The biggest mistake applicants make with new residency programs is acting like they’re interviewing for any other program. You’re not. You’re about to sign up to be the experiment.
If you do not ask the right questions, you become the quality improvement project.
New programs can be fantastic—innovative, flexible, less toxic than legacy departments. They can also be absolute chaos: shifting leadership, no structure, weak teaching, and residents used as cheap labor to “get the service running.”
Here are 9 questions applicants routinely forget to ask when interviewing at new programs—and why skipping them can ruin your next 3–7 years.
1. “Who is actually responsible for building this program—and how long are they committed?”
This is the question almost no one asks directly. And it’s the one that comes back to bite them.
Everyone hears the shiny pitch:
- “We’re building something exciting.”
- “You’ll be the founding class.”
- “You’ll have a voice here.”
That’s nice. What matters is: Who is actually doing the work and how stable are they?
Ask explicitly:
- Who designed the curriculum?
- Who is the core leadership: PD, APDs, program coordinator?
- How long have they been here?
- Are they on short-term contracts or already embedded in the institution?
- Has any key leadership left since the program was approved?
If they dance around staff turnover, that’s a red flag. If the PD says something like, “Well, I’m splitting my time between here and another hospital for now…”—pay attention. That means:
- You might not have a fully present leader.
- Early problems may not get fixed.
- You’re the glue holding together multiple half-baked plans.
You want to hear:
- “I was hired specifically to build and lead this program.”
- “I plan to be here for at least the next 5+ years.”
- “We have a stable core faculty group who signed on to this long-term.”
If multiple leadership roles are “interim” or “to be hired,” you’re walking into uncertainty. Do not ignore that.
2. “What is already in place—and what is still ‘planned’ or ‘in progress’?”
New programs love words like “will,” “soon,” and “we’re working on.” That’s how applicants get fooled.
You need to separate:
- What exists now
- What is promised later
Ask them to be specific:
- Which rotations are fully set up and running today?
- Are all major sites under contract with signed affiliation agreements?
- Do you already have a full schedule for current and upcoming PGY levels?
- Which parts of the curriculum are final vs. still being designed?
If they say:
- “We’re planning to add a MICU at the community site next year”
- “We’re in talks to develop a night float system”
- “We’re hoping to expand subspecialty clinics”
…translate that in your head to: This might not exist when you’re there.
Push politely but firmly:
- “If these plans get delayed, what’s the backup?”
- “If the affiliate agreement falls through, where will we rotate instead?”
- “Is there any required rotation that is not yet fully secured?”
Do not accept vague reassurance. You want concrete descriptions like:
- “Our ICU rotation is already staffed with X attendings; we’ve had residents from another program rotating there for 2 years.”
- “We have signed agreements for all core rotations through at least the next 3 years.”
You are not evaluating their dreams. You are evaluating their reality on your start date.
3. “How has the ACGME responded so far—and what feedback have you actually received?”
Everyone asks, “Are you ACGME approved?” That’s the bare minimum, not a differentiator.
The more revealing question:
- “What feedback did the ACGME give on your initial site visit or reviews?”
- “Were any citations issued or concerns raised?”
- “How are you addressing them?”
If they refuse to give specifics or say, “Oh, it was all fine, nothing significant,” that’s suspicious. Every new program gets feedback. The question is whether they’re honest about it.
You want to hear examples like:
- “ACGME wanted clearer documentation of scholarly activity; we’ve now built a research committee and dedicated time.”
- “They asked us to shore up continuity clinic volume; we added another clinic half-day and recruited more attendings.”
Huge red flags:
- “We don’t really discuss that with applicants.”
- “There were no concerns.” (Almost never true in reality.)
- “We haven’t had a site visit yet” when they’re already recruiting multiple classes.
Also ask:
- “Have you had any follow-up reviews or progress reports?”
- “What’s your current accreditation status (initial, continued, any warning)?”
| Status Term | What It Suggests |
|---|---|
| Initial Accreditation | Normal for new programs |
| Continued Accreditation | Generally stable |
| Continued - Warning | Serious issues present |
| Probation | High-risk, avoid |
If they’re anywhere near “warning” status and they’re casual about it—walk carefully.
4. “What does a real call schedule look like for each PGY year right now?”
Do not ask, “What will the call be like?” Ask, “What is the call schedule now—and can I see it?”
New programs often underestimate workload. Or overpromise “protected time” that instantly collapses when the hospital is short-staffed.
