Can I Negotiate Call or Weekend Adjustments to Protect Against Burnout?
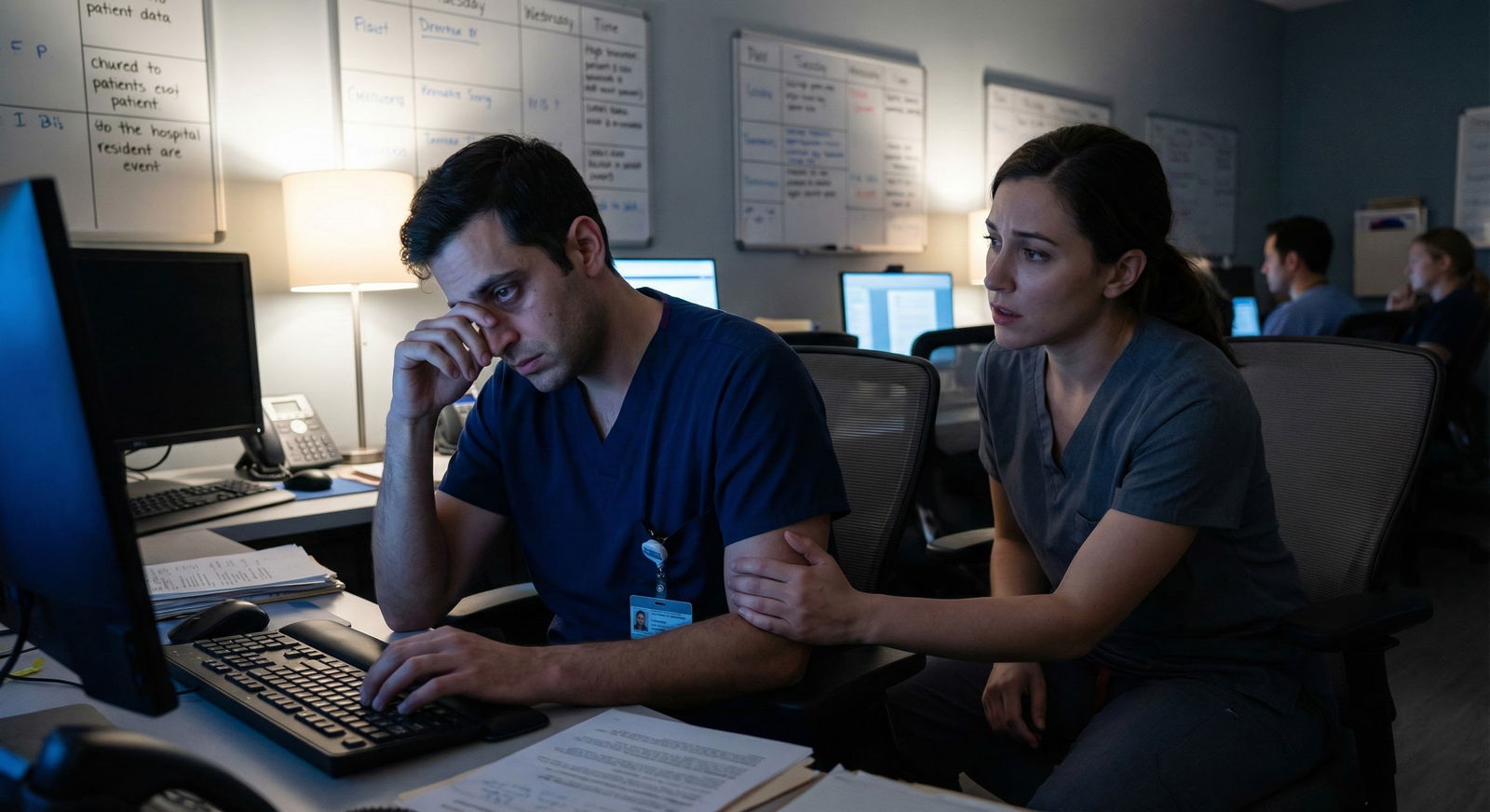
What if the only thing standing between you and burning out this year is one brave conversation about your call schedule?
Here’s the blunt answer: Yes, you can negotiate call and weekend adjustments as a resident. People do it all the time. But there are rules, politics, and hard limits. If you go in naive, you either get shut down or accidentally make enemies. If you go in strategic, you can often carve out the breathing room you need without tanking your reputation.
