
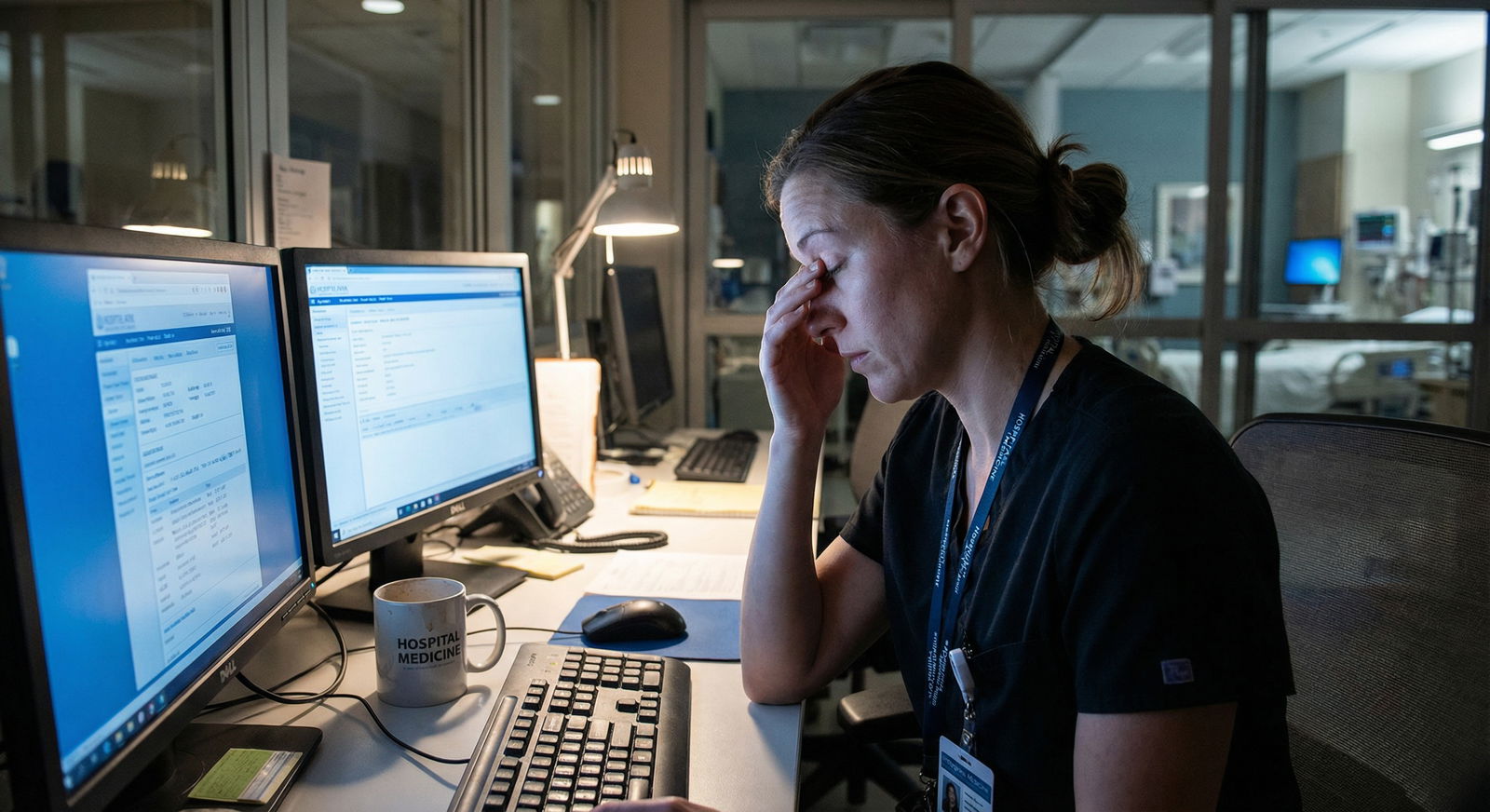
White-knuckling your way through 16-hour shifts is a terrible strategy. You need a system, not more grit.
I am going to show you exactly how to break a 16-hour shift into manageable blocks so you stop feeling like you are drowning by hour 10.
