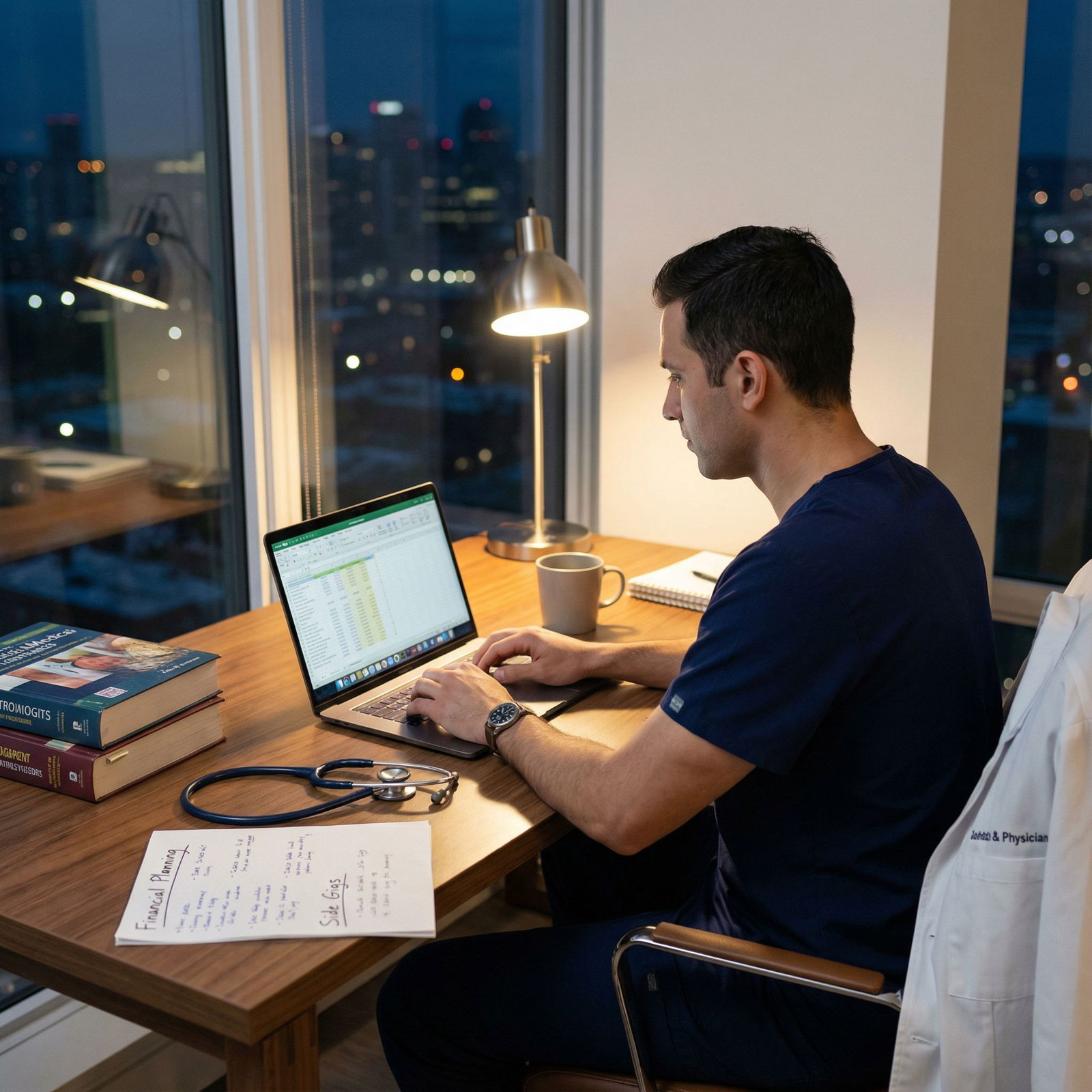
It is 8:45 p.m. You just finished a brutal 11‑hour clinic day. Your EMR inbox is still overflowing, but your brain is fried. You sit down with a cup of tea, open your laptop at the kitchen table, and instead of logging back into Epic, you open a neatly organized PDF set of records for a single case. No patients. No prior auths. No Press Ganey scores. Just one focused med‑legal chart review that will pay you more than your entire afternoon clinic.
