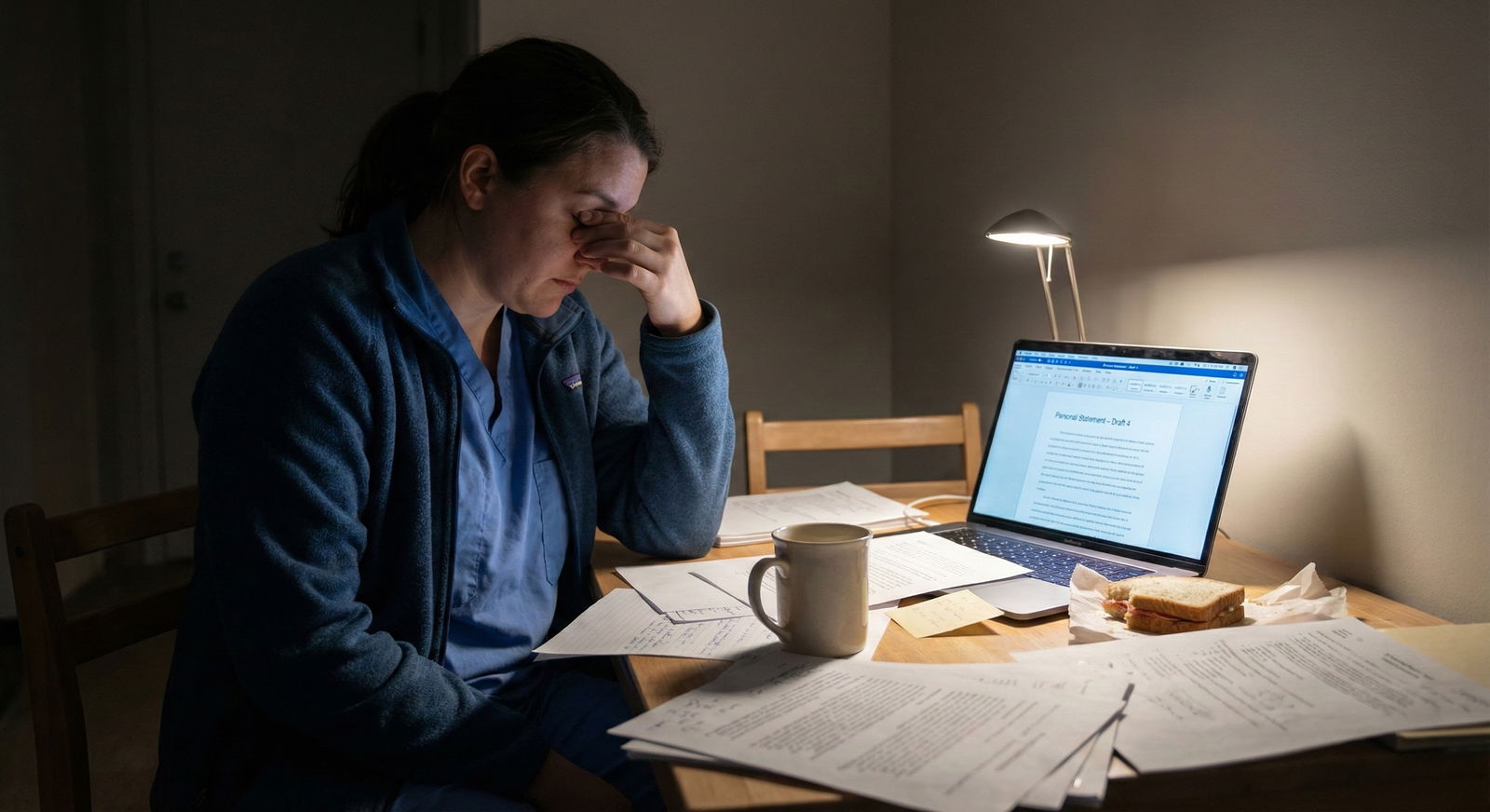
Most people either say way too much about their mental health in their personal statement… or panic and say nothing at all.
You’re probably terrified of both.
If you’re anything like me, your brain is bouncing between:
“If I’m honest, they’ll blacklist me” and “If I hide it, my story makes no sense and I sound fake.”
And then there’s the worst‑case spiral:
What if they think I’m unstable?
What if this goes into some permanent file?
What if one sentence ruins my entire career?
Let’s talk about all of that. Really plainly. No sugarcoating.
The uncomfortable truth: yes, they are judging your mental health
Not just if you disclose it. Always.