This is not about “self-care” platitudes. This is a tactical operating system for long shifts:
- How to structure the shift into predictable blocks
- When to do which type of work
- How to defend micro-breaks and food without screwing your team
- How to adapt the system for days vs nights, ward vs ICU vs ED
Use what fits your specialty and schedule, but keep the core structure. The residents I have seen do this well are less burned out, make fewer mistakes, and actually remember the drive home.
The Core Idea: Turn 16 Hours into 6 Functional Blocks
You will not survive 16 hours by “pushing through.” You survive it by only experiencing 2–3 hours at a time.
Here is the simple architecture:
| Block | Time (example) | Primary Focus |
|---|---|---|
| 0 | -0:15 to 0:00 | Pre-brief and setup |
| 1 | 0:00–3:00 | High-focus tasks |
| 2 | 3:00–6:00 | Rounds / procedures / throughput |
| 3 | 6:00–9:00 | Admin, calls, “loose ends” |
| 4 | 9:00–12:00 | Second wind work + teaching |
| 5 | 12:00–16:00 | Safe landing / handoff prep |
Time anchors will change (days vs nights, when rounds happen, etc.), but the function of each block stays similar:
- First third: high-cognitive, proactive
- Middle third: throughput, tasks, documentation
- Final third: consolidation, cleanup, handoff
You are not “surviving 16 hours.” You are doing:
- Block 1 well
- Then Block 2 well
- Then Block 3 well
Repeat until done.
Now let me break it down into something you can actually run on your next shift.
Step 1: The 15-Minute Pre-Shift Setup (Block 0)
If you walk onto the floor at 6:59 for a 7:00 start, you are playing from behind before you touch a chart.
Show up 10–15 minutes early. I know—unpaid. Do it anyway. Those 15 minutes buy you hours of sanity.
Your 15-minute script
Personal Setup (3–4 minutes)
Drop your bag, bathroom, water, coffee if needed. Phone on:- Do Not Disturb
- Exceptions: hospital, significant other, childcare
Tool Setup (4–5 minutes)
- Log into EHR on two workstations if possible: one for notes, one for orders/inbox
- Print or load your list with:
- Room numbers
- Diagnosis / service
- Key labs / vitals (space to fill in)
- Open:
- EHR “patient list” tab
- Labs/Imaging tab
- Inbox/Results tab
Shift Intent (2 minutes)
Quick mental outline:- What are the big predictable anchor events? (AM rounds, PM rounds, signout, scheduled procedures, admissions surge times)
- What is success today? Examples:
- “No unfinished notes at signout”
- “Every patient seen before rounds”
- “At least one real 10-minute break”
Rapid Incoming Intel (3–5 minutes)
Before the outgoing resident starts drowning you in details:- Ask: “Top 3 sickest patients?” Write them in big letters.
- Ask: “Any time bombs? Pending imaging, angry families, discharge disasters?”
- Ask: “Pattern of admissions today/tonight?” (The ED surge times matter.)
You are building a mental map before the chaos hits. That alone makes the shift feel 30% more manageable.
Step 2: Block 1 – The First 3 Hours Are Sacred
This is your prime time. Brain is freshest, decision-making is better, and you have the most control.
Use it ruthlessly.
Block 1 goals
- Identify and stabilize the sickest patients
- Front-load the most cognitively demanding work
- Set up the rest of the shift
Concrete actions for Block 1 (0:00–3:00)
Triage your list (15–20 minutes)
Mark each patient:- A = Sick / unstable / likely to crash
- B = Moderate / may need changes
- C = Stable / likely no major changes
Start with A, then B. C gets done later.
See A patients first (60–90 minutes)
For each A:- Quick chart review (1–2 minutes): overnight events, vitals trend, new imaging, labs
- Bedside assessment: focused but thorough
- Immediate orders for:
- Hemodynamics (fluids, pressors consult, etc.)
- Oxygenation/vent changes
- Critical labs/imaging
- One-liner note skeleton in your template (even just HPI/assessment bullets)
Do not fully write the note unless required pre-rounding. Just enough structure to finish faster later.
Hit key B patients next (remaining time)
Same pattern but faster. Goal: you have eyes on every A/B hot spot before rounds or admissions surge.Fast communication loops
- Page primary nurse early for anticipated changes: “Likely to increase diuresis / watch urine output.”
- Message your senior/attending early about anything that makes your gut clench.
