It’s January. You’re a fourth-year scrolling through FREIDA and you see it: “ACGME Initial Accreditation – First Match.” Brand new residency program. Shiny website. Lots of words like “innovative,” “supportive,” “growing rapidly.”
You’re tempted. Less competition, chance to be “founding class,” maybe fast leadership roles.
What you don’t see on the website: the chair who’s halfway out the door. The core faculty arguing over whether they even want residents. The APD who’s already interviewing for a job across the country. Or the fact that the clinic where you’d spend 60% of your time might switch ownership after your PGY-1 year.
Let me walk you through what actually happens inside new programs in their first three Match cycles – and how faculty turnover quietly makes or breaks them.
The Hidden Reality of “New Program” Faculty
Here’s the first thing nobody tells applicants: brand new programs almost never have stable faculty for the first three years. They just don’t.
To launch a new residency, leadership cobbles together:
- A PD who usually has “0.2–0.3 FTE” for education on paper and three full-time jobs in reality
- Core faculty who were voluntold into teaching residents
- A chair or chief who promised the GME committee they’re “fully committed” while planning a move in 24–36 months
There are exceptions. But if you assume churn, you’re more right than wrong.

| Category | Value |
|---|---|
| Year 1 | 15 |
| Year 2 | 30 |
| Year 3 | 40 |
Those numbers aren’t in any official report. They’re the kind of back-of-the-envelope estimates I’ve heard PDs share over drinks at APDIM and CORD meetings when the microphones are off.
Here’s the pattern I’ve watched repeat:
Year 0–1: Enthusiastic start. Everyone’s “all in.”
Year 1–2: Reality hits. Workload spikes. Billing drops. People start looking.
Year 2–3: One or two key faculty leave. Sometimes the PD. Sometimes the chair. Occasionally both.
That’s the context you’re walking into as an applicant or new resident.
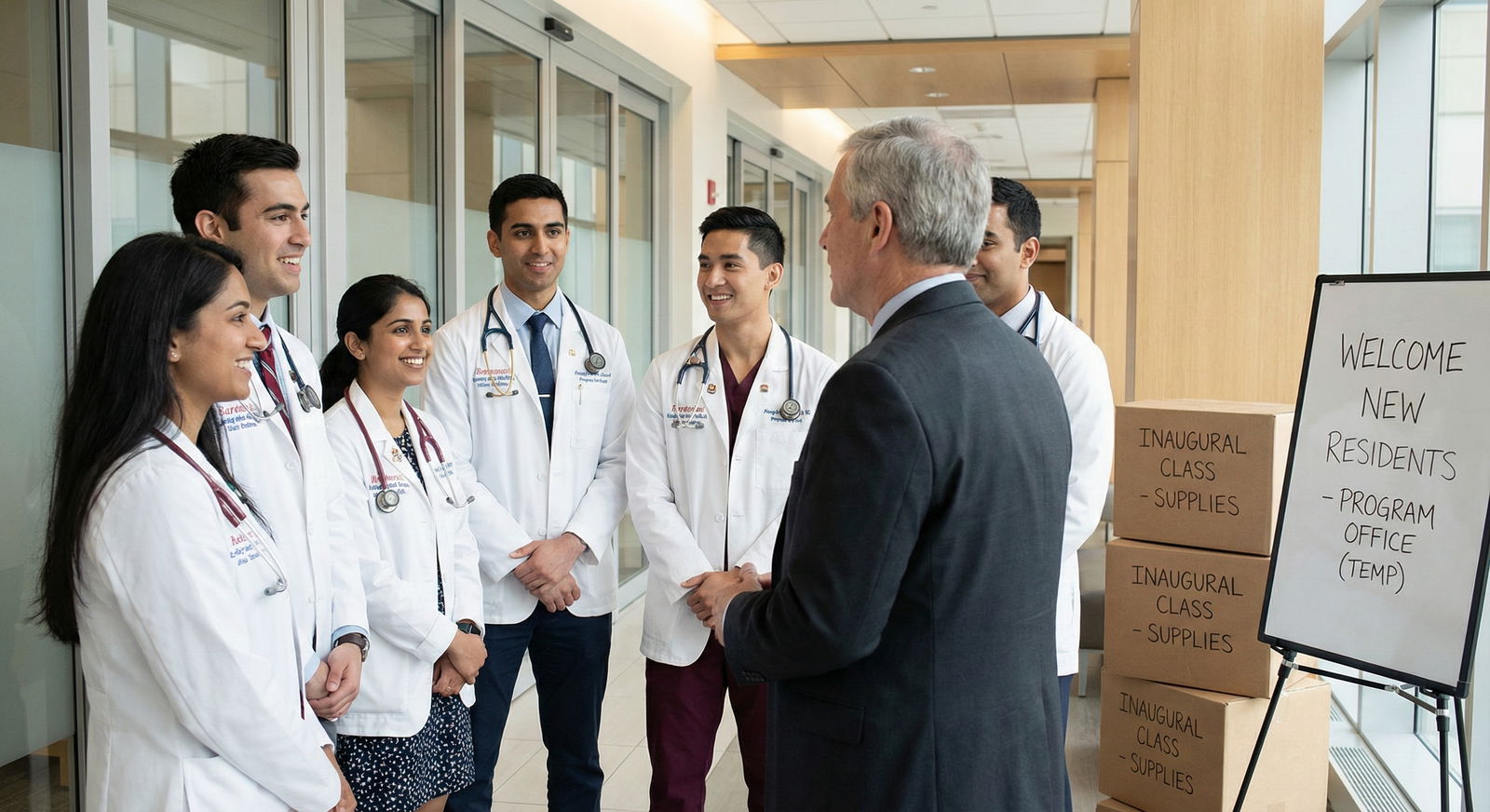
Match Cycle 1: The Honeymoon and the Mirage
The first Match cycle is smoke and mirrors, in both directions.
