Most attendings do not believe you when you say you’re “too tired to operate.”
They interpret it. They reframe it. But they almost never take it at face value.
Let me walk you through what actually runs through their heads, because no one is honest about this publicly. On the survey slides at grand rounds, everyone nods about wellness, duty hours, and fatigue risk management. Behind closed doors, in the workroom, the conversation is very different.
The First Thought: “Can I Trust You?”
The first thing an attending is assessing isn’t your fatigue. It’s your reliability.
When you say, “I’m too tired to operate,” most attendings silently translate that into: “Can I trust this resident with responsibility when it’s not convenient?”
They start a quick mental checklist:
- Is this a pattern or a one-off?
- How has this resident behaved overnight before?
- Are they usually the first to step up or the first to step back?
- How bad is the situation really? Life or death, or elective add-on?
I’ve sat in rooms where an attending hears that line and immediately says afterward, “That’s someone who’s never going to be chief material,” purely off that moment. Is that fair? No. Does it happen? All the time.
Here’s the critical nuance: attendings are not oblivious. Many of them did 120-hour weeks before duty hours existed. They know what true exhaustion feels like. But they also went through a culture where saying “no” to the OR wasn’t an option. Their default expectation is: the work gets done and the patient gets cared for. Your statement of fatigue is colliding with their identity.
So they’re not just judging your current state. They’re calibrating your future.
The Hidden Matrix in Their Heads
Attendings are constantly running a background risk-benefit analysis. They won’t say it out loud, but it looks roughly like this:
| Factor | What They’re Really Thinking |
|---|---|
| Prior work ethic | “Does this person usually hustle or usually complain?” |
| Performance trend | “Has their judgment been off recently?” |
| Case urgency | “Can this case wait or is it unsafe to delay?” |
| Backup options | “Is there another resident/fellow I trust more right now?” |
| Their own risk | “If something goes wrong, how will this look on me?” |
If you’re known as solid, hungry, and usually reliable, your “I’m too tired” gets interpreted as, “Wow, they must be really wrecked. I should listen.”
If you’re known as the person always “maxed on hours,” always citing wellness, always negotiating for less exposure, they interpret it as an excuse. Even if this time, you’re genuinely unsafe to operate.
Fair? Again, no. But that’s how humans work under pressure. They use pattern recognition.
What They Really Think About Duty Hours
Let’s strip away the fake committee language.
A significant chunk of surgical attendings think the 80-hour rule is soft. They won’t say it on record because they like having a job and not getting called into the DIO’s office. But in the OR lounge, here’s how it sounds:
“Back when I trained, we did Q2 and nobody asked how we felt; we just operated.”
“These residents are tired after 60 hours? Seriously?”
“If they can’t handle this call, they picked the wrong specialty.”
Before you react, understand where that’s coming from. They were conditioned in a system where your value was your stamina and your ability to perform under absurd pressure. The residents who survived and advanced into academic roles were the ones who could function dead tired. So their mental model of a “good surgeon” includes that trait almost by default.
Now plug your statement into that mindset: “I’m too tired to operate.”
They hear: “I can’t meet the standard that shaped me.”
They also hear: “You’re asking me to own this case alone,” because the moment you tap out, the burden shifts onto them. Which makes your fatigue not just your problem, but now their clinical, legal, and call-coverage problem.
And yet, paradoxically, they also know that the ACGME, hospital leadership, and risk management would destroy them if it came out that a resident told them they were unsafe and they forced them to operate anyway.
So they live in that tension between “be tough” and “don’t get sued or cited.”

| Category | Value |
|---|---|
| Patient safety | 90 |
| Legal risk | 75 |
| Resident development | 65 |
| Service coverage | 60 |
| Wellness optics | 40 |
They’ll never show you this bar chart, but that’s the unconscious ranking at many places.
The Spectrum of Attendings: Who You’re Actually Talking To
Not all attendings react the same way. You’re not up against a monolith, you’re up against types.
