
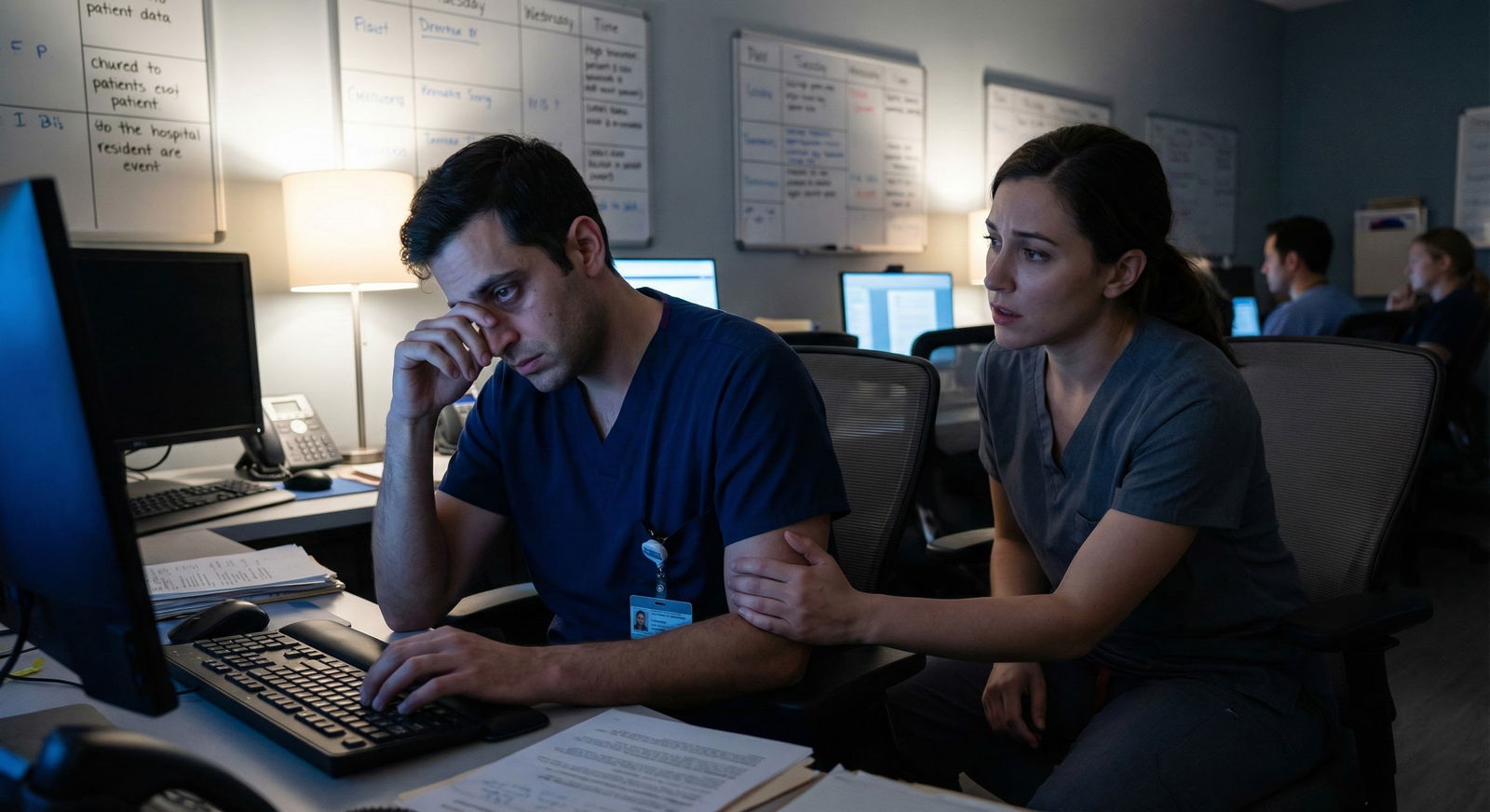
The way most residents “handle” burnout is backwards—and it is absolutely crushing people who would otherwise be great physicians.