Programs are trying to look bigger, more stable, more established than they are. Applicants are trying to guess risk from a website and one interview day.
What’s really happening behind the scenes
During that first recruitment season:
- The PD is still learning how to be a PD
- Faculty titles are being handed out like candy: “You’re core. You’re associate PD. You’re research director.”
- The hospital CFO is watching the numbers and asking, “Why are these doctors seeing fewer patients?”
I’ve sat in those early faculty meetings. You’ll hear things like:
- “We’ll just all precept one extra half-day.”
- “We can cover nights with faculty and moonlighters until we build up the resident classes.”
- “Let’s promise robust mentorship; we’ll figure out the details later.”
Translation: unsustainably high faculty workload disguised as “founding program energy.”
The key risk in Match 1 isn’t that people are leaving yet. It’s that leadership is overpromising based on a faculty structure that will not survive contact with reality.
How that impacts you as a member of the first class
If you match into that inaugural class, your PGY-1 year will feel like this:
- Access to attendings is great – at first. They’re excited to teach, they’re on rounds a lot, they know your name.
- Schedules are fluid and somewhat chaotic. Rotations get built on the fly.
- “We’re building this together” is said so often you start mentally billing for consulting.
But behind the scenes, some faculty are already thinking, “This isn’t what I signed up for.” They’re seeing:
- Longer days because residents slow down their clinics and inpatient lists
- More non-RVU work: evaluations, CCC meetings, lectures
- No real financial recognition for education work
If you want the real tell-tale sign: pay attention to what happens right after your first class matches. How many faculty quietly update LinkedIn or start showing up at national meetings asking “So… how’s your program?” – code for “Got any jobs?”

Match Cycle 2: The Shakeout Year
The second Match cycle is where you really see the impact of faculty turnover.
This is the year two major things collide:
- The first class is fully on service and generating the “pain” and “benefit” of having residents.
- Faculty who were already 50/50 on staying now have hard data on how their lives changed.
Who leaves and why
The most common flight pattern I’ve seen by the second year:
- Senior “rainmaker” faculty (high RVU, high billing) who never wanted residents in the first place
- Mid-career attendings who thought they’d have protected time and realized it was a lie
- Young faculty who came “for the education” but realize nobody’s backfilling their clinical load
Let me be blunt: money drives more of this than anyone admits publicly.
RVU-heavy departments (medicine, EM, surgery) quickly realize that education is expensive if you don’t structurally plan for it. Admin starts sending emails.
You’ll hear phrases like:
- “We need to get back to productivity benchmarks.”
- “Everyone has to do their part during this growth phase.”
- “Once the program is established, we can revisit the FTE distribution.”
Translation: the people pulling the biggest clinical numbers get fed up and leave for jobs where their work is valued and not diluted by educational duties.
How turnover shows up in the second Match
Now, on the recruitment side, here’s where it gets interesting.
Programs have to keep the marketing shiny while quietly navigating real instability. You’ll see things on interview day like:
- “We’re in a period of exciting growth” instead of “We just lost two core faculty.”
- “We’re reimagining our continuity clinic model” instead of “Your clinic attendings keep quitting.”
