
The day your program gets initial ACGME accreditation is not the victory lap people think it is. It’s the starting gun for a very quiet, very high‑stakes scramble that most applicants – and frankly, most residents – never see.
Let me walk you through what actually happens inside a brand‑new program once that “Initial Accreditation” letter hits the PD’s inbox. This is the unwritten playbook program directors pass to each other in hallway conversations, not in official ACGME manuals.
The Moment the Letter Drops: Panic-In-A-Blazer
Here’s the truth: most programs apply to ACGME before they’re really ready to run a mature residency. They have enough on paper to pass review – bylaws, faculty lists, policy manuals, sample rotation schedules – but the operational side is held together with optimism and templates borrowed from three different institutions.
The day the Initial Accreditation email arrives, three things happen in rapid sequence:
- The PD forwards it to leadership with way too many exclamation points.
- GME posts a cautiously celebratory announcement.
- A closed‑door meeting happens where someone says, “Alright. Now we actually have to build this thing.”
Behind that door, the conversation is not “We did it.” It’s:
- How fast can we get into ERAS?
- What can we realistically handle for PGY‑1 headcount?
- Who’s actually going to teach on July 1? Not on paper. In real life. On nights. With midnights admits.
And then the timeline clock starts ticking.

| Period | Event |
|---|---|
| Month 0-1 - Initial Accreditation Letter | Program approved |
| Month 0-1 - Internal Strategy Meeting | Leadership alignment |
| Month 1-3 - ERAS Participation Request | NRMP decision |
| Month 1-3 - Recruitment Branding | Website and materials |
| Month 4-9 - Interview Season | Applicant selection |
| Month 4-9 - Rotation Finalization | Block schedules locked |
| Month 10-12 - Rank List Submission | NRMP deadline |
| Month 10-12 - Pre-July Onboarding | Systems and policies live |
The Quiet War: Headcount vs. Reality
Nobody talks about this publicly, but new programs obsess over one number: initial complement. That’s the approved number of residents per class. And it’s a political landmine.
On paper, leadership wants big numbers. Residents bring labor, prestige, and eventually fellowship leverage. In reality, the PD knows:
- Too small an initial class and you look weak and unappealing.
- Too big and your first few classes become unpaid beta testers for a broken system.
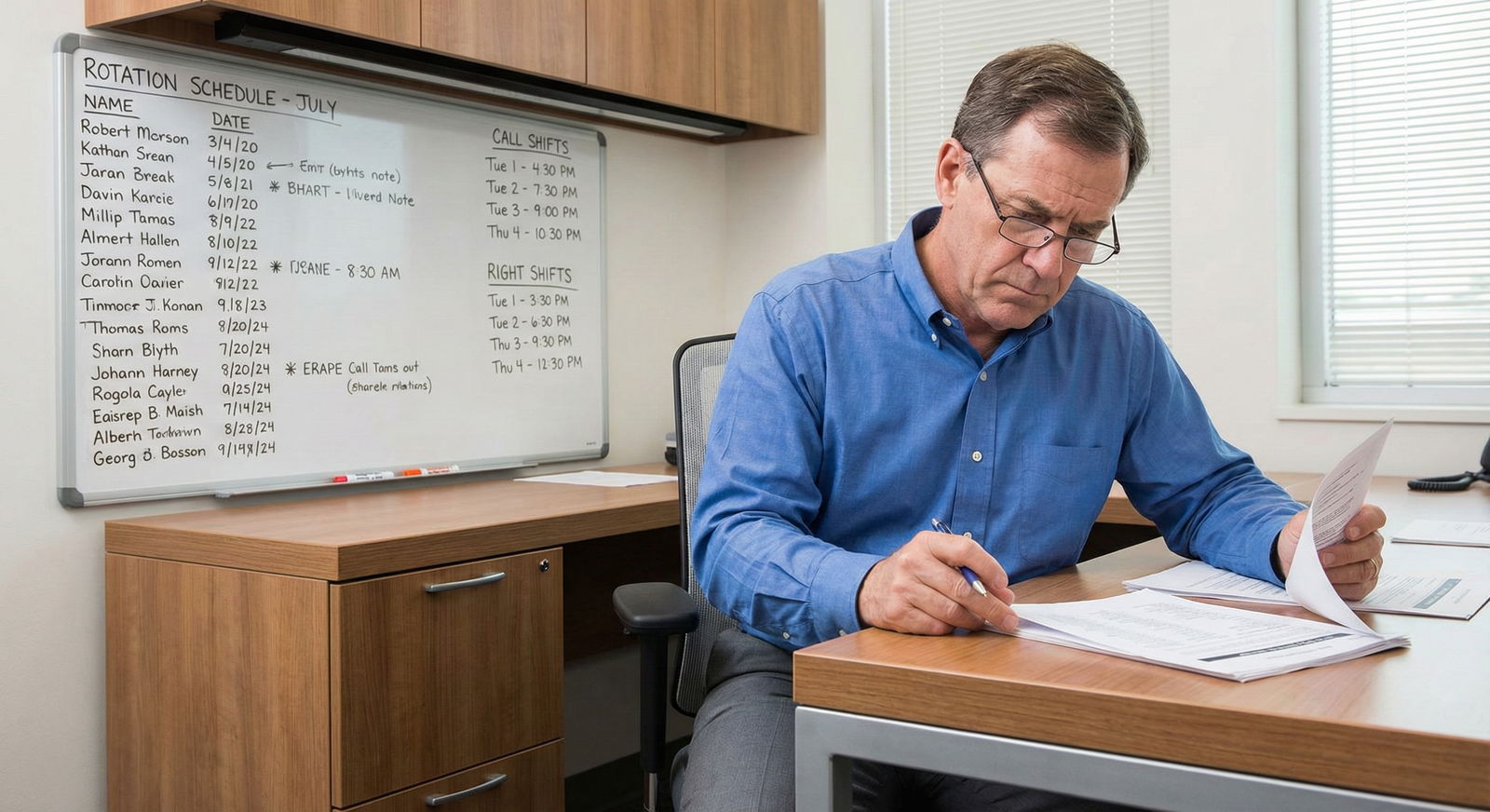
I’ve sat in a room where a brand‑new IM program director was being pushed to start with 15–18 interns. She slid a call schedule across the table and said, “Show me how you cover nights, clinics, electives, and still let them sleep.” They started with 8 instead.