You are building momentum, not perfection. The perfection comes later in documentation blocks.
Step 3: Align Blocks with Real-World Anchors
Your schedule is not theoretical. It is dictated by rounds, ED dumps, OR cases, and nursing shift changes.
So you align your 3-hour blocks to those anchors, not to a clock you made up.
Example: Day inpatient ward shift (7:00–23:00)
Block 0 (6:45–7:00)
Pre-setup and handoff prepBlock 1 (7:00–10:00) – Pre-rounding + prioritization
- See A/B patients
- Get vital pre-round labs ordered
- Identify 1–2 likely discharges
Block 2 (10:00–13:00) – Rounds + orders
- Focus on execution:
- Orders in during or immediately after each patient discussion
- Update families if possible right after room is done
- Protect a 10-minute snack break after rounds if humanly possible
- Focus on execution:
Block 3 (13:00–16:00) – Documentation + discharges
- Finish notes
- Push discharges over the finish line
- Call consults when you have the whole picture
Block 4 (16:00–19:00) – New admits / late issues
- Admit flow from ED
- Address late-afternoon problems (fevers, AKI, delirium)
- Micro-review sick patients again after major admits
Block 5 (19:00–23:00) – Consolidation + safe signout
- Finish admits notes/orders
- Handoff list with:
- 3 sickest patients
- Active issues
- “If X, then Y” instructions
Example: Night ICU shift (19:00–11:00)
- Block 0 (18:45–19:00) – Setup + sickest patients from outgoing team
- Block 1 (19:00–22:00) – ICU assessment and early interventions
- Block 2 (22:00–01:00) – Procedures, sedation optimization, vent tuning
- Block 3 (01:00–04:00) – Documentation and labs, micro-breaks
- Block 4 (04:00–07:00) – Pre-round labs / imaging / early morning events
- Block 5 (07:00–11:00) – Morning rounds + handoff/transition work
The details change. The principle does not: every 3-ish hours has a dominant job.
Step 4: Running Each Block: A Simple 5-Part Loop
Within each 2–3 hour block, use the same loop:
- List
- Triage
- Execute
- Document
- Reset
1. List (2–3 minutes)
- Update your patient list: discharges off, new admits on
- Scan for new labs/imaging flags
2. Triage (5 minutes)
Ask yourself:
- Who can deteriorate in the next 2 hours?
- Who is blocking flow (ED holds, late discharges)?
- What has a hard external deadline? (OR time, procedure slot, transport)
Rank the top 3 priorities for this block. Write them at the top of your paper list or a sticky note:
- “Block 3 priorities: finish 2 notes, call renal, dispo 402B”
3. Execute (60–90 minutes)
Focused, phone-away work on those top 3 items. Examples:
- See and stabilize sick patient
- Straight-through admit: see patient → orders → admit note skeleton
- Push a discharge to completion: med rec, follow-up appts, paperwork
Aim to batch similar tasks: 2–3 notes in a row, or 2–3 phone calls in a row.
4. Document (30–45 minutes)
Do not leave documentation for “later” (which never comes).
- Use templates and dot phrases aggressively
- Write as you go when possible:
- After each patient, drop in a short note skeleton
- At end of block, complete the details
Even for nights: get at least short documentation down while events are fresh.
5. Reset (5–10 minutes)
At the end of the block:
- Quick list update
- Check tasks: what is still open?
- Plan the first task of the next block
This reset is like a mini “new shift” every few hours. It keeps the work from blurring into a 16-hour smear of chaos.
Step 5: Protecting Micro-Breaks Without Abandoning Your Team
Residents do one of two dumb things:
- Never take breaks “because patients” → degrade cognitively and emotionally
- Take unannounced, long breaks → crush their co-residents
You are going to do neither.
Use the 3–Block Rule
In every 16-hour shift, pick two blocks where you will aim for:
- One 10–15 minute break
- One 5-minute reset
Usually:
- Block 2 or 3 for a real snack/food
- Block 4 or 5 for a 10-minute “I need to not talk to humans” break
How to make breaks actually happen
Announce the plan
“After we finish these two admits, I am going to take 10 minutes to eat. Then you should go.”
This normalizes breaks and keeps it fair.Choose timing sanely
- Not when a patient is crashing
- Not when 4 ED admits are waiting
- After you have addressed immediate A patients
Go completely off for those minutes
- Step away from the nurses’ station
- Phone on vibrate; check once midway for true emergencies
- No charting during this time. Your brain needs a different mode.