- “We’re restructuring leadership to better support residents” instead of “Our PD stepped down and we promoted the only person who said yes.”
| What You See Publicly | What It Often Means Internally |
|---|---|
| New interim PD or APD | Prior leader left or was pushed out |
| “Transitioning to a new clinic site” | Contract ended or private group pulled out |
| Heavy emphasis on “resident leadership” | Faculty capacity is thin |
| Lots of locums/PRN names on schedules | Difficulty recruiting stable faculty |
| Frequent mention of “ongoing changes” | Turnover or pressure from administration |
If you’re interviewing in that second Match cycle, your job is to read between the lines. Ask very concrete questions:
- “How many core faculty have been here since the program started?”
- “How many left in the last year?”
- “Who evaluates you and how often do they physically work with residents?”
If the PD tap-dances around those, you’ve got your answer.
Match Cycle 3: The Inflection Point
By the third Match cycle, most new programs hit one of two paths:
Path A: Stabilization – Leadership and faculty adjust expectations, workload is redistributed, and the program starts to look like a real, functioning residency.
Path B: Chronic churn – Leadership changes again, recruitment becomes harder, and the program develops a reputation that applicants pick up on (even if nobody says it out loud on the website).
What faculty turnover looks like in year 3
Here’s the quiet metric chairs and GME offices use that you’ll never see published: “How many core faculty have been replaced since we started?” Once that hits about 40–50% by year three, alarm bells go off.
Why? Because you’re constantly onboarding new faculty into:
- The ACGME requirements
- The culture of the program
- The unwritten expectations (who actually writes notes, who rounds where, who calls families, etc.)
You’ll see instability bleed into resident life:
- Rotation descriptions on paper and what actually happens diverge
- The attending who was supposed to be your mentor is suddenly “no longer with the institution”
- CCC and PEC meetings are run by people who barely know the residents they’re evaluating

| Category | Value |
|---|---|
| Year 1 | 80 |
| Year 2 | 65 |
| Year 3 | 50 |
That “resident experience score” isn’t from a formal survey; it’s the composite of what you hear in the hallways, in anonymous ACGME surveys, and in the way residents talk about their days when leadership isn’t around.
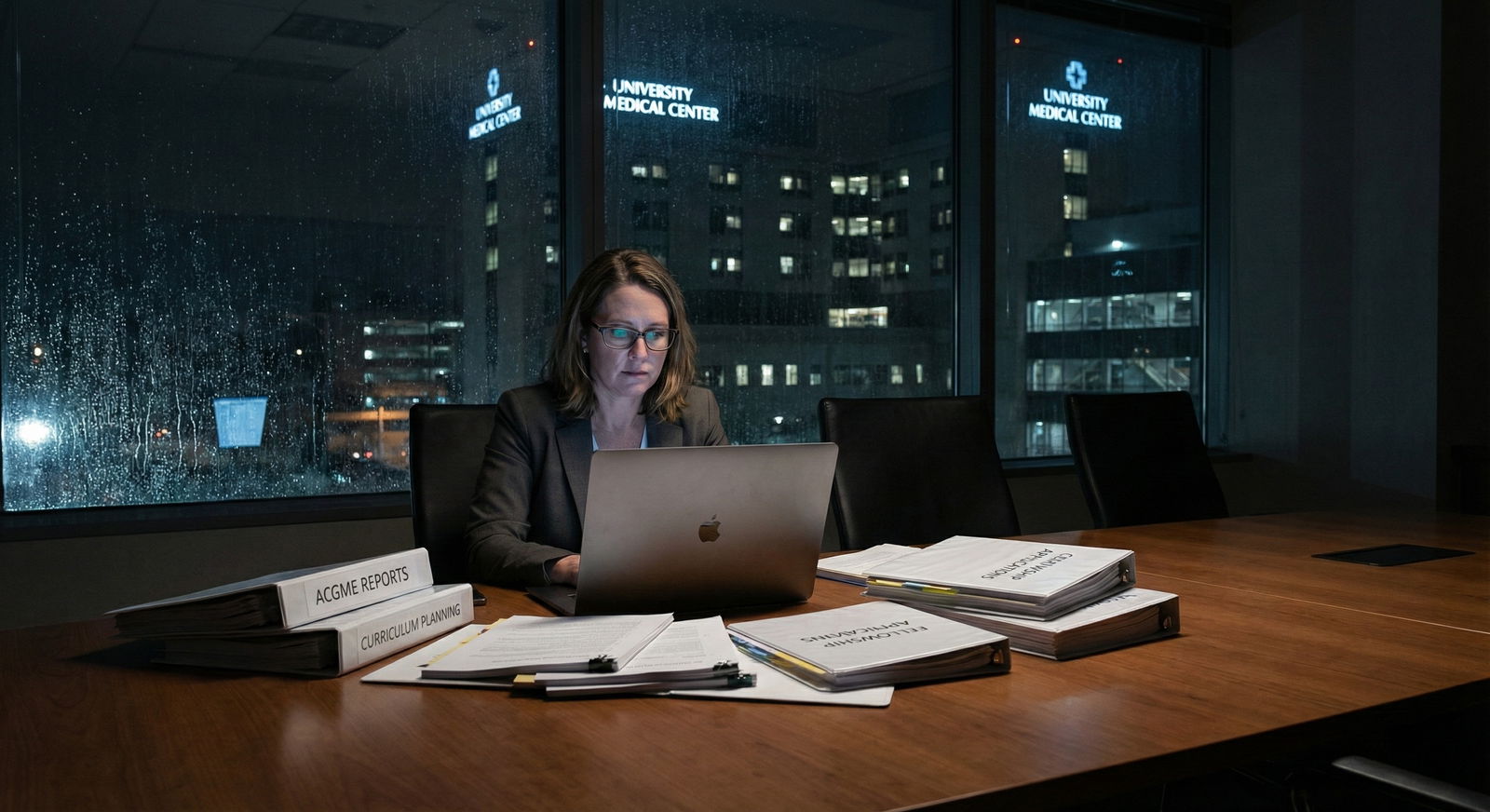
The power struggle you’ll never be told about
By year three, there’s usually a tug-of-war going on:
- GME and the PD want to preserve educational time and sane workloads
- The hospital wants RVUs, throughput, and cost control
- Faculty are trying to protect their sanity and career trajectory
If turnover has been high, administration often pushes harder, not softer: “You’re losing people; clearly you’re not efficient. Do more with less.”
If leadership is strong and stable, they push back: “We need protected time and backfill or residents will suffer, and then our accreditation will suffer.”