You do not prevent burnout by downloading a mindfulness app and hoping for the best. You prevent burnout by building a personal, brutally realistic, low-friction plan that fits how your life actually works on service. And then you make it so simple you can follow it even post–night float with 3 hours of sleep.
That’s what I’m going to walk you through.
Step 1: Stop Aiming for “Wellness,” Aim for “Bare-Minimum Sustainable”
You are not building a wellness retreat. You’re building a survival protocol.
The right bar for residency is not:
“I will feel great and have perfect work–life balance.”
The right bar is:
“I can function, grow, and not hate my life long term.”
So first, you define your minimum sustainable baseline, not your ideal.
Grab a scrap of paper (or Notes on your phone) and answer three questions, honestly:
When I’m doing okay (not great, just okay), what does my life look like?
- Sleep: roughly how many hours, even on tough rotations?
- Food: what does “not garbage all the time” actually mean for you?
- Movement: what’s the smallest amount that still helps your brain?
- Human contact: how often do you need to talk to someone who isn’t a patient or attending?
When I’ve been close to burning out before, what were the early warning signs? Common ones I see:
- You stop returning texts from friends entirely
- You’re irrationally angry at every consult
- You start fantasizing about walking out mid-shift
- You’re eating once a day and it’s vending machine sugar
- You feel numb with patients instead of engaged
What is non-negotiable for you as a human? This is not aspirational. It’s core identity stuff:
- “I need to talk to my partner at least 10 minutes most days.”
- “I need some form of spiritual or reflective practice weekly.”
- “I need time with my kid where I’m not charting.”
Write it down. This becomes your definition of sustainable, not someone else’s Instagram version of wellness.
Step 2: Build a Tiny, Rotation-Proof Core Routine
If your “burnout prevention plan” only works on elective, it’s useless.
Design a core routine that still works on ICU, nights, and when you’re doing 6 days a week.
Rule: it must fit into 15–25 minutes total on a bad day, broken into tiny pieces.
Use this template and customize it:
Micro-sleep anchor
- Example: “In bed, phone away, by 11:30 p.m. on non-call nights whenever humanly possible.”
- Or if your schedule is chaos: “I protect one continuous 4–5 hour block of sleep, no matter what else I sacrifice.”
5–10 minute movement block Examples:
- 10 squats + 10 pushups + 60 seconds of stretching in your room
- Walk the long way out of the hospital and climb one extra flight of stairs
- 7-minute workout YouTube in scrubs before shower
3–5 minute mental reset Don’t overcomplicate this.
- 10 slow breaths with your eyes closed at the end of shift, before you touch your phone
- A two-sentence nightly check-in: “What drained me today? What helped?”
- Box breathing while the computer is loading
1 meaningful connection Minimum effective dose:
- Voice note or quick call to one human you actually like
- Text your co-resident something supportive after a brutal shift
- 5 minutes of real presence with your partner or kid, no screens
On paper, this looks ridiculously small. Good. That’s the point. The win is: “I actually do it most days,” not “It impresses a productivity blogger.”
Step 3: Map Your Rotations and Pre-Plan Adjustments
Your life is not one lifestyle. It’s 100 different ones depending on rotation and call.
So you don’t make one burnout plan. You make a base plan plus tiny rotation-specific versions.
Make a quick table for yourself like this:
| Rotation Type | Biggest Risk | Core Adjustment |
|---|---|---|
| ICU | Sleep debt | Protect one 4–5 hour block daily |
| Nights | Isolation | Daily check-in with one friend or family |
| Ward Days | Overload | 5-minute post-shift brain dump before home |
| Clinic | Emotional fatigue | 10-minute walk alone before going home |
Now, for each major rotation type you have, answer three questions in a sentence or two:
What usually gets sacrificed first on this rotation?
(Sleep? Food? Movement? Friends? Basic hygiene?)What is realistic minimum self-care here?
