
You are PGY‑1 in July. You matched into a brand‑new residency. The ink is still drying on the ACGME letter. Your badge works on only half the doors. Nobody knows where your workroom is. The EMR order sets for your service literally do not exist yet.
You keep hearing two things:
- “You’ll have so much opportunity to shape the program.”
- “You’re the guinea pigs.”
Both are true. How that plays out depends heavily on the age of the program.
Let me walk you through what changes from Year 0 to Year 3 of a new residency—and what you should actually be doing, month by month, as the program matures.
Big Picture: How Program Age Shapes Your Training
Before the timeline, you need a mental model.
New residencies go through three rough phases:
| Program Year | Stage Name | Main Resident Experience |
|---|---|---|
| Year 0 | Build-and-Fix | Chaos, access, influence |
| Year 1–2 | Cementing | Structure, growing pains |
| Year 3+ | Stabilizing | Consistency, less flexibility |
By Year 3, your day-to-day looks very different from that chaotic first July. Same hospital. Same name. Completely different trainee experience.
And you do not experience this in the abstract timeline of the program. You experience it as your PGY year + program age. A PGY‑1 in Program Year 0 has a very different life from a PGY‑1 in Program Year 3.
So I am going to anchor this to program age and then layer in what you should be doing at each stage.
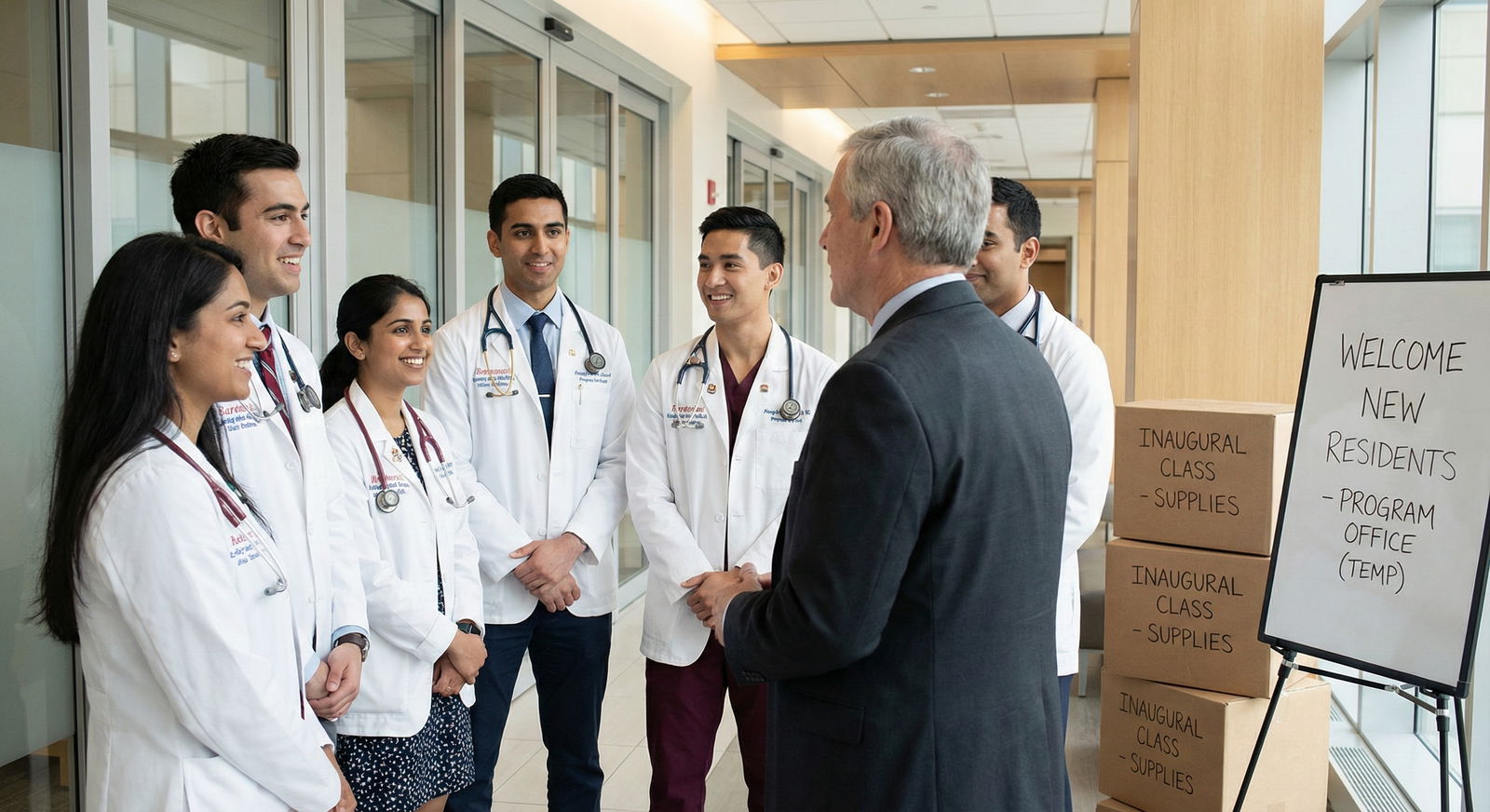
Program Year 0: The “We Just Opened” Phase
Assume Year 0 starts with the first residents ever. No upper levels. No alumni. The program director still says “when we get accredited” even though you already are.
Months 0–3: Survival and Infrastructure
At this point you should expect:
No institutional muscle memory
- Nurses, consultants, even attendings ask, “We have residents now?”
- Paging trees are wrong. Call schedules are improvised.
Curriculum gaps
- Conferences being built week-by-week.
- No established board-review schedule.
- Half the didactics are recycled from med student lectures.
Service design in flux
- Caps unclear.
- Workflows differ by attending: one wants notes in by 10:00, another by 13:00.