This is not fantasy. It is what a properly structured med‑legal chart review micro‑practice looks like when you do it right.
Let me break this down specifically.
1. What “Med-Legal Chart Review” Actually Is (And What It Is Not)
Most physicians lump anything involving lawyers into “expert witness work.” That is sloppy thinking and it will cost you opportunities.
There are three distinct buckets:
Pure Chart Review / Consulting (No Testimony)
You quietly review records and provide:- Written memos to counsel
- Chronologies / timelines
- Standard of care assessments
- Causation / damages opinions (for their eyes only)
You may never be disclosed as an expert. You might not even appear by name in any filing. This can be 100% home‑based and asynchronous.
Disclosed Expert Witness Work (With Possible Testimony)
You:- Write formal expert reports
- Have your CV disclosed
- Get deposed or testify at trial
This is higher profile, higher risk, higher pay, and more time‑sensitive.
Hybrid Roles (Consult first, convert later)
You start as a behind‑the‑scenes consultant. If the case is strong, the attorney may ask to designate you as an expert.
For a home‑based micro‑niche “side hustle” that coexists with a clinical job, bucket #1 is your starting point. Low visibility, low legal stress, high flexibility.
Core activities in med‑legal chart review:
- Reviewing EMR/PDF records and imaging reports
- Building a timeline of care (especially important in malpractice, delay in diagnosis, ED cases)
- Evaluating standard of care vs reality
- Assessing causation and contribution (did this deviation meaningfully cause harm?)
- Evaluating damages and prognosis
- Identifying missing records and key questions
No patient interaction. No physical exam. You are selling your brain and your ability to parse messy documentation into clear, defensible medical reasoning.
2. Why This Works Shockingly Well as a Home Micro-Niche
You can stack this work in the margins of your week and it scales just enough to matter without taking over your life.
Key advantages:
- Location independent – You can do this from home, vacation rental, or your parents’ house over the holidays as long as you have privacy and data security.
- Asynchronous – Almost no real-time demands. You work at 5 a.m. or 10 p.m. if you want.
- High hourly leverage – If you charge properly, you will often see effective rates 3–6× higher than your clinical hourly wage.
- Control over caseload – You say yes or no to each case. No RVU hamster wheel.
- Deep focus, not fragmentation – One case at a time. No EMR inbox whiplash.
- Career optionality – Builds a non-clinical income stream that can expand later into full med‑legal consulting or medico‑legal education.
Flip side—the constraints:
- Work ebbs and flows. Feast and famine if you do not have stable pipelines.
- Lawyers can be variable in sophistication. Some are outstanding; some are chaos.
- You must be comfortable saying “No” on weak or unethical cases. Firmly.
Bottom line: as a micro‑niche side practice, med‑legal chart review hits the sweet spot. It is technical, cognitively interesting, and compatible with a normal attending schedule if you keep boundaries.
3. Where You Actually Fit In the Med-Legal Ecosystem
You are not “helping lawyers sue doctors.” That is a lazy caricature. You are part of a risk‑allocation system built around evidence and standards.
There are 5 main stakeholders you might work with:
Plaintiff attorneys
- Use you to decide whether to take a case.
- Need candid assessment of liability and causation.
- Want to avoid sinking six figures into a loser case.
Defense attorneys / Risk management / Insurers
- Use you to stress‑test their case.
- Want to understand vulnerabilities before trial.
- Value clear explanation of how a jury might perceive the care.
Hospitals / Health systems (internal QA, early case assessment)
- Quiet internal reviews after adverse events.
- May pre‑empt litigation, guide root cause analyses, or settle early.
Disability / Workers’ comp / Personal injury firms
- Less about standard of care, more about causation, impairment, and prognosis.
- Heavy on timeline and functional status.
Government / Regulatory bodies (less common for side hustles)
- Board actions, peer review, quality investigations.
- Usually not something you dabble in part‑time at the beginning.
Your micro‑niche might live entirely inside one of these (e.g., plaintiff med‑mal only) or straddle a few (e.g., ED malpractice + EMTALA + wrongful death).