Short “micro-breaks” throughout
Use natural waits:- While labs are pending
- After putting in a big order set
- After two consecutive notes
Stand up. Stretch. Water. 60 seconds is enough to reset.
Forget the fantasy of a 45-minute lunch. Own the 5–15 minute windows you can actually protect.
Step 6: Managing Admissions, Crashes, and Other Chaos
Your beautiful block schedule will get wrecked by reality. That is expected.
The system is not there to prevent chaos. It is there to keep you from falling apart when chaos hits.
The “Crash Override” protocol
When something big hits (code, rapid response, crashing patient, ED admit storm):
Name it mentally
“Crash Override – Block 2.” This tricks your brain into seeing it as a temporary mode, not the new permanent reality.Drop to a simplified priority list
Only three questions matter:- Who can die or decompensate in the next hour?
- Who is waiting on me to make a major decision?
- Who can safely wait?
Document just enough
For the crisis:- Critical orders in
- Brief “event” note if required
- Everything else delayed until stabilizing
After the crisis (within 30–60 minutes)
- Reset your block:
- Update list
- Re-triage
- Identify time bombs created by the chaos (unseen patients, delayed discharges)
- Reset your block:
The point: You do not cling to your old plan during a crash. You temporarily suspend it, then explicitly reboot.
Step 7: A Simple Visual for Your Shift Flow
Sometimes you just need to see the structure as a path.

| Step | Description |
|---|---|
| Step 1 | Block 0 Setup |
| Step 2 | Block 1 High Focus |
| Step 3 | Block 2 Rounds or Procedures |
| Step 4 | Block 3 Admin and Notes |
| Step 5 | Block 4 Second Wind Work |
| Step 6 | Block 5 Handoff and Landing |
| Step 7 | Stabilize and Simplify |
| Step 8 | Major Event |
You are always somewhere on this path. Knowing that prevents the “I have no idea what I should be doing right now” spiral.
Step 8: Tracking Your Energy Across the 16 Hours
You are not a robot. Your mental performance is not flat across 16 hours.
Use it.

| Category | Value |
|---|---|
| Hour 1 | 90 |
| Hour 4 | 80 |
| Hour 7 | 65 |
| Hour 10 | 55 |
| Hour 13 | 50 |
| Hour 16 | 40 |
Roughly:
- Hours 1–4: High energy, best for complex decisions
- Hours 5–10: Moderate, best for throughput, documentation, standard admits
- Hours 11–16: Lower, best for checklists, handoff prep, routine tasks
Align your tasks:
- Schedule teaching, complex dispo planning, and difficult family meetings earlier when possible.
- Save routine progress notes, daily order renewals, and insurance forms for middle blocks.
- Final block: checklist and communication heavy, not creative.
Step 9: The Handoff-Ready Final Block
The last 2–4 hours decide whether you go home buzzing with anxiety or mostly at peace.
Treat Block 5 as a handoff block, not a “keep doing everything” block.
The 4-part landing checklist
Stabilize the sickest
- Re-evaluate A patients
- Make anticipatory plans:
- “If MAP < X, start Y and call Z”
- “If fever, culture pre-ordered”
Close documentation loops
- No loose admits if humanly possible
- Critical events documented
- At least brief notes for major overnight issues
Clean up orders and communication
- Stop outdated orders
- Clarify plans with nurses:
- “For 402B, okay to hold BP meds if SBP < 100.”
- Update consults with any overnight changes if day team needs it
Handoff that actually works
Your signout should include:- Sickest 3 patients, with:
- What happened
- What you are worried about
- What to do first if they worsen
- New admits with:
- Working diagnosis
- Pending studies that matter
- Clear to-do items for the next team, marked by priority
- Sickest 3 patients, with:
Handoff is not reading your entire note. It is delivering just enough targeted information for the next person not to get blindsided.
Step 10: Adapting the System to Your Reality
Every hospital, service, and attending is different. You are not going to run this system perfectly.
You do not need perfect. You need consistent enough.