Here’s how the discussion really goes:
- C‑suite: “We want 12–15. We need bodies on the wards and coverage for the new service line.”
- PD: “We have 4 people who can reliably teach and sign notes. The rest are ‘interested in education’ as long as it doesn’t interfere with their RVUs.”
- DIO: “Remember, ACGME will be back in 2–3 years. If they walk in and see 15 overworked, undersupported interns, we’re dead.”
So the first “post‑approval” move is not public at all. It’s a quiet recalibration of what the institution told ACGME during the application versus what they’re actually going to try to run.
And yes, they absolutely will “slow-roll” to their full complement if they’re smart.
ERAS, NRMP, and the Brand-Name Problem
Once accreditation hits, the next obsession is: can we make ourselves look like a real player in one application cycle or will this take three?
New programs have a branding problem. You can be clinically excellent, but to applicants you’re a risk: no alumni, no word of mouth, no proven board pass rate, no culture.
Here’s what programs actually do behind the scenes.
1. Fast-tracking ERAS and NRMP decisions
They get on the phone with ERAS and NRMP immediately:
- “Can we get into ERAS this season?”
- “What dates do we need to hit for Match participation?”
- “If we miss this window, what are our options for a SOAP or off-cycle recruitment?”
If the timing is late, some programs quietly decide to delay their first class a full year rather than scramble into a half‑baked interview season. The PD won’t say this to applicants, but the internal logic is simple: better to start strong in 12 months than fill half a class with panicked SOAP candidates right now.
2. Constructing a “track record” they don’t really have
You’ve seen these new program websites. They all sound the same: “robust clinical exposure,” “diverse patient population,” “strong faculty commitment to education.”
Internally, they’re asking:
- How can we borrow legitimacy?
- Can we say “affiliated with X University” even if we’re only a teaching site?
- Can we list that star subspecialist who agreed to be “core faculty” but lives mostly in the OR?
Faculty bios are rewritten aggressively. That one pulmonary doc who once gave a noon conference at a big‑name academic center? Congratulations, now your website says “Trained at [Top-10 Institution], brings academic rigor to our program.”
Nobody’s technically lying, but you’ll see a lot of selective framing.
3. Deciding which applicants they’re really targeting
Every new PD has to decide: are we aiming for:
- The “geography or life‑situation” applicants (need to stay local, couples match issues, visas)?
- The “late bloomers” who improved over time?