Not ideal. Minimum. For ICU nights, that might literally be:- One actual meal.
- One 10-minute walk.
- One conversation with someone you trust each day.
What has helped you cope on this rotation in the past? Things like:
- “Leaving the hospital with a co-resident so we can debrief.”
- “Pre-packing three high-protein snacks.”
- “Listening to non-medical podcasts on the drive.”
You’re building rotation playbooks, not vibes.
Step 4: Set Clear Early-Warning Triggers and “If–Then” Rules
Burnout doesn’t slam into you out of nowhere. It leaks in.
You want hard, specific tripwires and pre-decided responses so you do not try to “tough it out” until you are fantasizing about quitting medicine.
Go back to the early warning signs you listed. Turn each into:
- A trigger you can observe
- One automatic action you’ve pre-committed to
Examples:
Trigger: “I wake up with a pit in my stomach about going in 3 days in a row.”
If–then: “If that happens, I text [Friend/Co-resident] and say ‘I’m not okay, can we talk this week?’ and I schedule a 15-minute check-in.”
Trigger: “I haven’t done anything non-medical for myself in 7 days.”
If–then: “I must block 30 minutes on my next post-call or golden day for something fun or quiet—no exceptions, even if the notes are behind.”
Trigger: “I’m snapping at nurses or med students repeatedly.”
If–then: “I email or page my program’s confidential wellness resource or faculty mentor and ask for a quick conversation about coping, not performance.”
Trigger: “I’m having thoughts like ‘I don’t care what happens to this patient.’”
If–then: “I treat that as a red alert. I must talk to someone—trusted attending, program leadership, therapy—within 48 hours.”
Write 3–5 of these if–then rules. Keep them short. You’re pre-writing your own rescue protocol.
Step 5: Remove Friction: Make the Healthy Choice the Easy Choice
Most residents do not fail at self-care because they don’t know what to do. They fail because they’re exhausted and the easiest option is the worst one.
You fix that by making the good choices frictionless and the bad choices slightly annoying.
Here’s how:
Pre-pack survival kits
- Work bag: 2–3 decent snacks (nuts, protein bar, something with actual substance), spare socks, ibuprofen, lip balm, a small notepad.
- Locker or call room: instant oatmeal, tea/coffee, a phone charger, earplugs, eye mask.
Default meals Decide ahead of time:
- One “I’m dead tired” breakfast you can make in 2 minutes (yogurt + granola, overnight oats, whatever).
- One “I refuse to cook” dinner that’s still better than DoorDash fries (frozen meals that aren’t junk, pre-made salads with rotisserie chicken).
Automation
- Automatic grocery delivery every 1–2 weeks with staples you always use.
- Refill prescriptions with auto-refill and mail order if possible.
- Schedule recurring blocks: therapy, coaching, spiritual support, etc., like you do continuity clinic.
Speed bumps on bad habits
- Move doom-scroll apps off your home screen.
- No phone in bed unless you’re on call; charger across the room.
- Decide a time cut-off: “If I get home after 10 p.m., I’m not allowed to open the laptop for charts.”
You’re not relying on willpower. You’re building a system that assumes you’ll be tired and lazy—because you will be.

| Category | Value |
|---|---|
| Work | 60 |
| Sleep | 40 |
| Commute | 10 |
| Admin/Charting | 15 |
| Personal Care | 15 |
Step 6: Write a One-Page Burnout Prevention Plan
If your plan is longer than one page, you’ll never look at it.
Use these sections, keep it tight:
My Baseline
- “When I’m okay, I’m sleeping about X hours, eating Y real meals, and connecting with people Z times per week.”
My Non-Negotiables
- 3–5 bullets like:
- Talk to partner 10 minutes most days
- One small movement session on at least 4 days per week
- One protected block for something I enjoy every 1–2 weeks
- 3–5 bullets like:
My Daily Minimums on Hard Rotations
- “On ICU/nights, my minimum: one real meal, 4–5 hours of sleep in one block, one short connection with someone I trust.”