Here is how to adjust:
If you are in the ED
- Shorter internal blocks: 90–120 minutes instead of 180
- Within each block:
- Pull 2–3 new patients quickly
- See all of them
- Then chart in a focused batch

| Category | Value |
|---|---|
| Random | 4 |
| Block System | 7 |
(Here “4” and “7” can represent number of fully completed patients per 3-hour period. Residents using block systems reliably close more complete charts per block.)
If you are in ICU
- Aggressively front-load assessments and interventions (Block 1 and 2)
- Use 01:00–04:00 for documentation and micro-rest if stable
- Protect 04:00–07:00 for labs, vent changes, and pre-round prep
If your attending is disorganized
You compensate by being more organized:
- Keep your block plan in your pocket list
- When they wander, you anchor:
- “We still need to see 402 and 410 before rounds end.”
- “I will put in the orders for these two, then circle back to consults.”
You can run this system quietly no matter how chaotic the service is.
A Quick Example Day: How It Looks in Real Life
Let me walk you through a typical resident day where this actually works.
Shift: 7:00–23:00, medicine wards, 16 patients
6:45–7:00 (Block 0)
Coffee. List printed. Ask night resident: “Top 3 sickest, any fires, any likely discharges?”7:00–10:00 (Block 1)
- 7:00–8:30: See A/B patients, quick note skeletons
- 8:30–9:15: See C patients briefly
- 9:15–10:00: Rapid pre-round order cleanup and look at labs
10:00–13:00 (Block 2)
- 10:00–12:00: Rounds, put in orders room-by-room
- 12:00–12:15: Snack break, quick reset
- 12:15–13:00: Call two consults, update one family
13:00–16:00 (Block 3)
- 13:00–14:30: Batch documentation – finish 10–12 notes
- 14:30–15:30: Discharge two patients, finalize follow-up
- 15:30–16:00: List reset, identify evening issues
16:00–19:00 (Block 4)
- 16:00–18:00: Two ED admits – see, orders, admit notes started
- 18:00–18:15: 10-minute mental break and quick snack
- 18:15–19:00: Check back on sick patients, adjust plans
19:00–23:00 (Block 5)
- 19:00–21:00: Finish admit documentation, tie loose ends
- 21:00–22:00: Handoff prep – clean list, mark sickest, finalize anticipatory guidance
- 22:00–23:00: Signout, final questions, brief debrief with co-resident, go home tired but not destroyed.
Is this idealized? A bit. But it is reachable a lot more often than you think when you commit to the structure.
FAQs
1. What if my service is so busy that I cannot stick to 3-hour blocks?
Then shrink them. Use 90–120 minute micro-blocks with the same structure:
- Quick list update
- Triage top 2–3 priorities
- Focused execution
- Minimal documentation
- Reset
The point is not “3 hours.” The point is that you are never asking, “Out of 50 things, what now?” You are always choosing the top few for this block.
2. How do I deal with attendings who change plans constantly?
You treat their chaos as an external variable and keep your internal structure:
- At the start of each block, note your top priorities
- When the attending changes direction, decide:
- Does this override my current top items? If yes, re-triage.
- If no, park it and say, “I will get to that after finishing X and Y.”
You cannot control their style. You can control how you organize the work they create.
3. Any tools or apps that actually help with this?
Keep it simple. Residents who try to build elaborate systems fail by week two.
Use:
- Paper list with sections for:
- A/B/C patients
- Block priorities
- Call-back / consult list
- Timer or watch:
- To mark end of blocks
- To protect 10–15 minute breaks
- EHR tools:
- Smart phrases / templates
- Pre-built order sets
- Flags or “starred” patients for sickest cases
The system is mostly behavioral, not technological.
4. How do I stop bringing the whole 16-hour shift home in my head?
Use a hard shutdown ritual in the last 10–15 minutes:
- Check list one final time
- Ask: “Is any patient actively unsafe if I leave now?” If no, you are done.
- Write down any lingering worries in a small notebook or your phone:
- “Ask about 402B renal function tomorrow.”
- On the walk or drive home, do not rehash decisions. Tell yourself, “Shift closed. I will think about it again when I badge in.”
Two key points to end on:
- Long shifts do not magically get easier. They get manageable when you impose structure: blocks, priorities, and protected resets.
- Your job on a 16-hour shift is not to be a hero. It is to make consistently decent decisions for many hours. Systems beat heroics every time.



