- The “high‑risk, high‑ceiling” candidates big-name programs overlooked?
Behind closed doors, the PD will say openly: “We are not matching the Harvard med students this year. Let’s build a program that can truly support the residents we will get.”
The smart ones adjust expectations and build a program that doesn’t depend on super‑polished, hyper‑independent interns to keep the place from collapsing.

| Category | Value |
|---|---|
| Local students | 30 |
| Out-of-region DO/MD | 25 |
| International grads | 35 |
| SOAP/off-cycle | 10 |
The Hidden Curriculum for Faculty: “You’re Teaching Now”
ACGME approval binds more than just the PD. It quietly conscripts a whole set of attendings into a new way of working.
Here’s how this really unfolds.
The reluctant attending problem
Most hospitals do not start residency programs because their faculty woke up one day desperate to teach. They start them because:
- They want to be “an academic medical center.”
- They need residents to staff expanding services.
- They think it’ll help recruit and retain physicians.
So your core faculty list usually includes:
- 30% true educators who are thrilled.
- 40% “I’m open to it as long as it doesn’t destroy my clinic flow.”
- 30% who said yes because their chair volunteered them, and they’re already planning to dodge it.
After approval, the PD’s unofficial job description becomes “behavior change specialist.” There are a lot of closed‑door 1:1s that go like this:
“Your no‑show rate for teaching conferences is obvious to the residents. If you want to stay core faculty, that has to change before the site visit.”
“I watched you round with the students last month. The way you spoke to nursing will get us cited. Fix it.”
None of that makes it into faculty meeting minutes, but it absolutely happens.
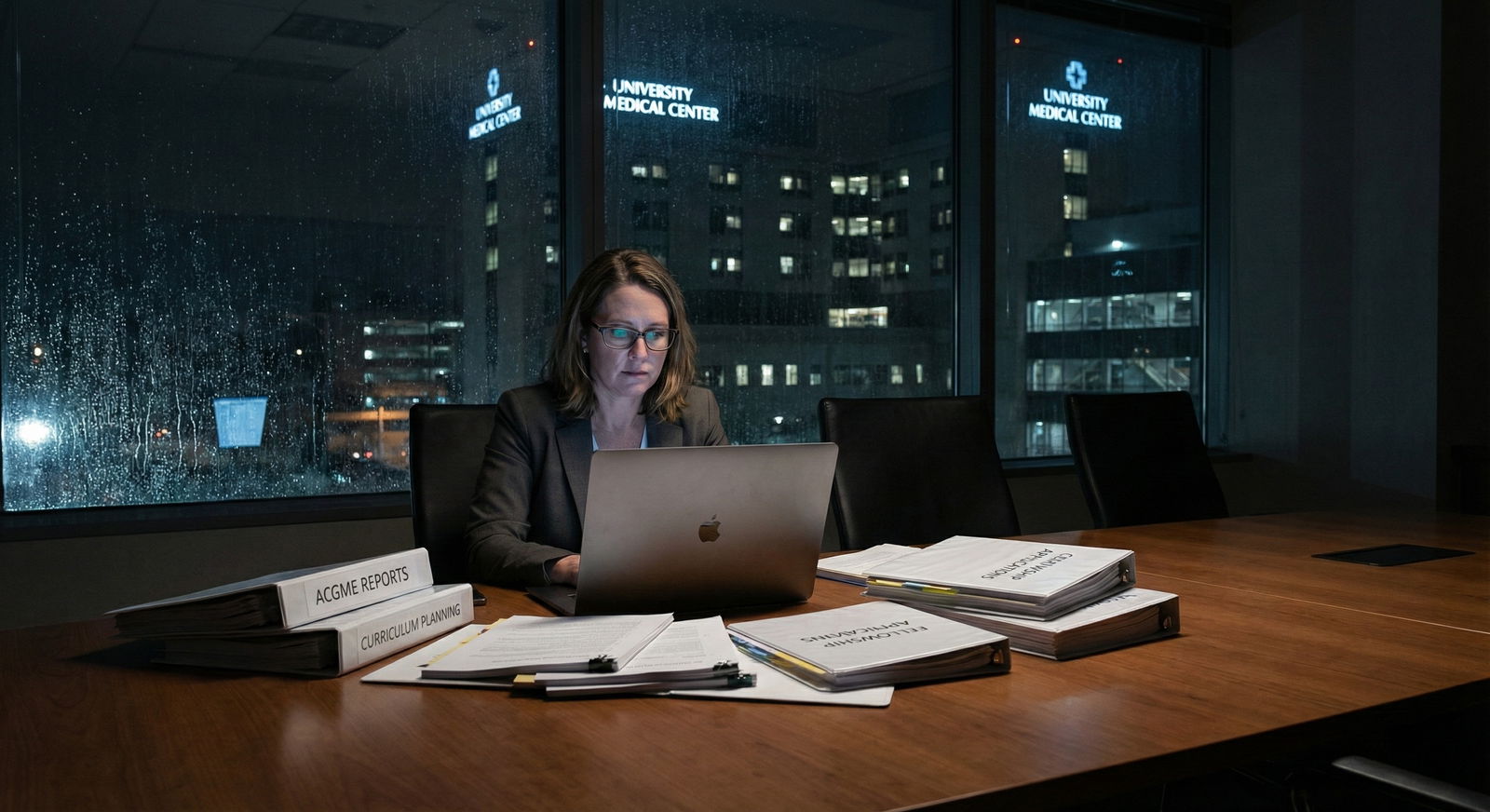
Building the fake-it-then-make-it educational infrastructure
The ACGME application forces programs to have policies and structures on paper. After approval, everyone realizes they now have to live by what they wrote.