You should press on:
- How many nights per month, average, by PGY year?
- Is there night float vs. 24-hour call?
- Who covers when census explodes—do attendings step in or is it “just the resident”?
- How often are duty hour violations reported? And what happens then?
If they say, “We’ve never had a duty-hour issue,” in a brand-new or understaffed place, that probably means one thing: underreporting. Residents are scared to complain this early.
Ask specifically:
- “Have residents ever escalated concerns about workload or duty hours?”
- “What changed in response?”
You want to hear:
- “We realized our interns were on nights too often, so we adjusted the rotation.”
- “We added a moonlighter to help when volume is high.”
- “When residents flagged an issue, we corrected it the next month.”
What you do not want:
- “Everyone just pitches in.”
- “We’re still figuring it out.”
- “There’s no perfect solution yet, but our residents are resilient.”
That’s code for: You’ll be used as flexible labor until the system stabilizes—maybe.
5. “Where are your graduates going—and if you don’t have any yet, what are you doing to set us up?”
For new programs, the single biggest unknown is outcomes.
You cannot see past fellowship match lists or job placements if they have no graduates. That doesn’t mean the program is bad. It does mean you need to ask how they’re compensating for that.
Two scenarios:
They already have at least one graduating class
- Ask: “Where did your last 1–2 classes match or take jobs?”
- Ask for ranges: academic vs. community, in-state vs. out-of-state, competitive vs. noncompetitive fellowships.
- Ask: “Were there any residents who struggled to match or find jobs? What support did they get?”
They have not yet graduated anyone
- Ask: “What’s your concrete plan for helping us with:
- Fellowship applications
- Letters of recommendation
- Networking with external programs
- “Do you already have relationships with fellowship programs or hiring groups?”
- “Have any of your faculty regularly placed residents in fellowships from prior institutions?”
- Ask: “What’s your concrete plan for helping us with:
Pay particular attention to:
- Whether faculty are known in their fields (regional/national).
- Whether anyone on staff has been a PD or APD elsewhere and understands what fellowship directors look for.
- Whether they’ve already contacted other programs saying, “We’re starting this new residency; here’s what we’re building.”
If the answer is some version of, “We’ll figure it out as we go, and you’ll help shape that,” understand what that really means: you’re the test case on the fellowship/job market.
6. “What exactly is the resident voice here—and show me one time you changed something because residents pushed for it.”
Every new program says, “Residents will have a voice.” It’s on every brochure. Worthless sentence unless you test it.
Do not stop at:
- “We have a resident council.”
- “We meet with residents quarterly.”
- “We’re very receptive to feedback.”
Push deeper:
- “Describe a specific change that was made because residents asked for it.”
- “What was the timeline from complaint to change?”
- “Has there ever been something residents pushed for that you said ‘no’ to—and why?”
You’re looking for:
- Real stories. “Our first class hated the old structure of clinic; we changed it by doing X within 3 months.”
- Evidence they can tolerate criticism without punishing people.
- A culture where residents feel safe being honest.
If the PD or faculty:
- Can’t name a single concrete example
- Only offers vague “we’re always listening” language
- Or seems defensive when you ask for specifics
…that’s a sign the “resident voice” line is mostly marketing.
New programs must be willing to iterate. If leadership is rigid this early, it only gets worse.
7. “How are you protecting wellness and psychological safety when the program is still unstable?”
Here’s the ugly truth: new programs are messier. More unknowns, more schedule changes, more ‘we didn’t anticipate this.’
That’s normal. What’s not normal is ignoring the toll that takes on residents.
Do not ask, “Do you care about wellness?” Every program will say yes.
Instead ask:
- “What formal support exists if residents are overwhelmed, burned out, or struggling mentally?”
- “Have there been any residents who needed leave or accommodations? How did the program handle that?”
- “Who do residents go to when there’s conflict with an attending or safety concern?”
Listen for:
- Access to real mental health services outside the department
- A clear, non-retaliatory reporting structure
- Examples where they backed a resident in conflict, not just faculty
Red flags:
- “We’re a family here, we don’t really have those issues.”
- “We haven’t had anyone need accommodations.”
- “We expect everyone to be resilient and adaptable with all the changes.”
Translation: if you struggle under chaotic conditions, you’ll be seen as the problem.
Ideally, they’ll say:
- “We anticipate the first few years will be bumpy, so we built in X, Y, Z safeguards.”