They’re reading your personal statement asking:
- Can this person handle residency hours without falling apart?
- Are they going to be safe with patients?
- Are they likely to burn out, quit, or need extended leave?
- Are they emotionally stable enough for this specialty?
The part no one tells you: they’re inferring this even if you never mention mental health. From your tone, your narrative, how you talk about setbacks, everything.
So the question isn’t “Should I let them evaluate my mental health?”
They already are.
The real question is:
Do you want to guide that narrative with careful, strategic honesty… or leave them guessing and possibly imagining something worse?
Sometimes it helps you to address it. Sometimes it hurts you. And sometimes, the best move is a vague, 1–2 line reference and then move on.
The 3 big mental health disclosure scenarios
Let me be very blunt. Most applicants I see fall into one of these buckets:
1. Your mental health is central to your story
Examples:
- A major depressive episode that led to a leave of absence
- A hospitalization (psych) during med school
- A serious suicide attempt in your past
- A diagnosed condition (bipolar, OCD, PTSD, eating disorder, severe anxiety) that clearly impacted your academic timeline, exam attempts, or leaves
If this is you, you’re probably thinking:
“If I don’t say anything, they’ll just see red flags and assume I’m worse than I am.”
You might be right.
But this is the landmine zone. If you do decide to address it in your residency personal statement, you need to:
- Avoid graphic detail
- Avoid sounding currently unstable
- Show concrete treatment, stability, and insight
- Tie it directly to growth or current strengths
Not vague “I’m stronger now” fluff. I mean: what systems, treatments, supports, changes actually exist?
2. Your mental health mattered to you, but didn’t disrupt your record
Examples:
- Ongoing therapy for anxiety or trauma, but no LOA, no big academic dip
- Mild–moderate depression you managed while functioning well
- Burnout that didn’t lead to formal accommodations
- Longstanding ADHD that you’ve had since before med school, managed with treatment
This is the gray zone where many people overshare.
You feel like “mental health is a huge part of who I am,” so you want to write an essay about it. The risk: it can raise concerns the committee didn’t even have.
If your file doesn’t show obvious red flags tied to mental health, you usually don’t need to go into diagnostic-level detail in the PS.
You can:
- Talk about empathy for patients with mental illness
- Mention personal or family experiences lightly
- Focus on what you learned rather than listing your own conditions
3. You’re tempted to use your mental health as “trauma fuel” for a powerful story
This is harsh, but I’ve seen it a lot.
You think:
“My scores are average. I need a gripping story so I stand out. Maybe I should write about my suicide attempt / panic attacks / self-harm / hospitalization in detail.”
Programs are not reality TV. They’re risk‑averse institutions. A highly dramatic, recent, or graphic mental health narrative absolutely can backfire.
Not because your story isn’t valid. But because from their chair, they’re thinking:
“Will this person safely handle night float with three crashing patients and zero sleep?”
If the mental health narrative is mostly there for “impact,” and not because it explains a clear part of your record, I’d strongly reconsider including it.
What programs really worry about (the part they’ll never say out loud)
Here’s the ugly internal monologue some PDs and faculty have. I’ve heard versions of this in real life:
- “Will they be reliable on call?”
- “Am I going to be dealing with constant crises or leaves?”
- “Is there a risk of self-harm in a high‑stress environment?”
- “Are we putting patients at risk if this person decompensates?”
- “Do they understand their limits and have supports in place?”
They are not supposed to discriminate against mental illness. In practice, they’re absolutely screening for functional risk.
Your personal statement, if it mentions mental health, needs to answer their secret questions without you ever writing, “Don’t worry, I’ll be fine.”
How much detail is “too personal”?
Let’s make this less abstract.
| Level of Detail | Example Snippet |
|---|---|
| Safe, high-level | 'I took a brief medical leave, got treatment, and returned with stronger coping skills.' |
| Moderate, cautious | 'During my second year I experienced depression, worked closely with a therapist, and adjusted my routines.' |
| Risky | 'I was hospitalized for suicidal ideation and still struggle some days, but I’m trying hard.' |
| Very risky / avoid | Graphic detail of self-harm, suicide attempts, or ongoing unstable symptoms |
Think in terms of:
- Time – How long ago was the worst of it?
- Stability – Are you clearly stable now with a track record to prove it?
- Function – Are you meeting responsibilities consistently?
- Specifics – More specifics about coping and support, fewer specifics about symptoms and crises
You want to zoom out on the crisis and zoom in on the recovery and structure.