- That elegant evaluation system they showed to ACGME? It’s really a half‑configured MedHub/New Innovations instance and a few shared spreadsheets.
- The “robust didactic curriculum” is still mostly stolen slide decks and last year’s CME talks.
- The “faculty development plan” is a lightly attended lunchtime workshop with dry sandwiches.
First year, the real work is turning templates into habits. Getting attendings to actually:
- Complete evaluations within 7 days.
- Show up on time for protected didactics.
- Treat residents like learners, not cheap NPs.
The PD’s internal metric isn’t “Do we have a rotation description?” It’s “When ACGME calls PGY‑1s during our site visit, will they describe a real curriculum or just say, ‘We mostly just work on the wards’?”

The Residents They Really Want vs. The Residents They Accept
This part applicants never hear but should understand.
During that first recruitment season, the PD and recruitment committee build two mental lists:
- The residents they fantasize about getting.
- The residents they can build with.
Fantasies: 250+ Step 2, AOA, multiple publications, polished communicators who could easily have matched at established university programs but “love building something new.” Those exist, but they’re rare, and most are not going to rank a program that doesn’t have a single graduate yet.
Builders: solid, hungry, slightly overlooked candidates who want hands-on experience, leadership roles, and are willing to tolerate some chaos in exchange for opportunity.
The unwritten rule among PDs of new programs is this: take hungry over shiny.
I’ve watched PDs pass on a higher‑scoring but clearly disengaged applicant to rank a slightly “riskier” candidate who lit up when they started talking about quality improvement or teaching medical students. Every time, they were happier with that choice.
Because in a new program, your first two classes aren’t just residents. They are co‑architects. If they show up expecting everything to be pre‑built like a 50‑year-old flagship program, they will be miserable and loud about it.
| Trait | Priority Level |
|---|---|
| Willingness to give feedback and build | Very High |
| Flexibility with workflows | Very High |
| Step/COMLEX scores | Moderate |
| Name-brand school pedigree | Low–Moderate |
| Desire for leadership roles | Very High |
| Tolerance for uncertainty | Critical |
The First July 1: Controlled Chaos
You think July 1 is chaotic at an established residency? Double it and add uncertainty.
Here’s what happens behind the scenes that you’ll never see in the glossy brochure.
Every system is being tested live
Duty hour tracking, evaluation systems, handoff tools, sign-out workflows, EHR permissions. Half of it has never really been stress‑tested with residents in the loop.
Common internal questions in that first month:
- “Why can’t the interns see X note type in the EHR?”
- “Who actually approves their time‑off requests? Because they’re asking everyone.”
- “Did anyone tell pharmacy they can page the night float?”
- “Who is covering them when they go to clinic? No, really, who?”
The PD is putting out fires daily while pretending to the outside world that everything is “going great.”
PDs are watching like hawks
In those first 4–8 weeks, the PD isn’t actually judging residents primarily on raw knowledge. They’re watching for:
- Who owns mistakes.
- Who disappears during hard shifts.
- Who speaks up about safety issues instead of quietly compensating.
- Who shows early signs of unprofessionalism or emotional volatility.