If you want predictable work and lower drama, defense and internal QA often feel less emotionally heated than plaintiff med‑mal. Plaintiff work has more variability but can be more financially aggressive.
4. Building a Real Micro-Niche: Do Not Be a Generalist
“Internal medicine expert willing to review any case” is not a niche. It is a red flag to good attorneys.
You want to be obviously the right person for a very specific slice of the market.
Examples of strong micro‑niches:
- “Emergency physician focused on sepsis, stroke, MI, and ED triage delays in community hospitals.”
- “OB/GYN with emphasis on shoulder dystocia, fetal monitoring interpretation, and VBAC complications.”
- “Hospitalist with expertise in anticoagulation management, perioperative medicine, and inpatient falls.”
- “Pediatric intensivist with specific experience in non‑accidental trauma and sepsis recognition.”
- “Interventional cardiologist focused on cath lab complications, door‑to‑balloon delays, and PCI appropriateness.”
The market rewards specificity + credibility.
To define your micro‑niche, ask:
- What kinds of cases have you actually seen or managed repeatedly?
- Where do you know the guidelines cold?
- Where do you see recurrent systems failures in your day job?
- What makes attorneys’ eyes light up when you describe your background?
Then write your positioning statement in plain language:
“I help plaintiff and defense attorneys evaluate emergency department standard of care and causation in time‑sensitive conditions such as sepsis, stroke, ACS, and pulmonary embolism, particularly in small community hospitals without in‑house specialists.”
That one sentence governs everything—website copy, LinkedIn profile, which calls you take, how you price, and who you say no to.
5. Money: Pricing, Billing Structures, and What “Good” Looks Like
If you get the pricing wrong, you just created a second underpaid job.
Here is what a rational structure looks like for home‑based chart review.
A. Your Hourly Rate
For U.S. physicians with real clinical experience, $350–$600/hour for med‑legal work is standard. Surgeons, proceduralists, and tertiary‑care subspecialists can be higher, often $500–$800/hour.
Anything under $300/hour for expert med‑legal work is undervaluing yourself unless you are very early and just building a portfolio.
You should have:
- One standard hourly rate for review, calls, and memo writing.
- Optionally, a higher rate for rush work (e.g., <72‑hour turnaround).
B. Retainers and Minimums
Never start work without money in hand. Lawyers expect this.
For micro‑level chart reviews (no formal report, no testimony), a clean structure:
- Initial retainer: $1,500–$3,000 upfront for your first 3–5 hours.
- Minimum billing increment: 0.25 hours (15 minutes).
- Re‑up retainer: When retainer drops below 1 hour of work, you require replenishment.
For busier practices, some physicians move to flat minimums per project:
- “Minimal case review (up to 3 hours): $1,500 flat. Additional time billed hourly.”
Always, always send a simple letter of engagement that spells out rate, deposit, scope, cancellation terms, and what happens if they later want deposition or trial testimony.
C. Where the Time Actually Goes
Attorneys underestimate this constantly. You should not.
Typical time breakdown for a single med‑mal chart review (moderate complexity):

| Category | Value |
|---|---|
| Record review | 40 |
| Timeline building | 25 |
| Memo/report writing | 20 |
| Calls with counsel | 10 |
| Admin & setup | 5 |
That means for a 10‑hour engagement, you may spend:
- 4 hours reading and annotating records
- 2.5 hours assembling the chronology and cross‑checking
- 2 hours writing your memo/summary
- 1 hour on Zoom or calls with counsel
- 0.5 hours on admin (billing, file organization, secure transfer)
Do not be shy about billing for every professional minute spent on the case. You are not an RVU robot. You are a consultant.
6. Setting Up the Home Infrastructure (Without Getting Cute)
You do not need a “firm.” You need a serious, professional, and secure setup that respects HIPAA and attorney–client privilege.
A. Technical Stack (Minimum Viable, Not Fancy)
Hardware
- Reliable laptop or desktop
- Dual monitors (non‑negotiable for large records)
- Encrypted hard drive (BitLocker/FileVault)
- Wired backup drive for encrypted local backups
Software & Tools
- Robust PDF reader/editor (e.g., Adobe Acrobat Pro, Foxit, PDF‑XChange) for bookmarks, annotations, and Bates number navigation
- Spreadsheet or simple tool for timeline (Excel, Numbers, or a light project tool—keep it simple)
- Secure email solution with encryption (or a secure client portal)
- Password manager (1Password, Bitwarden, etc.)