Let’s walk through how to do this like an adult in a system that doesn’t always treat you like one.
First Reality Check: What Is Actually Negotiable?
Not everything about call is flexible. Some things are hard-wired: ACGME rules, hospital coverage needs, union contracts, and program policy. Other things are surprisingly bendable if you ask the right way.
Here’s the rough split.
Non‑negotiable (in practice or by rule):
- Core coverage that keeps the hospital safe (night float, ICU, ED)
- ACGME duty hour requirements (80 hours, 1 day off in 7, etc.)
- Contracted obligations in union or institutional policies
- “Golden weekends” frequency if it’s already tight for everyone
Often negotiable (case‑by‑case):
- Swapping specific calls/weekends with co‑residents
- Small reductions for documented medical/mental health needs
- Temporary changes for major life events (childbirth, surgery, family crisis)
- Gradual return to full call after leave
- Adjusting which rotations you’re on when (less intense blocks during tough personal periods)
Quietly negotiable if you’re smart:
- Being taken off certain especially draining “extra” duties (frequent jeopardy, backup lists)
- Not being the default person who always picks up uncovered shifts
- More predictable patterns (e.g., grouping calls together vs scattered)
The key: don’t walk in asking, “Can you just give me fewer calls?” That sounds like you’re asking for a lighter job than everyone else. Instead you’re asking, “Can we adjust when and how I take call so I don’t break?”
Before You Ask: Do These 4 Things
You need to prep. Walking into your PD’s office with “I’m so burned out” and nothing else is how you get an empathy nod and zero change.

| Category | Value |
|---|---|
| Burnout/Exhaustion | 40 |
| Health Issue | 25 |
| Childcare | 15 |
| Family Illness | 10 |
| Education Needs | 10 |
1. Get specific about the problem
“I’m burned out” is vague. “4 straight q3 call weeks, no real day off in practice, and I’m not recovering between shifts” is actionable.
Write down:
- Exact rotations/call patterns that are killing you
- How many weekends in a row you’ve worked
- Any duty hour violations or close calls
- Concrete impacts: near errors, cognitive fog, panic attacks, insomnia, physical symptoms
You’re not whining. You’re documenting a patient safety and physician impairment risk.
2. Decide your goal in plain language
You need a clear ask:
- “I need at least one truly off weekend this month.”
- “I can’t safely do back‑to‑back 28‑hour calls right now; can we adjust sequence?”
- “After my upcoming surgery, I need a 4–6 week no-call period and then stepwise ramp‑up.”
If you don’t define what better looks like, they will define it for you. Usually in a way that preserves the schedule and sacrifices you.
3. Check the official rules
Look at:
- Your residency handbook
- Union contract (if you have one)
- ACGME program requirements and duty hour rules
You’re looking for:
- Maximum frequency of call
- Required number of days off
- Policies for medical leave, parental leave, and accommodations
This tells you whether your request is asking for basic compliance or for extra consideration. The first is easier to push hard on.
4. Line up quiet support
Talk—carefully—to:
- A senior resident you trust
- Your chief(s)
- A mentor or APD who’s known to be human
Ask, “Is there any flexibility with call for X situation?” Listen more than you speak. You’ll often hear: “We’ve done X for someone before” or “People usually talk to Y about this.”
Who To Talk To (And In What Order)
Don’t go straight to the program director with a vague complaint if you can avoid it. There’s a smarter sequence.

| Step | Description |
|---|---|
| Step 1 | Identify Specific Problem |
| Step 2 | Informal Chat with Senior or Mentor |
| Step 3 | Talk to Chief Resident |
| Step 4 | Confirm in Writing |
| Step 5 | Meeting with PD or APD |
| Step 6 | Involve GME or HR |
| Step 7 | Monitor and Follow Up |
| Step 8 | Solved with Swaps? |
| Step 9 | Need GME/HR? |
Step 1: Co‑residents and schedule swaps
First tier is horizontal: your peers.
- See what you can swap directly.
- Offer value: “I’ll take your random Sunday if you take my q3 call post‑night‑float.”
- Use whatever schedule system you’ve got (Amion, QGenda, spreadsheet) and send formal change requests as your program requires.