When you probably should address it (and how to do it without sinking yourself)
If any of these are true, silence can hurt you more:
- You took a medical/LOA in med school
- You repeated a year, failed Step/Level multiple times, or had a long unexplained gap
- Your dean’s letter/MSPE will explicitly reference mental health or “personal difficulties”
- You switched schools or had big transcript disruptions
Because if you don’t give context, committees will invent their own.

| Category | Value |
|---|---|
| Leave of Absence | 35 |
| Failed Boards | 25 |
| Major Grade Drop | 15 |
| Gap Year Explanation | 15 |
| Family-Related Mental Health Context | 10 |
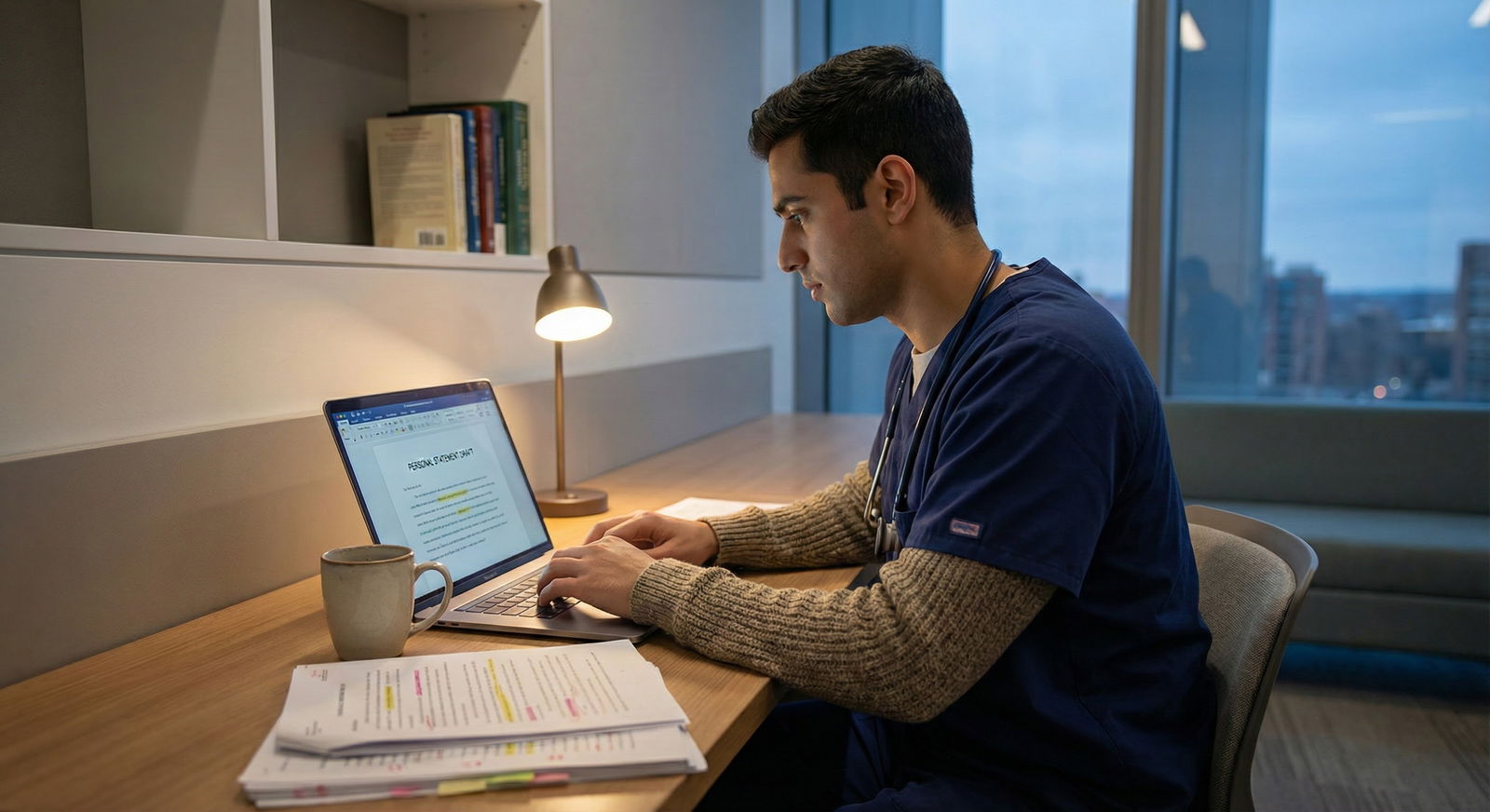
A safer structure to talk about mental health
Here’s a way to organize it that doesn’t read like a confession:
Briefly name the disruption, not the drama.