Data Security Basics
- Unique, strong passwords + MFA on email and storage
- No case files on random USB sticks
- No printing charts unless you have a locked storage system and shredder
- Use client’s secure upload portals whenever possible
If your tech setup looks like a college student’s laptop on Starbucks Wi‑Fi, you are not ready.
B. Physical Workspace
- A door that closes. Period. No spouse walking through Zoom calls, no kids behind you during confidential discussions.
- Desk, ergonomic chair, and monitor stands. Case review is stationary; your neck and back will complain.
- Locked file drawer if you ever print anything.
You are selling professional judgment. Your physical environment should not scream “side gig on the couch.”
7. Process: How a Case Flows Through Your Micro-Practice
Attorneys love reliability. They hate chaos. You should have a standard pipeline for every case, even if it is just you.
Here is a clean, lean flow from first email to final invoice:

| Step | Description |
|---|---|
| Step 1 | Inquiry from attorney |
| Step 2 | Conflict check |
| Step 3 | Engagement letter and retainer |
| Step 4 | Secure receipt of records |
| Step 5 | High level scan of case |
| Step 6 | Detailed review and notes |
| Step 7 | Timeline and key issues |
| Step 8 | Written memo or summary |
| Step 9 | Call with counsel |
| Step 10 | Final invoice and close file |
Let me translate that into the real world:
Inquiry – Short call or email. You get:
- Case type (e.g., ED sepsis death)
- Role (plaintiff vs defense)
- Jurisdiction
- Date of events (for recency, standard of care guidelines)
Conflict Check – You make sure you are not:
- Employed by or under contract with defendant institution
- Already consulting on related cases
Engagement + Retainer – You send:
- One‑page agreement
- W‑9 if they request
- Wiring or payment instructions
Work starts only after funds clear.
Records Intake – Via secure portal or encrypted link. You immediately:
- Confirm completeness (ED + inpatient + consults + imaging + labs + EMS + outpatient if relevant)
- Ask for missing pieces before diving in.
High‑Level Scan (0.5–1 hour, billable)
- Orient yourself to patient story, timeframe, outcome
- Decide whether anything about the case makes it inappropriate for you
Deep Review and Timeline
- Systematic record review with annotations
- Build a detailed chronology (dates, times, providers, key decisions)
Memo / Summary
- Typically 3–10 pages
- Clear statements of:
- What happened
- What the “reasonable physician” would be expected to do
- Where you see divergence from standard of care (or not)
- Causation analysis: did the deviation cause harm?
- Case strengths and weaknesses
Call with Counsel
- Walk through your findings
- Clarify legal questions (e.g., specific elements of negligence, foreseeability)
- Discuss whether the case is worth pursuing or how to shore up weaknesses
Closeout
- Final invoice + payment
- Confirm file retention period and destruction policy (often 3–7 years, depending on your preference and any applicable rules)
This systematic flow makes you look less like a moonlighting doc and more like a micro‑consulting practice—which is exactly what you are building.
8. Getting Clients: What Actually Works vs Wasted Motion
This is where most physicians flail. They post a generic LinkedIn update and then declare “there is no demand.” Nonsense.
Here is what works.
A. Anchor Presence: A Simple, Credible Website
One clean 1–2 page site that covers:
- Who you are (training, current clinical role)
- Your specific med‑legal niche
- Services (case screening, chart review, internal QA, standard of care analysis, etc.)
- Pricing philosophy (e.g., “hourly with retainer; no contingency”)
- Contact info and secure intake instructions
You do not need SEO wizardry. You need a URL you can send when an attorney asks “do you have a website?”
B. Platform Profiles that Matter
LinkedIn – Completed, with a headline like:
“Emergency Physician | Med-Legal Chart Review & Standard of Care Consulting | Sepsis, Stroke, MI, ED Triage Delays”Direct expert databases (optional, selective)
Bottom tier is spammy; top tier can be worthwhile. I have seen:- SEAK panel (if you go heavier into expert work)
- Specialty‑specific medico‑legal groups
- Regional bar association expert lists
Treat these as amplifiers, not your primary lead source.