- “We’ve trained faculty on how to support residents in transition.”
- “We separate performance evaluation from wellness conversations so residents can be honest.”
You want infrastructure, not vibes.
8. “How do you guarantee I’ll meet case/volume and milestone requirements in a new, growing system?”
The most dangerous assumption residents make: “They can’t graduate us if we don’t meet ACGME requirements, so they’ll make sure it’s fine.” That’s not how this works in practice.
New programs frequently struggle with:
- Procedure volume
- Certain rare but required case types
- Continuity clinic numbers
- Exposure to specific environments (ICU, ED, OR volume depending on specialty)
Your question cannot be, “Will I get enough cases?” They’ll just say yes.
Instead ask:
- “What systems are in place right now to track each resident’s:
- Case logs
- Procedure numbers
- Milestone progression”
- “Have you had any residents at risk of not meeting requirements? What did you do?”
- “If a rotation site suddenly loses volume (e.g., contract change, pandemic, staffing shifts), what’s the plan B?”
You’re trying to see if they:
- Proactively monitor your numbers
- Have redundancy in rotation sites
- Have levers they can pull to boost your exposure if needed

| Category | Value |
|---|---|
| Case Volume | 85 |
| Procedures | 75 |
| Clinic Continuity | 70 |
| Supervision | 65 |
| Fellowship Support | 80 |
If the answer is, “We haven’t really run into that yet, but we don’t expect it to be a problem,” that’s not good enough. They should be borderline obsessive about tracking these things early.
9. “If the program leadership or structure changes dramatically, what protections do residents have?”
This is the nightmare scenario almost no applicant wants to look at: the PD leaves. The chair changes. The sponsoring institution merges. Suddenly the culture is unrecognizable.
In established programs, the machine tends to keep running. In a new program, a single leadership change can blow everything up.
You must ask:
- “What happens if the PD leaves? Has the institution committed to maintaining and supporting the program regardless of individual leaders?”
- “Is there an associate PD or succession plan already identified?”
- “Has the hospital made a written commitment to continue supporting the residency long term?”
Drill down:
- “Is the program financially supported by the hospital, a health system, or dependent on a specific grant?”
- “If the hospital’s finances get tight, could GME funding be cut or limited?”
You’re not just asking whether the program will exist. You’re asking whether it will still function well enough to train you properly if things change.
Healthy answers:
- “We have multiple APDs with leadership training who could step in if needed.”
- “The hospital has committed to this residency as part of a long-term strategy; it’s not dependent on a single champion.”
- “We have a designated institutional official (DIO) who oversees GME stability across all programs.”
Scary answers:
- “Oh, our PD would never leave.”
- “We’re really built around one leader’s vision.”
- “We haven’t really thought about succession; we’re just getting started.”
That’s exactly the problem. You’ll be in PGY-2 when they start “thinking about it.”
How to Actually Ask These Questions Without Tanking Your Interview
One more mistake: applicants know these are good questions but are scared to sound “negative.” So they stay quiet and hope for the best. Bad strategy.
You can ask hard questions and still look professional if you frame them right:
- Use curiosity, not accusation: “I’m really interested in how you’re building this from the ground up—can you tell me…”
- Tie it to your priorities: “I want to be part of a place that’s committed to long-term improvement, so I’m wondering…”
- Stay calm and neutral. Do not sound anxious or hostile, just matter-of-fact.
Try grouping questions:
- Ask the PD about ACGME feedback, leadership stability, and future plans.
- Ask chief residents about real call schedules, workload, and changes based on feedback.
- Ask current interns about how often schedules change and how responsive leadership is.
And pay more attention to how they answer than the exact words:
- Do they get defensive?
- Do they talk in specifics, or just slogans?
- Do different people give conflicting information?
If the vibe is, “Stop asking difficult questions and just trust us,” you already have your answer.