My Triggers and If–Then Rules
- List those 3–5 early warning triggers and exact actions.
My Support Contacts
- 2–3 humans you can contact when things start sliding:
- A co-resident you can be honest with
- A faculty mentor
- A therapist / counseling service / employee assistance
- Include actual names, numbers/emails.
- 2–3 humans you can contact when things start sliding:
Emergency Protocol One short paragraph that answers:
- “If I start having persistent thoughts of self-harm, or that everyone would be better off without me, I will:”
- Tell someone in person or by phone immediately (not just text)
- Use my institution’s urgent mental health resource or national crisis line
- Remove myself from clinical duties if I truly feel unsafe, no matter how guilty I feel
- “If I start having persistent thoughts of self-harm, or that everyone would be better off without me, I will:”
Print this. Put it:
- In your locker
- In your bag
- As a pinned note on your phone
You’re creating something you can literally pull out at 2 a.m. and follow.
Step 7: Schedule 10-Minute Weekly Reviews (Yes, Really)
The plan is worthless if you never adjust it.
You don’t need a journaling retreat. You need 10 minutes once a week.
Pick a consistent time:
- Sunday afternoon
- Post-call when you’re home and showered
- Day off morning with coffee
Run through five rapid-fire questions:
- How burned out do I feel on a 0–10 scale this week?
- What helped even a little?
- What made things clearly worse?
- Did I hit my minimums (not my ideals)?
- What tiny adjustment am I making for this coming week?
Examples of tiny adjustments:
- “Last week I went three days without a real meal. This week I’m pre-packing 3 microwavable meals.”
- “I skipped the movement block entirely. This week I’ll do it only 3 days and call that a win.”
- “I’m still stewing about a bad patient outcome. I’ll bring it to supervision instead of ruminating alone.”
You’re iterating. Not self-flagellating.

| Step | Description |
|---|---|
| Step 1 | Rotation Starts |
| Step 2 | Check One Page Plan |
| Step 3 | Identify Rotation Type |
| Step 4 | Apply Rotation Adjustments |