C. Direct Outreach that Does Not Feel Like Spam
The most effective tactic I have seen:
- Identify 10–20 plaintiff and defense firms in your state that regularly handle cases in your niche.
- Send each a short, tailored email along with a one‑page CV.
Something like:
“I am a board‑certified emergency physician practicing at [Hospital Type]. I focus on med‑legal chart review and internal case screening for ED cases involving sepsis, stroke, acute coronary syndromes, and triage delays, especially in community settings.
I handle confidential, behind‑the‑scenes reviews (no testimony required) and provide detailed chronologies and standard of care analyses to help you decide which cases to pursue or defend.
I am available for a brief introductory call if you would like to discuss how I approach early case evaluation.”
You do not attach a 6‑page marketing deck. Keep it lean.
D. Relationships and Repeat Business
Once you deliver on a couple of cases for a firm:
- They will send more if you are:
- On time
- Candid, even when the case is weak
- Clear in your communication
Consistent, high‑quality work for 3–5 firms can fill your micro‑niche pipeline. You do not need 50.
9. Performance: How to Actually Be Good at This
Plenty of smart clinicians are bad med‑legal consultants. They either:
- Write sloppy, emotional screeds.
- Or they equivocate so much the memo is useless.
Your job is not to be the angry doctor or the scared doctor. Your job is to be the clear, dispassionate, precise physician who understands the clinical reality and can articulate it to non‑clinicians.
Core skills you must develop:
Timeline discipline
The heart of any med‑legal case is “who knew what, when, and what did they do with that information.”
Your chronology must be:- Precise with timestamps
- Cross‑linked to source records
- Stripped of fluff
Standard of care articulation
Not guidelines alone. Not perfection. The question is always:
“What would a reasonably prudent physician with similar training do under similar circumstances at the time of care?”You must be able to:
- Cite concrete references (guidelines, literature, usual practice)
- Allow for gray zones and reasonable judgment differences
- Still call out clear departures without flinching
Causation analysis
The single biggest weakness in many physician reviews.
You must answer:
“If the care had met standard, is it more likely than not that the outcome would have been meaningfully different?”Hand‑waving about “might have changed something” is poor work.
Communication for non‑clinicians
Your memo should read cleanly for an intelligent lawyer, not just a cardiologist colleague.- Minimize jargon or define it once.
- Use short, declarative sentences for key points.
- State conclusions explicitly: “In my opinion, Dr. X met the standard of care” or “In my opinion, Dr. X’s failure to [X] fell below the standard of care and was a substantial contributing factor in [outcome].”
You are not writing a board exam essay. You are writing a professional opinion to guide six‑ and seven‑figure decisions.
10. Risk, Ethics, and Staying Out of Trouble
Let me be blunt: most physicians dramatically overestimate the legal risk of med‑legal work and underestimate the ethical risk of doing it sloppily.
Legal / Professional Risk
- Licensing – Usually, you should be licensed in at least one U.S. state, ideally where you actively practice. Case jurisdiction rules are nuanced, but for behind‑the‑scenes review, this is generally sufficient.
- Malpractice / E&O coverage – Many carriers offer “expert witness / consulting” riders. Call and ask. Do not assume you are covered.
- Board issues – There have been rare cases where physicians got in trouble for obviously dishonest or grossly incompetent testimony. If your work is honest, literature‑supported, and within your training and experience, your risk is low.
Ethical Guardrails
Non‑negotiables:
- You do not alter your opinion to fit the side that hired you.
- You turn down cases outside your real expertise, even if they pay well.
- You disclose key limitations (e.g., missing records, conflicting data).
- You do not diagnose parties you have not examined; you stick to record‑based opinions.
If you feel pressured to reach a particular conclusion, that is not a gray area. That is your cue to disengage.
11. Growth Paths: From Side Hustle to Serious Practice (If You Want)
You may want this to remain 5–10 hours per month forever. That is fine. But if you get hooked on this work, here is how it evolves.
