No established exam review structure? Board pass rate “N/A, no graduates yet”? You might be walking into 3 years of reinventing the wheel rather than building skill with deliberate practice and feedback.Inconsistent supervision quality
In new programs, the attending group may be a rapid patchwork of hires. Some may love teaching and graded autonomy. Others might be burned-out community docs who never wanted residents and now see you as extra work. Crushes true autonomy, because you’ll either be micromanaged or abandoned depending on the shift.
Subspecialty Reality Check: Autonomy Is Not One-Size-Fits-All
The autonomy myth hits some specialties harder than others. Let’s be concrete.

| Category | Value |
|---|---|
| Community IM (new) | 75 |
| Legacy Tertiary IM | 60 |
| New Gen Surg | 80 |
| Legacy Gen Surg | 70 |
| New EM | 70 |
| Legacy EM | 65 |
Again, not exact data, but reflective of common patterns.
Internal Medicine: New community IM programs sometimes give PGY‑1s way more responsibility in cross-cover than big quaternary centers. But the big centers may give you more procedural autonomy in a supervised ICU setting with intensivists right there.
Surgery: The “you’ll be primary operator on everything at a new program” line ignores a key fact: case complexity and variability matter more than raw attending count. I’ve seen new programs where residents log tons of basic lap choles but almost no advanced cases. A legacy program with fellows might still give you a rich mix and structured graduated autonomy in the OR.
Emergency Medicine: EM autonomy is driven heavily by ED culture and attending presence. A new EM program attached to a community hospital with understaffed shifts can push juniors into full attending-level decision-making early, which some people romanticize—until the first miss. Strong legacy EM programs often have very robust autonomy by PGY‑2, with attendings acting as consultants, not dictators.
The point: stop using “new” as a proxy for “more autonomous.” It’s lazy and untrue.
Safety, Malpractice, and the Myth of “Trial by Fire”
Another reality people conveniently ignore: you’re not just playing with your own learning curve. You’re playing with patients’ lives and your future liability.
There’s a reason ACGME and malpractice carriers care about supervision levels. Studies in both surgery and medicine show that appropriate supervision reduces adverse events and doesn’t meaningfully stunt resident development. The idea that you need wild, unsupervised trial by fire to “really learn” is macho nonsense.
Good programs—old or new—let you:
- Make the initial call
- Commit yourself to a plan
- Then immediately staff that plan with a supervising physician who challenges, sharpens, or green-lights it
That’s where real learning lives. Not in being left alone at 3 a.m. to manage a crashing septic patient while the attending is asleep 40 minutes away.
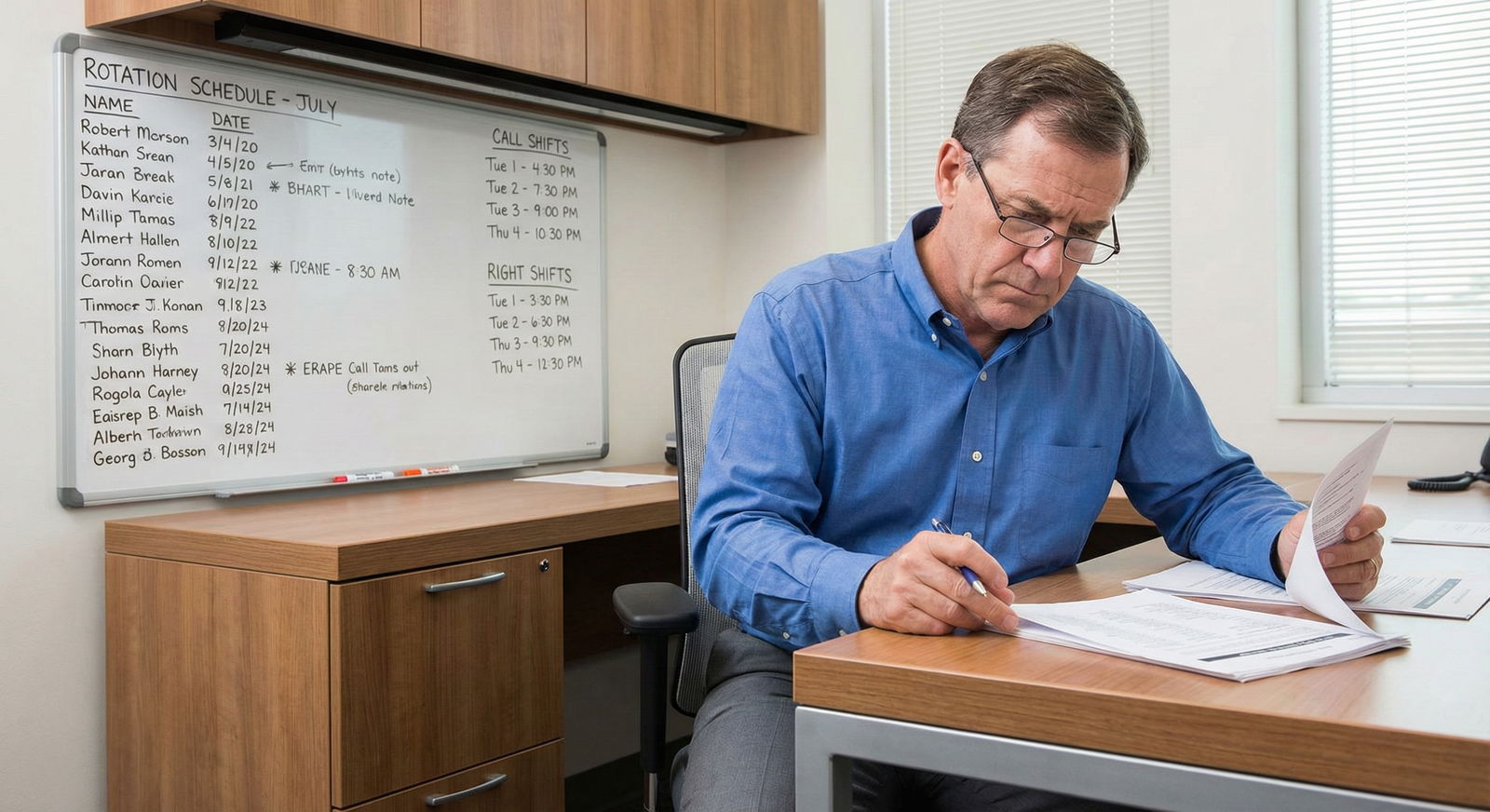
How To Actually Evaluate “Autonomy” When You Interview
If you’re serious about this, stop asking, “Do residents get a lot of autonomy?” Every program will say yes. It’s meaningless.
Ask questions that force them into specifics:
- “Who writes the initial orders on new admissions, and when does the attending usually see the patient?”
- “On nights, how many patients is the cross-cover resident responsible for, and where is the attending physically located?”
- “For codes and rapid responses, what’s the resident’s role vs the attending’s role?”
- “Can you give an example of what a typical PGY‑1 is allowed to do on day 1 of ICU versus a PGY‑3?”
- “Have there been any ACGME citations related to supervision or resident workload?”
Then watch the body language. Vague answers like “Oh, you’re very independent here” without concrete structure? Red flag.