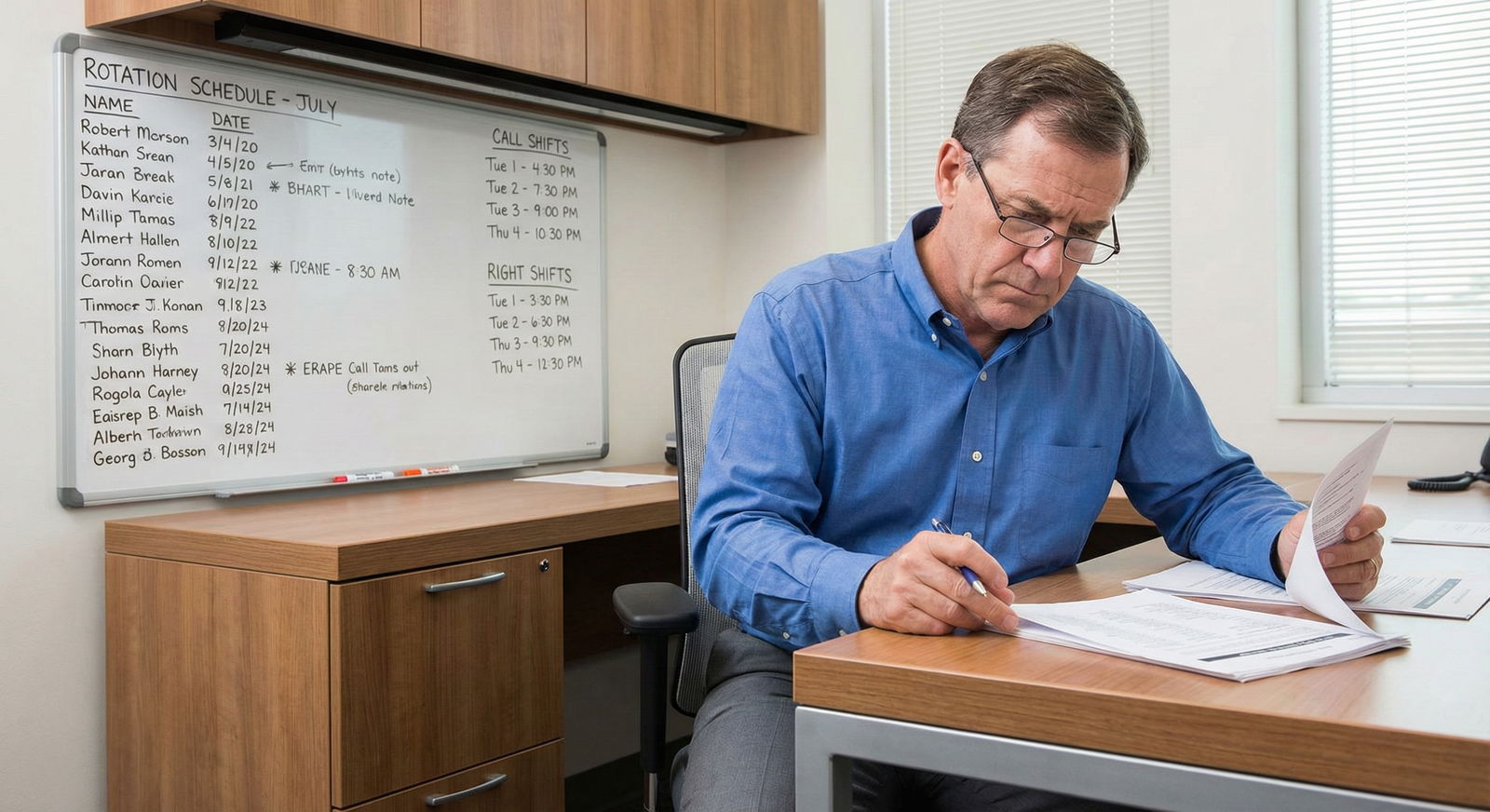
Two Visual Red Flags You Should Not Ignore
Watch for these on interview day; they’re subtle but real:

Chaotic resident workroom and zero structure
- Whiteboards with half-erased schedules
- Residents have no idea what their next block is
- Everyone “thinks” someone else handles X rotation
No one can clearly explain the next 2–3 years
- PD gives a vague, hand-wavy overview
- Residents say “things change a lot” but can’t describe a consistent plan
- Faculty each describe a different model of the program
That’s not “flexibility.” That’s disorganization dressed up as innovation.
Bottom Line: What You Cannot Afford to Forget
If you remember nothing else, remember this:
- New residency programs are not automatically bad—but they are automatically higher risk.
- Your job as an applicant is not to be polite and impressed. Your job is to protect your training and your future.
- The biggest mistake is accepting big promises without forcing them to show you what actually exists right now.
Ask the hard questions. Demand specifics. Walk away if the answers are all vibes and no structure. Your degree got you to the interview; your judgment gets you through residency intact.