If you can fix it with swaps and no one is getting abused, that’s ideal.
Step 2: Chief residents
Cheifs are the unofficial schedule diplomats. They know the unwritten rules.
How to approach:
- Email or message: “Can we talk briefly about my call schedule? I’m worried about sustainability and safety.”
- In the meeting, be concrete and calm.
- Bring 1–2 proposed solutions, not just problems.
Good asks at this level:
- “Can we group my calls together so I have some real off stretches?”
- “Can someone else pick up x call if I cover y less intense shifts?”
- “Can we avoid me stacking ICU nights right after ED nights for the next month?”
Step 3: Program director / APD
Involve them when:
- Your health is at stake
- You’re hitting or approaching duty hour violations
- You need a formal adjustment (reduced call, accommodations, schedule redesign)
Go in like this:
- Describe the pattern and its impact. Short, factual.
- State your concern as a patient safety / physician safety problem, not “life is unfair.”
- Present 1–2 realistic possible solutions.
- Explicitly acknowledge fairness: “I don’t want to dump extra work on co‑residents; I’m open to trade‑offs or making this time-limited.”
That last part matters. They’re always thinking about precedent.
How To Frame Your Ask So They Actually Listen
Language matters. You’re in a hierarchy. Pretending otherwise is naive.
Use phrases like:
- “I’m concerned I’m not safe to practice at my current schedule.”
- “I’m reaching a limit where I’m worried about making mistakes.”
- “I’m not asking to do less work than my peers, but I need to distribute that work differently.”
Avoid:
- “It’s unfair that…”
- “Everyone else seems fine…” (That can backfire immediately.)
- “I just can’t deal with nights/weekends.”
Tie everything back to three themes:
- Patient safety
- Compliance with duty hour and institutional policies
- Retaining you as a functional, long-term member of the workforce
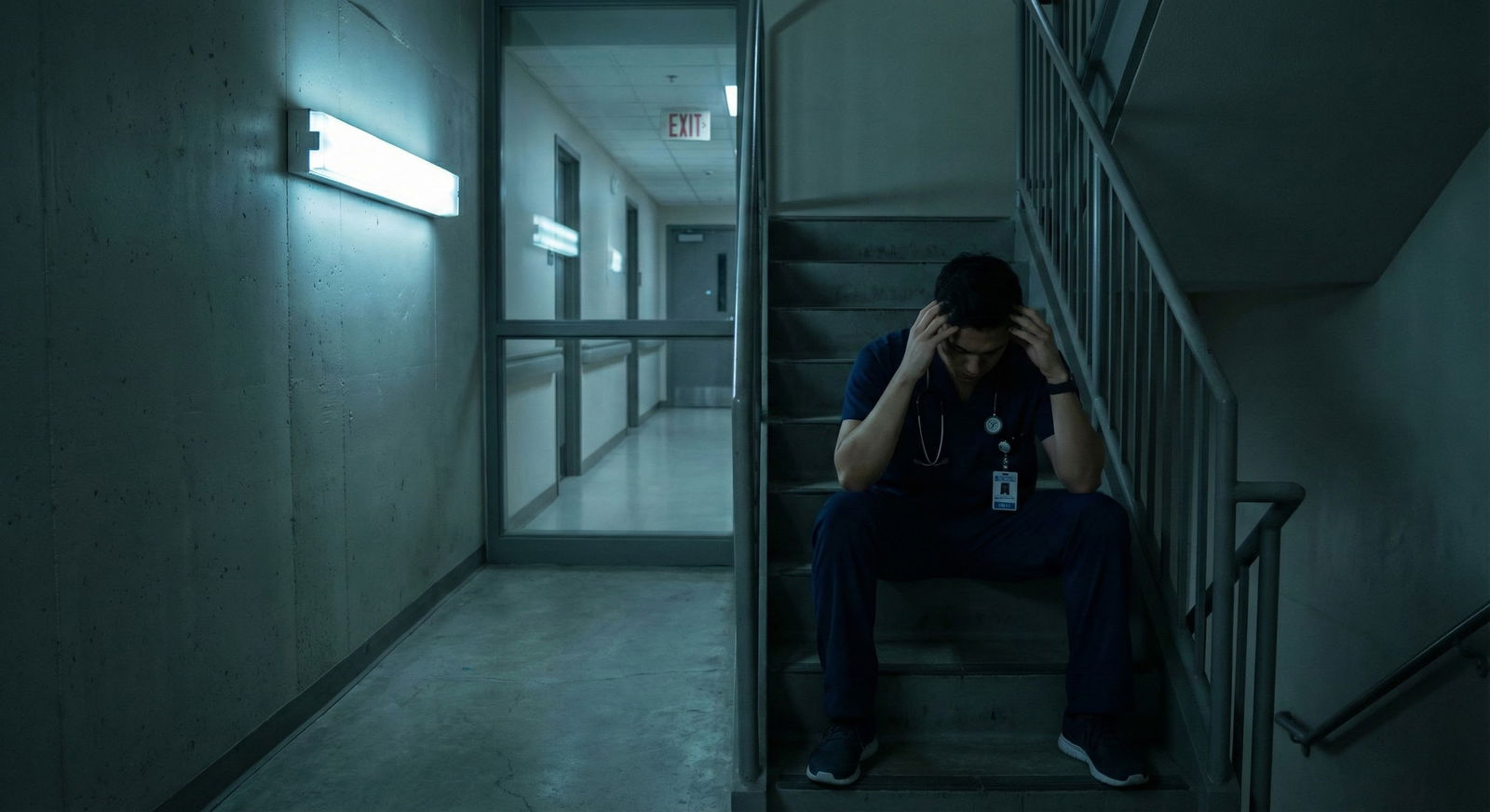
When You Have a Health or Mental Health Issue
This is a different category. And honestly, underused.
If you have:
- Major depression, anxiety, panic attacks
- Pregnancy complications
- A new medical diagnosis (autoimmune, seizure disorder, etc.)
- Sleep disorder, cardiac issues, anything worsened by nights
You’re not asking for a favor. You’re asking for a reasonable accommodation.
Steps here:
- Get evaluated by a physician or mental health professional.