| Step | Description |
|---|---|
| Step 1 | Ask About Night Coverage |
| Step 2 | Structured Supervision |
| Step 3 | Ask About Response Time |
| Step 4 | Potentially Safe Autonomy |
| Step 5 | Unsafe Pseudo Autonomy |
| Step 6 | Attending On Site? |
| Step 7 | Clear Policy and Support? |
You want structured supervision or potentially safe autonomy, not vague “we trust our residents, they run the place” with no backup plan.
The Future: Autonomy Will Be Measured, Whether Programs Like It Or Not
Here’s where this is heading, and where the “new program” myth is going to collide hard with reality.
- The ACGME and certifying boards are already pushing competency-based progression.
- Tools that track EPAs and supervision levels are being piloted and refined.
- Hospitals are more risk-averse, not less, as malpractice costs climb and public reporting expands.
In the near future, programs won’t be able to survive on “vibes-based autonomy.” They’ll need to demonstrate:
- When residents are entrusted with which tasks
- How supervision levels are adjusted over time
- How patient outcomes look across those transitions
New programs that are serious will build this structure from day one. Old programs will retrofit it. The wild-west “we just let the juniors figure it out” ethos will die, or get regulated out.

Bottom Line: What You Actually Want (And It’s Not Just “New”)
If you strip away the marketing and mythology, here’s what matters.
You want a program—new or old—where:
- You own your patients longitudinally and feel responsible for decisions.
- Faculty are present, accessible, and explicitly grading your independence.
- Mistakes lead to feedback and system improvement, not cover-ups and blame.
- You’re doing the work of your eventual attending role in a protected, supervised scaffold, not flying solo out of necessity.
New programs can give you that. Some do it well. Others absolutely do not.
Legacy programs can give you that. Some are outstanding. Others are suffocatingly hierarchical or so fellow-heavy that you never get to truly lead.
So stop asking, “Will I get more autonomy because it’s a new program?” That’s the wrong question.
Ask instead: “Who really carries the responsibility here, how is it shared, and how do you decide when to trust a resident with more?”
If they can’t answer that concretely, it doesn’t matter how shiny or storied the program is. The autonomy you’re imagining probably does not exist there.
Quick Reality Check: 3 Things To Remember
- “New program = more autonomy” is not a rule; it is mostly marketing. Actual autonomy depends on supervision culture, staffing, and case mix—not program age.
- You want structured, graded autonomy, not being left alone because the system is understaffed. Those are fundamentally different experiences with very different risk profiles.
- When you evaluate programs, force them into the specifics: who’s there at night, who makes which decisions, how they entrust more responsibility. If they can’t be specific, walk away—no matter how loudly they promise “you’ll really run the place.”