- Rotation goals often unspoken or generic.
What you should actively do in Months 0–3:
Document everything that breaks Keep a running log (shared doc, not a group text that evaporates):
- Tasks you are doing that feel like scut / not educational.
- Recurrent bottlenecks (e.g., imaging delays, consults ignoring you).
- Times you cannot meet duty hours because of predictable issues.
At this point you should:
- Tag items by severity: “unsafe,” “unsustainable,” “annoying.”
- Bring 2–3 high-yield issues to your chief or PD every month, not 20 scattered complaints.
Clarify expectations ruthlessly Ask each attending on each rotation:
- “What does a successful intern look like on this service?”
- “What decisions do you expect me to make independently by the end of the month?”
- “How do you like to run rounds?” (find this out on Day 1, hour 1)
Year 0 programs do a terrible job of articulating this. You have to force the issue.
Protect your base
- Learn the EMR deeply. Being the person who can actually find prior notes or pull meaningful trends buys you goodwill while the rest of the program flails.
- Nail simple tasks: timely notes, clean sign-outs, following up results. Boring, but in Year 0 chaos, reliability stands out.

| Category | Value |
|---|---|
| Clinical Work | 45 |
| Fixing Systems | 20 |
| Curriculum Building | 15 |
| Random Firefighting | 20 |
Months 4–6: Emerging Patterns, First Corrections
By now:
- Call patterns have repeated.
- The program has had its first minor crisis (duty hour issue, near-miss, a rotation meltdown).
- Faculty are starting to see where residents actually fit.
At this point you should:
Push for very specific schedule changes Not vague “work-life balance” talk. Concrete asks like:
- “Night float should be 5+2 instead of 7 in a row due to X.”
- “We need a protected sign-out block from 16:30–17:00.”
Year 0 is the easiest time to change structure. Once a call schedule survives one year, it calcifies.
Start defining your program’s “identity” Decide, collectively:
- Are you going to be procedure-heavy?
- Strong on QI and systems?
- Very resident-driven with early autonomy?