The Old-School Cowboy
Usually 50s–60s, trained pre-duty hours, often at big-name programs. Loves to tell stories that start with, “When I was a resident…”
When you say you’re too tired, this is what’s happening internally:
- Baseline reaction: “Soft.”
- Sub-reaction: “If I say what I’m really thinking, I’ll be written up.”
- Practical decision: “Alright, scrub out, I’ll do it,” said with that edge you feel in your spine.
Here’s the danger: you just got labeled. That attending will bring your name up in the faculty room. “We can’t depend on them at 3 AM.” That sticks.
The Performative Wellness Attending
Talks a lot about “well-being,” quotes literature on fatigue and error rates, is on some committee. On rounds, they ask, “How are you holding up?” in that slightly performative way.
Internally, they’re running two scripts:
- External: “Thank you for speaking up. Fatigue is real. We want you safe.”
- Internal: “This is the third time they’ve said this this block. Do they want to be a surgeon or not?”
They tend to be supportive the first couple of times, neutral the next few, and quietly negative if it’s recurrent. Their emails to leadership and their private evaluations do not always match.
The Quietly Protective Attending
You’ll know them because the senior residents love them. They remember being wrecked and nearly making catastrophic mistakes. They’re the ones who say, unprompted: “You’re done. Go home.”
When you say you’re too tired, they’re more likely to accept it at face value if you’re usually solid. They’re also the most likely to walk into the workroom later and say, “Listen, I’ll back you if you ever feel unsafe. But be very careful how often you use that line. People remember.”
This is the attending you should be studying, because they’ll tell you how the faculty really interpret things.
The Subtext: “Too Tired” vs “I Can’t Be Bothered”
Here’s the hardest truth: a lot of attendings don’t trust residents to distinguish between being dangerously impaired and just miserable.
Residents say “I’m too tired” to mean five very different things:
- I am literally nodding off and might harm someone.
- I’m wiped but could push if I had to.
- I’m emotionally done; I don’t want to be here anymore.
- I’m angry this got added on and I’m protesting.
- I think I’ve “hit” my duty hours and I want to go home.
Attendings have watched residents misuse fatigue language to negotiate. “I’m concerned about my duty hours” comes out exactly when the board looks heavy or a difficult attending is on.
Once faculty see that a few times, they start discounting the entire category. They assume 80% of “too tired” is actually “don’t want to” or “protecting my schedule,” and maybe 20% is true functional impairment.
So when you use that phrase, they’re not just hearing your words in isolation. They’re hearing them against a background of a dozen residents over the years who used the same words for very different motives.
That’s why the wording matters more than you think.
How Smart Residents Actually Say It
The residents who earn respect and still protect themselves don’t lead with “I’m too tired.” That line is too vague, too loaded, and frankly, too easy to weaponize against you later.
They communicate like colleagues assessing risk, not like trainees asking for permission to rest.
They say things like:
- “I’m starting to make small cognitive errors and I’m worried I’m not safe to perform a new major case. I can assist, but I shouldn’t be the primary.”
- “I’ve been up for 26 hours. I can stay and help with positioning and opening, but for the critical part of the case, you should have someone fresh.”
- “I want to be transparent: I’m at the point where my judgment is off. If we proceed, you’ll need to take the lead.”
You see the difference?
You’re not making it about your feelings. You’re describing your function. You’re explicitly prioritizing patient safety and their leadership.
That framing triggers a different internal response in most attendings:
- “They’re thinking like a surgeon.”
- “They know their limits.”
- “If something goes wrong and this ends up in court, I’m protected because the resident warned me clearly.”
So now you’ve converted your weakness into something that can read as maturity.

| Step | Description |
|---|---|
| Step 1 | Recognize true impairment |
| Step 2 | Assess case urgency |
| Step 3 | Request deferral or swap |
| Step 4 | Offer limited role |
| Step 5 | Use function based language |
| Step 6 | Attending decision |
You’ll notice the key node is “function based language,” not “complaint based language.”