Common expansions:
From consulting only → formal expert witness
You start writing full reports and testifying in depositions and trials. Higher pay, more visibility, more schedule disruption, more scrutiny.From solo → micro‑team
You bring in a part‑time RN or paralegal to help with timeline building and record organization while you focus on medical analysis.From single niche → adjacent niches
Example: An ED doc who starts with sepsis and stroke later adds EMTALA, boarding, and ED mental health holds.From case work → education / speaking
CLE talks for lawyers, risk management talks for hospitals, developing internal guideline audits and QA projects.
None of this is required. But it is available if the money, intellectual challenge, and autonomy pull you in.
12. Quick Comparison: Clinical Hour vs Med-Legal Hour
Let me crystallize why this matters financially.
| Feature | Clinical Hour (Outpatient) | Med-Legal Chart Review Hour |
|---|---|---|
| Typical pay | $80–$150 | $350–$600+ |
| Interruptions | Constant | Minimal |
| Control of schedule | Low | High |
| EMR / inbox burden | High | None |
| Documentation style | Billing/compliance driven | Analysis and clarity driven |
| Location | Clinic only | Anywhere private and secure |
This is why even 4–8 well‑priced hours per month changes your financial and psychological landscape. It is not about grinding extra shifts; it is about elevating the value of each non‑clinical hour you choose to work.
FAQ: Med-Legal Chart Review Micro-Practice
1. How many years of clinical experience do I need before doing med‑legal chart reviews?
I recommend at least 3–5 years of independent attending practice in the niche you want to review. Fresh grads can technically do it, but your credibility and pattern recognition are weaker. You want enough real‑world exposure to know what is “usual,” what is “borderline,” and what is “outrageous.”
2. Can I do this if I am an employed physician with a non‑compete or outside work policy?
Often yes, but you must check your contract. Many employed positions require disclosure of “outside professional activities” and may restrict expert witness work involving your own institution. I have seen contracts that totally forbid medico‑legal work and others that allow it with prior written consent. Get clarity in writing before you start.
3. Do I have to appear in court if I only want to do behind‑the‑scenes review?
Not if you structure your practice that way. In your engagement letter, specify that your role is limited to consulting and internal case evaluation, not formal expert designation or testimony. If a client later wants to designate you, you can negotiate a separate agreement and decide on a case‑by‑case basis whether you are willing.
4. How do I handle cases where my opinion is bad news for the hiring attorney?
You tell them the truth, quickly and clearly. Many of the best plaintiff lawyers I know are grateful for early, candid “this is a weak case; do not file it” feedback. It saves them money and time. Your reputation rests on being unflinchingly honest, not on generating favorable opinions. If they regularly pressure you to change your views, drop the client.
5. What if I am asked about my med‑legal work during a credentialing or malpractice suit I am personally involved in?
You list it honestly, but you do not volunteer case details protected by privilege or confidentiality. Having med‑legal experience is not a negative; in some contexts, it is a strength. But assume anything you write could be scrutinized for internal consistency with your clinical practice. That is another reason to keep your opinions careful, evidence‑based, and within your expertise.
6. How many hours per month can I realistically do without burning out on top of a full‑time job?
For most full‑time clinicians, 5–15 hours per month is the realistic sweet spot. That might be 1–3 modest cases. Beyond 20 hours per month, you are essentially adding a part‑time job and will feel it. Start with a single case, see how it fits around your existing schedule, then slowly expand until you feel the strain and back off 20–30%.
You are standing at an inflection point in your career where “more shifts” is not a sustainable answer, but you are not ready to walk away from medicine altogether. A focused med‑legal chart review micro‑practice gives you a controlled, high‑leverage way to monetize what you already know—without another fellowship or another degree.
Get your niche clear. Set your rates like a consultant, not a resident. Build a simple, secure home infrastructure. Then take one well‑chosen case and do meticulous work.
Once you see what a well‑paid, interruption‑free two‑hour review session feels like compared with your average clinic block, you will understand exactly why so many physicians quietly build this into the next phase of their careers. What you do with that leverage—cut back clinical time, pay off debt faster, or design a semi‑retired future—is the next chapter.


