“During my second year, I took a medical leave related to my mental health.”Immediately shift to action and support.
“I established care with a psychiatrist and therapist, adjusted my workload, and developed concrete routines for sleep, exercise, and boundaries.”Show outcome with evidence, not adjectives.
“Since returning, I’ve passed all subsequent exams on the first attempt, taken on a research project, and maintained strong clinical evaluations.”Connect to who you are as a physician now.
“This experience made me more attuned to my patients’ invisible struggles and deliberate about modeling sustainable practice.”
Notice what’s missing:
No diagnosis labels required. No graphic moments. No asking for sympathy.
You’re not writing a therapy note. You’re writing a professional narrative that happens to include mental health.
When you probably should not go deep in the PS
These are tough to hear:
- Your mental health crisis was very recent (past 6–12 months) and your record doesn’t yet show sustained stability
- You have no concrete supports or treatment in place (no consistent therapy, no meds if indicated, no systems)
- You’re still actively in the thick of it, with frequent crises, self-harm, or major functional impairment
I’m not saying “you shouldn’t apply.” I’m saying: this may not be material you want to showcase in your main personal statement.
If you’re currently very unstable, the most protective move might actually be:
- To delay your application by a year
or - To keep the PS focused on other aspects and, if absolutely necessary, use another part of the application (or a trusted advisor) to explain essentials
Programs don’t want to be your first real stress test.
Concrete examples: what this can look like on the page
These are sample vibes, not copy‑paste lines. Don’t clone them. But use them to calibrate what “personal but not unsafe” feels like.
Example 1: Leave of absence for depression
Weak (too raw, too risky):
In MS2, I became severely depressed and suicidal. I could barely get out of bed and started self-harming. After failing multiple exams, I had to take time off. I still struggle, but I’m hoping residency will give me purpose and help me feel better.
Why this scares programs:
You sound like you’re still in crisis and looking for residency to save you. That’s a no.
Stronger:
During my second year of medical school, I took a medical leave related to depression. With the support of my school, psychiatrist, and therapist, I learned to address my health proactively instead of waiting until I was overwhelmed. I returned to complete my preclinical coursework, passed Step 1 on my first attempt, and have since received strong clinical evaluations. That experience changed how I approach both my own limits and my patients’ struggles with mental illness.
This version says:
There was a problem. I got help. I stabilized. Here’s proof. Here’s what it means now.
Example 2: General anxiety / longstanding therapy
Weak (oversharing and unnecessary):
I’ve dealt with anxiety since childhood and have tried several medications and therapists. I still have frequent panic attacks, but I’m learning to push through. My anxiety makes me overthink every patient interaction, but maybe that’s a good thing.
This basically screams: ongoing impairment, unstable.
Stronger:
Throughout training, I’ve worked with a therapist to develop sustainable coping skills for stress and self-doubt. That ongoing work has made me more intentional about how I show up for patients and colleagues, especially on busy services. It’s also helped me recognize signs of burnout early and address them before they affect my performance.
You don’t need the diagnosis name for this level of discussion. The focus is on functioning and growth.
What about using family mental health or trauma?
Sometimes the question is: “Can I talk about my parent’s bipolar disorder? My sibling’s suicide? My partner’s addiction?”
Yes, but with the same rules:
- Don’t go into graphic detail.
- Don’t make it the only thing you talk about.
- Make sure it actually connects to your path into medicine or your specialty.
- Don’t sound like you’re still actively drowning in it.
For example:
Growing up with a parent who cycled through untreated bipolar episodes taught me how invisible suffering can be, even to those closest to you. That early exposure shapes how seriously I take mood symptoms in my patients and how carefully I listen when a family member says, “Something’s just not right.”
Reasonable. Controlled. Relevant. Not trauma‑dumping.
Okay, but I’m still terrified: will this secretly blacklist me?
Here’s the worst‑case voice in my own head:
“One sentence about depression, and boom, every PD in the country puts a red X next to my name.”
Reality is more nuanced.