If you do not define this, hospital admin and random legacy culture will do it for you. Badly.
Build simple, repeatable tools
- Standard admit H&P templates.
- Standard sign-out format for your program.
- Basic checklists for common rotations (ICU, wards, ED).
Think: “What can a new intern do correctly on Day 2 with a one-page guide?”
Months 7–12: The “Prototype Version 1.0” Year Ends
By the end of Year 0, several things are true:
- The ACGME site visit or follow-up is either done or looming.
- Faculty are less confused by your existence.
- Word about your program is circulating among med students.
At this point you should:
Shape the narrative Med students will ask you, “How is it there?” Your honest-but-strategic answer matters.
Avoid:
- “It’s chaos, do not come here” (even if you feel that). That poisons your own future reputation. Use:
- “We’re new, so some systems are still being built, but I get a ton of hands-on experience with X and Y. If you want structure handed to you, this may not be your best fit.”
Start compiling a real resident handbook Not the generic PDF HR gave you. The real one:
- Who actually answers pages on each service.
- Hidden workflows (how to get an urgent MRI after hours, who really controls beds).
- “If you’re on call and X happens, do Y, not Z.”
Push for protected education that actually stays protected Before Year 1 begins, you want:
- A weekly didactic block with coverage plans.
- Clear rules: when can you be pulled out, by whom, and for what level of emergency.
If this is not nailed down by the start of Year 1, it will never truly be protected.
Program Year 1: From Chaotic Startup to Early System
Now residents have been there one year. Maybe two classes exist (PGY‑1 and PGY‑2). The program is no longer “brand new,” but it is still very much in beta.

| Period | Event |
|---|---|
| Year 0 - Build basic schedules | Start |
| Year 0 - Identify failures | Month 3 |
| Year 0 - First major revisions | Month 9 |
| Year 1 - Add second class | Start |
| Year 1 - Formalize curriculum | Month 6 |
| Year 1 - First recruitment cycle review | Month 12 |
| Year 2 - Add senior class | Start |
| Year 2 - Solidify call structure | Month 6 |
| Year 2 - Prepare for first graduates | Month 12 |
| Year 3 - Graduate first class | Start |
| Year 3 - Stabilize identity | Month 6 |
| Year 3 - Enter steady-state operations | Month 12 |
Months 0–3 (of Year 1): The First Real Hierarchy
Suddenly:
- There are now “upper levels” (PGY‑2s) but they only have one year more experience than the interns.
- Systems you helped design last year are being used by people who never saw how bad it was before.
At this point you should:
Standardize teaching expectations If you are a PGY‑2:
- Set norms for sign-out teaching, on-call supervision, and procedure supervision.
- Explicitly decide: “Interns place all non-ICU lines with supervision” or “Only seniors place central lines.”
If you do not set these expectations, each attending will impose their own, and interns get whiplash.
Create simple evaluation tools that match reality For each key rotation, define:
- 3–5 concrete skills an intern / junior must demonstrate.
- Rough milestones: by Week 2 of wards, an intern should independently manage X; by end, Y and Z.
Then push the PD to align official evaluation forms to those actual skills.
Guard against “senior creep” New PGY‑2s will be tempted to do everything themselves because:
- They remember Year 0 chaos.
- It feels faster and safer.
That destroys intern autonomy. At this point you should be consciously asking:
- “What can I safely hand down?”
- “What must I do myself?”
Months 4–8: Cementing Routine, Fixing Overcorrections
By mid–Year 1, the pendulum often swings:
- From “no rules” to “too many rules.”
- From total chaos to rigid structure that does not flex by service volume or patient complexity.
At this point you should:
Audit your own schedules Once or twice in this window:
- Pull 4–6 weeks of schedules for each PGY level.
- Check duty hours, clinic conflicts, call fairness, ICU/ward/ED exposure balance.
You are looking for:
- Quiet but toxic inequities (one resident stuck on nights constantly).
- Accidental gaps (no one gets meaningful outpatient time).