| Step 5 | Use Daily Minimum Routine |
| Step 6 | Continue Routine |
| Step 7 | Activate If Then Actions |
| Step 8 | Contact Support If Needed |
| Step 9 | Weekly 10 Minute Review |
| Step 10 | Early Warning Trigger? |
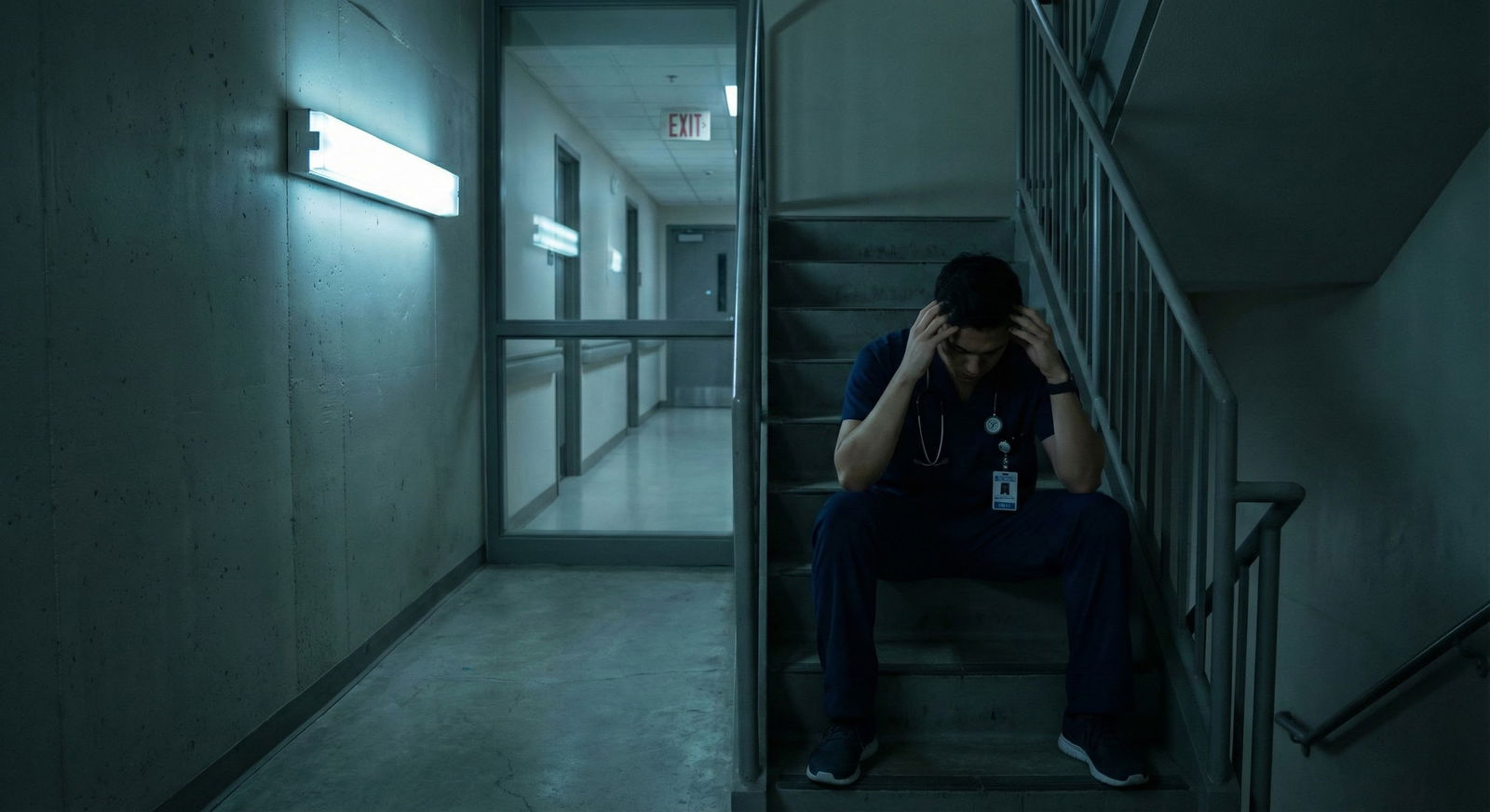
Step 8: Know When the Problem Is the System, Not You
Here’s the uncomfortable truth: no personal plan can compensate for a toxic program indefinitely.
Your burnout prevention plan is not a shield against:
- Systemic abuse
- Chronic unsafe staffing
- Retaliation for asking for help
- Persistent discrimination or harassment
Warning signs that you’re dealing with a system problem:
- Every resident on your service looks destroyed, not just tired
- People openly brag about how little they sleep as a badge of honor
- You’re discouraged from seeking medical or mental health care
- You’re punished or shamed for normal human limits
In those cases, part of your burnout plan might include:
- Documenting concerns
- Finding allies in other departments or GME
- Quietly exploring transfer or long-term exit options
You are allowed to decide that your life and health are worth more than “toughing it out” in a broken environment.
Step 9: Put It All Together in 5 Minutes Today
If you want a quick starting template, here’s a simple fill-in-the-blank you can use right now:
My minimum sustainable baseline:
- Sleep: I function at ___ hours most nights.
- Food: I need at least ___ real meals per day.
- Movement: I can realistically do ___ minutes, ___ days/week.
- People: I need to connect with someone I care about at least ___ times/week.
My non-negotiables (3–5 bullets).
My daily minimum routine on hard rotations:
- Sleep: __________________________________
- Food: ___________________________________
- Movement: _______________________________
- Connection: _____________________________
My top 3 early warning signs:
And my if–then rules for each.
My support list:
- Peer: __________________________________
- Faculty: _______________________________
- Mental health: _________________________
Draft it. It does not have to be beautiful. It has to exist.