That power struggle directly determines whether your third- and fourth-year experience is shaped by “We’re growing and improving” or “We’re in perpetual crisis mode.”

How Faculty Turnover Changes What You Actually Live Through
Let’s get concrete. What does faculty turnover actually change in your day-to-day life as a resident in these early years?
1. Clinical teaching quality
High churn means you’re constantly orienting new attendings who:
- Don’t know the documentation templates
- Don’t understand resident scope at that hospital
- Haven’t internalized the program’s expectations for autonomy
You end up doing a lot of “explaining the system” upward. Which sounds empowering until you’re PGY-1 trying to convince a new hospitalist that yes, you are actually allowed to place those orders.
2. Consistency of feedback and evaluations
When faculty keep leaving:
- Your milestone evaluations are written by people who barely know you
- Feedback whiplash happens: one attending says you’re “too slow,” next one says you’re “too fast and unsafe”
- Letters of recommendation for fellowships come from people with shallow longitudinal experience
That hurts you when you apply for fellowship or jobs. PDs reading LORs can tell the difference between “I’ve worked with this resident closely for two years” and “I met this person last month and they seem nice.”
3. Culture and psychological safety
Stable faculty create predictable expectations. Unstable faculty culture feels like:
- “Which attending is on? Okay, today we can do X, but tomorrow that same thing will get us yelled at.”
- Residents policing each other: “Don’t do that on Dr. ___’s service, they hate it.”
- Whisper networks about which new faculty are “malignant,” “checked out,” or “amazing and probably leaving in a year.”
If you’re seeing wildly different vibes from rotation to rotation in a small hospital, that’s usually turnover talking.
4. Curriculum and innovation
New programs sell themselves on being “innovative.” Reality: innovation requires time, bandwidth, and faculty continuity.
When turnover is high:
- Didactic schedules get thrown together last-minute
- QI and research projects die when the faculty mentor leaves
- The “cool new curriculum” never gets evaluated or iterated – it just exists on paper
This is why some three-year-old programs already feel stale. The people who cared enough to build new things left, and the people who stayed are underwater.

| Step | Description |
|---|---|
| Step 1 | Program Launch |
| Step 2 | Match 1 - Honeymoon |
| Step 3 | Minor Turnover |
| Step 4 | Major Turnover |
| Step 5 | Match 2 - Adjusted Expectations |
| Step 6 | Match 2 - Instability |
| Step 7 | Match 3 - Stabilization Path |
| Step 8 | Match 3 - Chronic Churn |
| Step 9 | Resident Experience Improves |
| Step 10 | Resident Experience Erodes |
| Step 11 | Faculty Workload Realization |
| Step 12 | Strong Leadership |
How to Read a New Program’s Future From Its Faculty
You can’t control turnover. But you can read it. And you absolutely should if you’re considering ranking a new program anywhere near the top of your list.