Separate loud complaints from real problems There will be noise. A lot of it. Your job as a maturing cohort is to:
- Elevate issues that affect safety, education, or fairness.
- Down-prioritize stuff that is just preference (start time 06:15 vs 06:30).
Refine conferences from “topics” to “curriculum” Early on, conferences are random:
- “Someone talk about pneumonia?”
- “Who can cover sepsis bundle this week?”
By now, at this point you should:
- Lay out a 12-month curriculum map.
- Assign blocks (e.g., Cardiology month: CHF, ACS, arrhythmias, valvular disease).
- Ensure every PGY level hits required content at least twice in 3 years.

| Category | Value |
|---|---|
| Year 0 | 20 |
| Year 1 | 50 |
| Year 2 | 75 |
| Year 3 | 90 |
(Values = rough “percent of topics with structured curriculum,” not perfection, but you get the idea.)
Months 9–12: First Full Feedback Loop
By the end of Program Year 1:
- You have gone through at least one full recruitment cycle.
- Med students are rotating with you based on your first year’s reputation.
- Hospital leadership is expecting “mature” performance.
At this point you should:
Review recruitment versus reality Ask yourselves:
- What did we sell on interview day?
- Did the actual intern year match that pitch?
- Where did we overpromise?
Then either:
- Fix the gap, or
- Change the pitch.
Lock in what is working—on paper Anything that has worked well two cycles in a row:
- Build it into policy.
- Put it in the handbook and orientation material.
- Make it the default, not the exception.
Decide where you want to be differentiated by Year 3 You have maybe 18 months before your first grads walk out. This is when you decide:
- “We are the community-heavy, high-volume, procedure-competent program,” or
- “We are research/QI focused with strong academic mentorship,” etc.
Then align electives, scholarly time, and faculty hiring to that.
Program Year 2: First Seniors, Real Culture
Now there are three classes. Seniors exist. “We’ve always done it this way” starts to appear, which is both good and dangerous.
Months 0–4: Establishing Senior Standards
PGY‑3s (or PGY‑4s, depending on specialty) are now:
- Running codes.
- Leading rounds.
- Covering multiple services at night.
At this point you should:
Define what “graduation-ready” looks like As a senior, ask:
- “If I was attending tomorrow at this hospital, what would I need to feel safe?”
Then check:
- Are you getting enough independent decision-making?
- Have you managed the common critical scenarios without attending immediately at your elbow?
Codify handoff from senior to intern level Set explicit:
- What decisions must involve the senior.
- What intern decisions are presumed unless overruled.
- Escalation chains for conflict with consultants, nursing, or administration.
Harden call and backup systems Year 2 is where you fix:
- Who covers if someone is out sick.
- What qualifies as “sick enough” to call out.
- How backup call is compensated or credited.
If this is loose, burnout skyrockets.
Months 5–8: QI, Research, and External Presence
Now that the basic clinical machine runs, you should start looking outward.
At this point you should:
Build a QI pipeline Take those Year 0 and Year 1 “annoying problems” lists and:
- Identify 3–5 that can become formal QI or patient safety projects.
- Pair residents with faculty to turn them into posters, abstracts, or local talks.
Start showing up at regional/national meetings Even one or two projects presented at:
- Society of Hospital Medicine
- ACEP, CHEST, ACOG, etc.
changes your program’s external identity from “new and unknown” to “upcoming.”
Mentor the juniors on how to use the program’s youth Explicitly teach:
- Where they can bend rules to improve care.
- How to propose changes.
- When to shut up and just get the work done because the hospital is not ready to change yet.
Months 9–12: Preparing for First Graduates
You are now on the edge of Program Year 3 reality: graduates.
At this point you should:
Track actual outcomes For the first graduating class:
- Fellowship match results.
- Job offers (type of practice, geography).
- Board pass rates (if available later, but prep starts now).