Not because they’re eager to punish. Because in a brand-new program, ACGME will come hard if there are early patterns of duty hour violations, bad culture, or unsafe care. A single problem resident in a 5‑person class isn’t just “a challenge.” It’s a systemic risk.
And yes, people get quietly counseled out in year one if they are clearly a disastrous fit. PDs will bend over backwards with remediation, but they will not sacrifice the survival of the program for one resident.

| Category | Value |
|---|---|
| Duty hour tracking | 70 |
| Scheduling gaps | 55 |
| EHR access | 40 |
| Missing evaluations | 65 |
| Conference attendance | 50 |
The ACGME Shadow: Living for the Next Site Visit
Initial accreditation isn’t permanent. The clock starts toward continued accreditation, and PDs live under that shadow.
Here’s the unspoken part:
Every significant decision in the first 2–3 years is quietly run through the filter: “If ACGME saw this up close, would they trust us?”
- Thinking about letting residents routinely cross 80 hours? Absolutely not. Someone will be fired before they allow a pattern to be documented.
- Considering loosening supervision overnight? Not until there’s a proven track record.
- Contemplating a politically popular but educationally useless rotation? It’ll quietly get cut if it jeopardizes case logs or core requirements.
Residents often think, “Why is my PD so rigid about X?” The answer, often, is: there is an ACGME field rep and a Review Committee that will take our accreditation if we’re sloppy.
That’s also why your PD pushes you so hard to complete surveys and evaluations. Your ACGME resident survey responses are ammunition – for or against the program. If the early cohorts torch the place on that survey, it’s not just an awkward conversation. It can trigger focused visits, citations, and in the worst cases, non‑continuation of accreditation.
What This Means If You’re Considering a New Program
Let me give you the blunt, behind‑the‑curtain view.
If you’re an applicant, and you’re considering ranking a new program with fresh initial accreditation:
You are not signing up for a finished product. You are signing up to influence the blueprint.
Programs that succeed do a few things consistently post‑approval:
- They’re honest with residents about what’s still being built.
- They over‑invest in communication and feedback loops.
- The PD is visible, accessible, and clearly in charge (not just a figurehead under a chair or service line VP).
- They protect education time ruthlessly, even against a hospital screaming for service coverage.
Programs that fail to mature?
You’ll see the signs early if you know where to look:
- Faculty bad‑mouth residents to nursing or consultants.
- Didactics are constantly canceled “because the floor is busy.”
- Nobody can explain who actually handles your concerns. It’s always “Talk to X,” and X sends you to Y.
- The PD seems more scared of the CMO than of losing accreditation.
The real playbook PDs share with each other privately is simple: treat your first three classes like co‑founders, not cheap labor.
If they’re doing that, you’ll feel it when you interview. If they’re not, politely thank them for their time and rank them accordingly.
Years from now, you won’t remember the exact language of the ACGME letter or the hospital press release. You’ll remember whether the people who built that program with you were honest, responsive, and willing to fix what was broken while you were living through it. That’s the difference between being “first class collateral damage” and being part of something you’re actually proud to have started.
FAQ
1. How risky is it really to match into a brand‑new ACGME program?
Risk is real but nuanced. The program’s accreditation itself is unlikely to vanish overnight; ACGME usually works with programs through citations and action plans. The bigger risk is quality of your day‑to‑day training: disorganized rotations, weak supervision, and culture problems. Talk directly with the PD and early faculty, and if possible, current or incoming residents. If leadership is transparent, responsive, and knows their own weaknesses, that’s a good sign. If they’re defensive or selling hard, be cautious.
2. What specific questions should I ask on interview day at a new program?
Ask how they used feedback from their first cohort (or from their planning phase) to change the program. Ask who actually handles schedule changes, conflict resolution, remediation, and wellness. Ask what they’re most worried about for the next ACGME visit. The content of their answers matters, but their tone matters more. You want thoughtful, concrete examples, not vague reassurance.
3. Can a new program really set me up for competitive fellowships or jobs?
Yes, but not automatically. You’ll likely get more hands‑on experience and leadership roles early, which fellowship directors respect if you can articulate what you did. What you may lack is brand recognition and established pipelines. That means you’ll need stronger networking, research/quality projects, and intentional letter‑writers. Good PDs of new programs will actively help you with that – connecting you to colleagues at other institutions, pushing you into presentations, and guarding your reputation. If they shrug when you ask about fellowship or job placement plans, that’s a red flag.