| Category | Value |
|---|---|
| Ongoing severe impairment | 90 |
| Lack of treatment/support | 80 |
| Recent instability | 75 |
| Unexplained gaps with no context | 60 |
| Well-managed, past episode | 20 |
What really spikes concern:
- Evidence you’re still quite unstable
- Drama without resolution
- No clear treatment/support or insight
- Recent crisis with no time‑tested stability afterward
What usually doesn’t blacklist you:
- A past episode you’ve clearly treated and grown from
- A well‑explained LOA with strong performance afterward
- Mention of therapy or past struggles framed as part of your development
Can some programs quietly hold it against you anyway? Yes. Some will. I’m not going to lie.
But others will see it as emotional maturity and resilience. In psych, peds, FM, IM, especially—the right framing can actually be a net positive.
The job is to maximize the chance that the right programs see the best version of you, and minimize unnecessary red flags.
Strategic alternatives: you don’t have to cram everything into the PS
Your personal statement isn’t the only place to address mental health–related issues.
You can also consider:
- MSPE / Dean’s letter (they may already allude to it)
- A brief note in ERAS “additional info” or experiences section
- A conversation with a trusted advisor who can advocate for you
- Rarely, a very short explanation in a program‑specific communication if invited

| Step | Description |
|---|---|
| Step 1 | Do you have a clear red flag? |
| Step 2 | Needs some explanation |
| Step 3 | Optional to mention |
| Step 4 | Brief, structured mention in PS |
| Step 5 | Use MSPE/Advisor/Other section |
| Step 6 | Focus PS on strengths |
| Step 7 | Is PS the best place? |
You’re allowed to be selective. You don’t owe every reader your entire psychiatric history.
Practical checklist: should I mention my mental health in my personal statement?
If your anxiety is screaming at you, run through this honestly:
- Is there a major, visible disruption in my record that mental health actually explains?
- If I say nothing, will programs be confused or assume something worse (e.g., professionalism violation, substance issue)?
- Can I describe this briefly, without graphic detail, and with clear evidence of stability since?
- Do I have at least 6–12 months of consistent functioning (academically/clinically) since the worst of it?
- Can I connect this to who I am as a physician now, not just as a victim of circumstances?
If you get mostly “yes” to 2–5, a brief, carefully controlled mention is often reasonable.
If you’re hitting “no” on 3–4, I’d be extremely cautious about centering it in your PS.
What you can do today (so this doesn’t stay a vague cloud of panic)
You don’t have to fix the whole essay right now. Do this one specific thing:
Open your personal statement draft and underline every sentence about mental health. Then, for each one, write in the margin: “Crisis, Treatment, Stability, or Growth.”
If more than half your mental health content is “crisis,” start cutting and shifting toward “treatment, stability, growth.”
That one exercise will immediately show you if your statement reassures programs… or quietly terrifies them.
FAQ (4 questions)
1. Should I actually name my diagnosis (e.g., “bipolar disorder,” “PTSD”) or keep it vague?
You usually don’t need the label. Saying “I took a medical leave related to my mental health” is often enough. Diagnosis names can trigger snap judgments you don’t control. The only time I’d consider naming it is if:
- it’s already in official documents, and
- you can show a long, clear period of stability with strong performance, and
- an advisor who knows your full situation agrees it’s safe.
Default: keep it general and focus on actions, support, and outcomes.
2. Will programs ask about my mental health in interviews if I mention it in my PS?
Some will. Some won’t. If you bring it up in writing, you must be prepared to talk about it calmly and consistently in person. That means having a 1–2 sentence, non‑defensive script ready, focusing on: what happened in broad terms, what you did to address it, and how you’ve functioned since. If even imagining that question makes you panic or tear up, your story may still be too raw to center in your application.
3. What if my mental health is fine now but my Step score or grades took a hit in the past?
You can link them briefly without over‑explaining: “During that period I was struggling with unrecognized depression, which affected my performance. After starting treatment and adjusting my routines, my subsequent scores and evaluations better reflect my abilities.” Then you must let your later performance carry the weight. One sentence of explanation, then concrete evidence of improvement. Don’t spend three paragraphs defending one bad score.
4. I feel like hiding everything is dishonest, but being honest feels dangerous. What do I do?
This is the core tension. You don’t owe full disclosure of every painful detail to strangers deciding where you train. You owe them an accurate picture of your professional readiness. That’s different. You can be truthful without being fully transparent. If there’s a major event that clearly affects your record, mention it briefly, focus on recovery and function, and save the emotional details for your therapist and close people, not your personal statement. If you’re still torn, run your draft by someone who’s sat on a residency selection committee and actually seen how these things land.



