Cross-check outcomes with original goals If the stated goal was:
- “Produce community-ready generalists,” but everyone is scrambling to get fellowships they did not match into, your messaging and training are misaligned. Or:
- “Strong fellowship placement,” but your research infrastructure is thin. Fix that now for cohorts behind them.
Create alumni feedback loops Plan now:
- How you will survey grads 6–12 months out.
- What you will ask: “What were you underprepared for?” is the key question.
Program Year 3: Stabilization and the Tradeoff
By Year 3, you are losing the “new program” label in people’s minds. That is good for reputation and bad for flexibility.
Months 0–6: First Graduation, Real Identity
Graduates walk across a small ceremony in the auditorium. Suddenly:
- You have alumni in practice or fellowship.
- Applicants can ask, “Where do your grads go?” and you have real answers.
- ACGME is looking for outcome data.
At this point you should:
Use alumni stories strategically For current residents:
- Debrief with alumni about what was missing.
- Add those missing experiences to senior rotations or electives.
For recruitment:
- Highlight strong matches and jobs.
- Be honest about where you are still building.
Lock in non-negotiables Decide:
- Which aspects of training are now “this is who we are,” not up for annual debate.
Examples:- Every PGY‑2 gets at least 2 dedicated ICU months.
- Dedicated weekly simulation that never gets cancelled.
You cannot re-argue foundational structure every year and stay sane.
- Which aspects of training are now “this is who we are,” not up for annual debate.
Clean up legacy workarounds In young programs, residents invent workarounds:
- Shadow paging lists.
- Side spreadsheets tracking patients because EMR is bad.
- Unofficial rules for when to involve certain attendings.
By Year 3, at this point you should:
- Either formalize these into official workflows, or
- Eliminate them and build proper systems.
Months 7–12: Entering Steady State (and Guarding Against Stagnation)
The program is no longer “fragile.” Now the risk is different: stagnation and complacency.

| Category | Value |
|---|---|
| Year 0 | 90 |
| Year 1 | 65 |
| Year 2 | 45 |
| Year 3 | 30 |
(Flexibility: high in Year 0, declines as structure improves.)
At this point you should:
Institutionalize resident leadership Not just a “chief resident” doing schedules. Real roles:
- Director of Resident QI.
- Resident Curriculum Committee chair.
- Wellness and culture leads with actual authority and budget.
Implement a 2-year rolling review cycle Instead of re-litigating everything every year:
- Odd years: Review curriculum and rotations.
- Even years: Review call schedule and duty hour structure.
Or some equivalent cadence. Point is: structured, predictable change, not constant churn.
Keep a small “experimental zone” Reserve:
- One elective block per year for “experimental rotations.”
- One conference per month for resident-led innovations.
This keeps some of that Year 0 energy alive, without reintroducing Year 0 chaos.

What This Means For You, Personally
All that program-level talk is only useful if it guides what you do at different program ages.
If you are an intern in Program Years 0–1:
- Focus on:
- Clinical competence.
- Documenting problems.
- Being one of the “builders,” not just a complainer.
- At this point you should say “yes” to:
- Sitting on curriculum or QI committees.
- Helping create orientation materials.
If you are a mid-level (PGY‑2/3) in Years 1–2:
- Focus on:
- Standardizing expectations.
- Mentoring without smothering.
- Turning recurring frustrations into QI projects or structural fixes.
If you are a senior in Years 2–3:
- Focus on:
- Ensuring graduation readiness—for yourself and those below you.
- Shaping program identity for the next decade, not just surviving your year.
- Leaving behind clear systems instead of undocumented hacks.
Three Things To Walk Away With
Program age changes everything. Year 0 is chaos and leverage. Year 3 is stability and less flexibility. Use the phase you are in instead of fighting it.
Your cohort sets the culture. The first 2–3 classes decide what “normal” looks like. Future residents will inherit your defaults—good or bad.
Think like a builder, not a passenger. Log problems, propose solutions, pilot small changes, then lock in what works. That is how a new residency becomes a good residency.