- Get a letter that clearly states functional limitations, not just diagnoses. Example: “Should avoid overnight call for the next 8 weeks” or “Needs guaranteed 1 day off in 7 with at least 24 consecutive hours.”
- Take that letter to your PD and, if your institution has it, GME/HR or an accommodations office.
Legally and ethically, programs have to engage in an “interactive process” around accommodations. That doesn’t mean they must give you exactly what you ask for, but “too bad, deal with it” is not an acceptable answer.
Expect:
- Some schedule re‑shuffling
- Potential extension of training if you significantly reduce certain types of call
- Some awkwardness with co‑residents unless leadership handles messaging well
But I’ll say this bluntly: extended training is better than a breakdown, a suicide attempt, or a license‑threatening error. Every time.
How To Protect Yourself Politically
You’re in a small ecosystem. Word travels. You need to be strategic.
| Situation | Smart Approach | Risky Approach |
|---|---|---|
| Feeling overwhelmed by q3 call | Meet with chiefs, propose swaps | Complain repeatedly in the workroom |
| New mental health diagnosis | Get letter, involve PD + GME | Tell co-residents only, hide from PD |
| Near miss from fatigue | Document, email PD about safety concern | Joke about it and keep quiet |
| Need reduced call during pregnancy | Request formal accommodation | Informally ask for “lighter schedule” |
| Ongoing scheduling unfairness | Track data, bring pattern to PD | Accuse chiefs of favoritism |
Basic political rules:
- Never ambush a chief or PD in front of others with this stuff. Always ask for a short private meeting.
- Don’t build your case as “I’m working harder than everyone else” unless you have hard data and are ready for conflict.
- Once you get an adjustment, don’t brag about it or frame it as “I got out of call.” You will get shredded in the gossip channel.
Instead, emphasize: “I’m working with the program to stay safe and effective. It’s temporary, and I’ll pull my weight in other ways.”
What If They Say No?
Sometimes they will. Or they’ll offer a cosmetic change that doesn’t actually help.

| Category | Value |
|---|---|
| Approved as Requested | 30 |
| Partial Adjustment | 35 |
| Initially Denied, Then Modified | 15 |
| Fully Denied | 20 |
If the answer is no or useless:
- Clarify: “Can you help me understand the constraints? What can be adjusted, if anything?”
- Ask: “If this becomes unsafe or unmanageable, what’s the right next step for me?” (You’re on record flagging risk.)