How Your Statement Echoes in the Background
You might think this is a one-off moment. It isn’t. Every attending stores these interactions and they come back up when it matters: evaluations, letters, fellowship calls.
“He’s technically decent but doesn’t have the stamina.”
“She’s smart but checks out when it gets late.”
“They’re very into wellness; I wouldn’t put them in a high-acuity, high-volume environment.”
You’ll never see those exact phrases in your written evals. Instead you’ll see:
- “Will benefit from continued experience managing high-volume workloads.”
- “May require ongoing support in building resilience.”
- “Best suited for a balanced practice environment.”
Those are code. And specialty PDs know exactly what they mean.

| Category | Value |
|---|---|
| High energy resident | 90 |
| Resilient under pressure | 80 |
| Values work life balance | 40 |
| Best in structured settings | 35 |
| Solid 9-5 clinician | 25 |
The top ones are career accelerators. The bottom ones are subtle brakes.
Every time you raise fatigue, your attending is deciding which side of that chart you’re moving towards.
The Line Between Safety and Reputation
Let me be crystal clear: there absolutely are times when you should not be scrubbed in.
When you’re microsleeping on your feet. When you can’t remember the last step you did. When your hands are shaking from sheer exhaustion. I’ve watched that resident drop a needle into a wound and then lose track of it. It happens.
You are not obligated to destroy yourself to satisfy some warped sense of toughness. No case is worth your license or a preventable complication.
But you also don’t get infinite “get out of OR free” cards without cost.
The smartest residents do three things:
They bank credibility early. During your earlier years and on better days, you bust it. Show up. Volunteer. Take call for a sick colleague once in a while. Build a reputation as someone who leans in, not out. Then, when you finally say, “Today I truly cannot,” people believe you.
They separate discomfort from danger. Being tired, grumpy, behind on notes, or missing a meal is miserable but not necessarily unsafe. True impairment is another level. Attend that internal distinction ruthlessly.
They use solutions, not just refusals. “I’m too tired” sounds like you’re handing your problem to the attending. “Given my state, here’s how I can safely contribute, and here’s where you’ll need someone fresh,” sounds like a colleague managing shared risk.
How This Plays Out on a Real Night
Let’s walk through two versions of the same 3:00 AM scenario. Attending is scrubbed on a ruptured appy, you’re the PGY-2, you’ve been up for 26 hours, and there’s a second case pending: a non-perforated cholecystitis that technically could wait but everyone would prefer to get done.
Resident A:
“Honestly, I’m just too tired. I don’t think I can do another case.”
What the attending hears:
I’d rather sleep than learn. Service is your problem, not mine.
They say, “Okay, go home,” but later: “They’re never going to make it through fellowship.”
Resident B:
“I’m at 26 hours, and I can feel my decision-making slowing. For the gallbladder, I’m worried I’d be more of a liability than a help as primary. I can stay to help set up and assist a bit if you want, or we can see if the night float can come down. What do you prefer?”
What the attending hears:
They’re aware. They’re prioritizing patient safety. They’re still willing to help.
They might say exactly the same thing—“Go home”—but the story they tell about you later is totally different.
Same underlying truth (you’re wrecked). Completely different professional signal.
Building a Reputation That Survives Honest Fatigue
You’re not going to outrun fatigue in residency. You can only manage how you’re perceived when it hits.
Here’s what I’ve watched actually work over the years:
You show up early. You know the cases cold. You don’t vanish when something tedious comes up. You don’t constantly bring up duty hours unless they’re actually in danger of violation. When you do ask to leave, it’s with clear reasoning:
- “I’m at 78 hours for the week if I stay for this case, it pushes me over. Happy to stay if we document it, but wanted to flag it.”
- “I’ve been on for 24 hours straight; I’m safe to assist but not to lead a complex lap case.”
You also build informal capital: you cover a shift, you help a co-resident with notes at 5 PM, you stay late for a family meeting and let the attending see it. You’re not doing this to be a martyr. You’re doing it to create a track record.