Then refine it during your next weekly 10-minute review.

| Category | With Plan | Without Plan |
|---|---|---|
| Month 1 | 6 | 6 |
| Month 2 | 5 | 7 |
| Month 3 | 4 | 8 |
| Month 4 | 4 | 9 |
FAQs
1. What if I’m already burned out—does a prevention plan still matter?
Yes, but you’re no longer in pure prevention mode; you’re in stabilization and repair. The steps are the same, but your priorities shift:
- First: address immediate safety (sleep, mental health, any self-harm thoughts).
- Second: lighten the load where possible (vacation, schedule changes, medical leave if needed).
- Third: then use the plan to stop yourself from sliding back when you start to recover.
If you’re crying in your car regularly, waking up dreading every single day, or having dark thoughts, you should treat that as a clinical issue as well as a burnout issue. Reach out for professional help. That’s not weakness; that’s doing the job of being your own patient.
2. How do I bring this up with my program without looking “weak”?
You do it in the language programs respect: patient care and longevity.
Examples:
- “I want to make sure I can sustain my performance long term. I’ve noticed I’m exhausted enough that it’s getting harder to focus in the afternoons. Can we talk about strategies or resources for coping better?”
- “I’m working on a personal burnout prevention plan because I want to be here and be effective. I’d appreciate your perspective or any institutional support that aligns with that.”
You’re not saying “I can’t hack it.” You’re saying, “I’m taking my career and my patients seriously enough to treat my own health as part of the system.”
3. What if I literally have no time for any of this on some rotations?
Then you scale even smaller. There will be days when your entire “plan” is:
- Ate once
- Slept 4 hours
- Texted one friend “I’m alive but dying, talk later”
Fine. The plan is not a perfection contract. It’s a floor, not a ceiling. If you truly have zero time to eat, sleep, or pee consistently for weeks, that’s an unsafe environment and needs escalation beyond a personal plan.
4. Do I really need therapy, or can I just use this plan?
A plan is not a substitute for treatment. Use both when:
- You have persistent anhedonia (nothing feels good), hopelessness, or irritability
- You’re using alcohol or substances more to cope
- You’re having thoughts like “My patients would be better off with someone else” or “I don’t want to be here anymore”
Therapy gives you tools and a private, confidential space. Your plan makes those tools usable in the chaos of residency. They work together.
5. How detailed should my rotation-specific adjustments be?
Keep them rough and practical. You don’t need a novel for each rotation. For example, for Nights:
- Sleep: blackout curtains, white noise, phone on Do Not Disturb
- Food: prep 3 meals, keep snacks in bag
- People: 5-minute call with partner before shift; group chat with co-residents alive and active
If you’re spending more than 5–10 minutes writing it, you’re overbuilding it.
6. What if my co-residents don’t care about any of this?
Some will roll their eyes. Some are quietly drowning and will latch onto it. You don’t need group consensus to protect yourself.
You can still:
- Share pieces of your plan with the one or two people you trust
- Normalize short walks, real meals, and early-warning language (“I’m hitting my yellow flags this week”)
- Be the one person in the room who says, “Hey, anyone eaten today?”
People follow behavior more than they follow lectures.
7. How often should I rewrite the whole plan?
Not often. Rewriting is procrastination disguised as productivity.
Treat your plan like this:
- Core stays the same for 6–12 months
- Tiny tweaks in your 10-minute weekly reviews
- Bigger revision after major transitions (intern to PGY-2, changing programs, new city, major life changes like a new baby)
Two or three key points to walk away with:
- Your burnout plan must be small, rotation-proof, and brutally realistic or you will not use it.
- Early-warning triggers plus if–then rules turn vague “I should take care of myself” into actual action.
- You cannot fix a toxic system with self-care, but you can protect your bandwidth, spot red flags earlier, and make deliberate choices about what you’re willing to endure—and what you’re not.




