Here’s the insider playbook.
Look for actual named humans, not generic titles
On the website and during interviews:
- How many core faculty are listed by name with real bios?
- Do they seem like people who have ties to the region (family, long-standing jobs) or short-term visitors?
- Do the “leaders” have a track record in GME or were they just knighted last month?
If the website has two faculty bios and ten “TBD” or “Faculty coming soon,” that tells you exactly how much continuity you can expect.
Compare who interviewed you to who is actually there
This one’s subtle but powerful.
When you interview:
- Ask how long each faculty interviewer has been at the institution
- Ask what they did before joining the program
- Quietly note how many seem to be new in the past year
If half the interviewers say something like, “I just joined from [other institution] six months ago,” that’s not pure growth; that’s often replacement.
Ask residents targeted questions
Do not waste resident Q&A time on vague “Are people nice?” questions. Ask:
- “How many attendings that you worked with as an intern are still here?”
- “Has your PD or chair changed since you matched?”
- “Have any of your key mentors left? How was that handled?”
- “Do you feel like the program is more stable now than when you started, or less?”
Listen less to the words and more to the pauses and facial expressions. Residents are often coached on how to answer, but they’re not professional actors.
The Future: Why This Will Matter Even More
Here’s the part people are still underestimating: faculty turnover in new programs is going to get worse over the next decade, not better.
A few reasons:
- Burnout and early retirement: Mid-career and senior faculty are leaving clinical practice earlier, especially in high-burnout specialties. New programs lean heavily on that exact group.
- Corporate consolidation: Hospital systems are merging, reshuffling contracts, and cutting “non-productive” time. Education FTE is always on the chopping block.
- Remote and hybrid work: Some faculty can now work telehealth or administrative jobs from home with less hassle, which makes “come build a new residency with tons of in-person responsibility” a harder sell.
- ACGME pressure: As accreditation standards tighten, new programs will need more documented faculty time and involvement. That’s good for residents, but only if the hospital is willing to pay for it. Many will not.
What this means for you: every new program you consider exists in a more volatile ecosystem than the one before it. That doesn’t mean you should never go to a new program. It means you have to be sharper in how you judge stability.
Some new programs will absolutely thrive. Often because they’re anchored by a stable department with deep roots and a chair who fights for education. Others will limp along on the edge of accreditation trouble, with residents caught in the middle.
You don’t want to guess which is which. You want to know.
FAQ
1. Is it a bad idea to rank a brand new program highly?
Not automatically. I’ve seen new programs become phenomenal training sites within five years. What makes it a bad idea is going in blind. If leadership is stable, the department has a long-standing reputation, and faculty seem committed with actual protected time, a new program can be a fast-track to leadership and opportunity. If you detect high churn, vague answers, and thin faculty depth, ranking them high is gambling with your career.
2. How can I tell if a PD is likely to stay?
Ignore the motivational speech and look at their trajectory. If they were recruited from outside specifically to start the program, have prior GME roles, and seem embedded in the institution (committee roles, academic titles, research), they’re more likely to stay at least 3–5 years. If they were a last-minute internal promotion with no clear support, or they hint at “this role being a stepping stone,” assume higher risk. Also, residents will often hint: “We really hope they stay” is very different from “They’re not going anywhere.”
3. What happens to residents if a bunch of faculty leave at once?
Day-to-day, your life gets more chaotic. Rotations get rearranged, electives disappear, continuity suffers. On paper, the program scrambles to recruit replacements, borrow faculty from other departments, or have leadership pick up teaching directly. ACGME may get involved if core faculty numbers drop below requirements. Residents usually still graduate, but the quality of training can dip significantly during the transition period, and your letters and mentorship may suffer.
4. Should I ask directly about faculty turnover on interview day?
Yes, but do it intelligently. With leadership, you might ask, “How has your core faculty group evolved since initial accreditation?” or “What’s your strategy for maintaining faculty stability as the program grows?” With residents, be more blunt: “Have many attendings left since you started? Did that affect your training?” You’re not trying to interrogate; you’re trying to see if the story you hear from leadership matches what residents are actually living.
If you remember nothing else:
- The first three Match cycles of a new program are dominated by faculty churn, whether they admit it or not.
- Your training quality is directly tied to whether that churn stabilizes by year three or becomes chronic.
- You can read a program’s trajectory by tracking who stays, who leaves, and how honestly they talk about it.