- Immediately start documenting: duty hours, emails, any incidents.
- Bring in the next layer: GME office, ombudsperson, union (if present).
Where things are serious: if you’re not safe to work, you do not keep silently working. That is how careers end.
Be willing to say: “I’m not safe to take this call tonight” and escalate up the chain. Nobody likes hearing that, but legally and ethically, that statement triggers a different level of responsibility for them.
How To Negotiate Without Burning Bridges: A Script
Here’s a simple structure you can adapt for a PD or chief meeting.
Open with impact
“Over the last month I’ve had X, Y, Z call pattern. I’m noticing significant fatigue, trouble concentrating, and I’m worried about my ability to practice safely if this continues.”State the problem clearly
“Specifically, the back‑to‑back 28‑hour calls with only one day in between aren’t giving me enough time to recover.”Tie to safety and standards
“I know the program cares about patient safety and duty hour compliance, and I’m trying to be proactive before this turns into a real problem.”Propose concrete options
“I see a couple of possible solutions:- Shift one of these calls to later in the month and give me a real 24‑hour off period.
- Or allow me to swap this ICU weekend with a lighter weekend rotation and I’ll cover an extra shift there.”
Show fairness awareness
“I don’t want to offload work onto my co‑residents long‑term. I’m open to making this time‑limited or picking up non‑call responsibilities in exchange.”Ask for their ideas
“What options do you see that would be realistic from the program’s side?”
That structure keeps you from either rambling or sounding entitled.
What Actually Works Best in Real Life
Here’s what I’ve consistently seen work:
- Early, small adjustments beat late, desperate ones. Ask while it’s a yellow flag, not once you’re in full breakdown.
- Framing things as “distribution of workload” rather than “less workload” goes down smoother.
- Bringing options that show you understand coverage needs builds trust.
- Involving a mental health professional and GME gets taken more seriously than vague burnout complaints.
And what usually fails:
- Whining in the workroom but never formally asking for change.
- Acting like you’re the only one suffering.
- Threatening to quit in the heat of the moment.
- Expecting change without any trade‑off or compromise.
FAQs
1. Can I ask for no nights or no weekends at all?
You can ask, but for most core specialties the honest answer is no—at least not long‑term. Nights and weekends are part of core training and service. You’re more likely to get a temporary exemption (for health, pregnancy, acute crisis) or modified frequency than a blanket lifetime pass.
2. Will asking for call adjustments hurt my fellowship chances?
Not automatically. What hurts you is being labeled unreliable or difficult. If you approach things professionally, document health or safety reasons, and remain strong clinically, most PDs don’t go telling fellowship directors, “This person once negotiated their schedule.” If you’re worried, ask your PD directly how they see it.
3. Do I have to disclose specifics of my mental health diagnosis to my PD?
No. You can keep it high‑level. Something like: “I’m under the care of a mental health professional who recommends avoiding overnight call for the next X weeks.” If you involve HR or an accommodations office, they usually only share functional limitations, not the full diagnosis, unless you explicitly authorize it.
4. What if my co‑residents resent me for getting schedule changes?
Some might. Especially in small programs. You can lower the temperature by being transparent about pulling your weight in other ways (“I’m happy to help with notes/consults/research/teaching”) and framing this as time‑limited. At the end of the day, your health and safety outrank their opinion. Full stop.
5. Can I use duty-hour violations as leverage to demand fewer calls?
You can and should report duty-hour violations—internally, through official systems, or both. But “you violated duty hours, so I never want to do call again” is not a reasonable ask. A more effective angle: “Our current call pattern is pushing us over ACGME limits. Can we redesign the system so it’s compliant and safer, maybe by adjusting X and Y?”
6. What’s one thing I can do this week if my call schedule is already crushing me?
Take 10 minutes today to map out your next 4–6 weeks of call, identify exactly which days/blocks are unsustainable, and draft a short email to your chief requesting a brief meeting: “I’m worried my current call schedule isn’t sustainable or safe. Could we talk about options?” That one email starts turning vague misery into a solvable problem.
Open your schedule right now. Circle the one call stretch you’re genuinely afraid of. That’s your starting point. Write down how you’d change just that piece and who you need to talk to first. Then send the message to set up that conversation.



