Because then, when you finally say, “I’m genuinely unsafe to operate tonight,” the attending’s first thought isn’t, “Here we go again.”
It’s, “If they’re saying this, I need to take it seriously.”
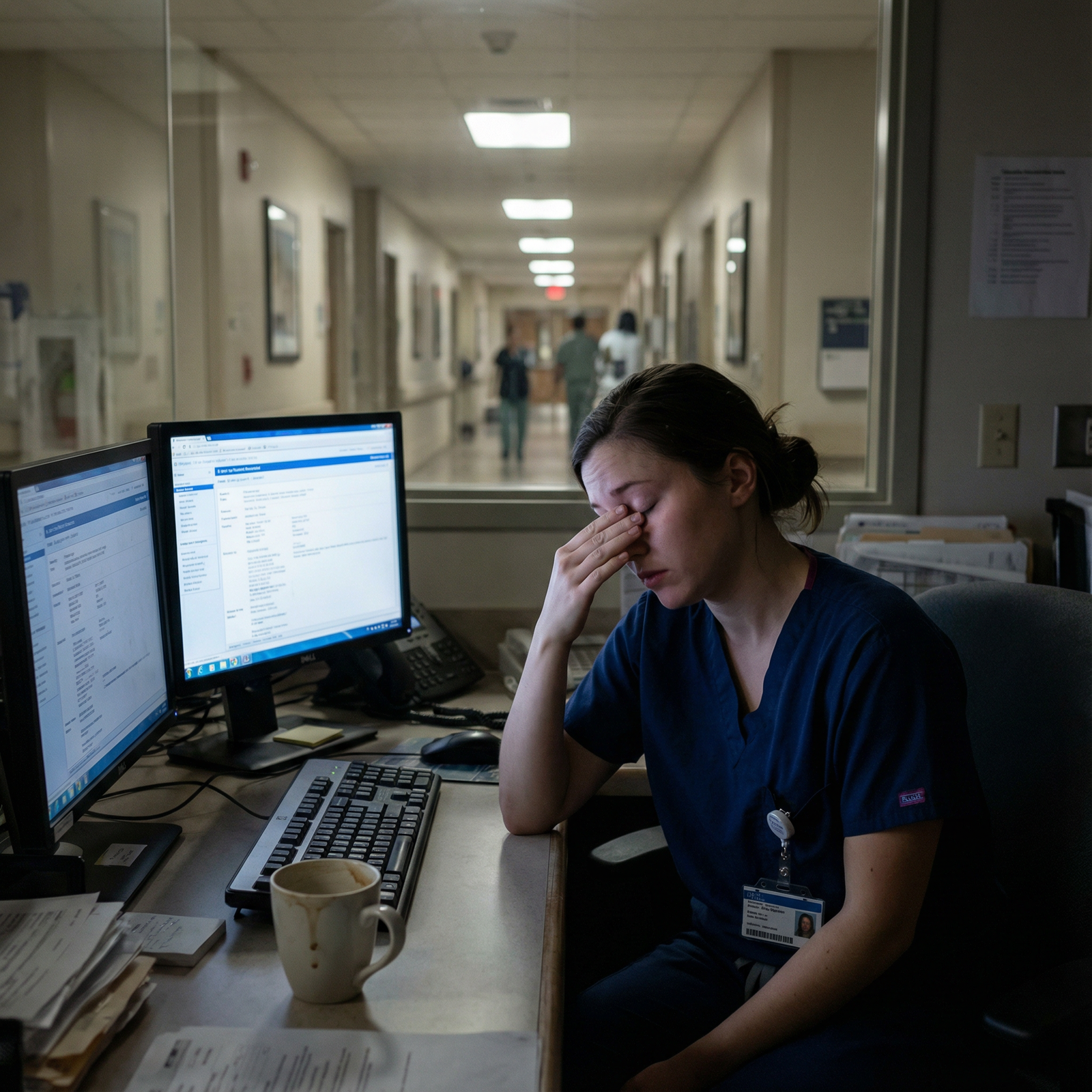
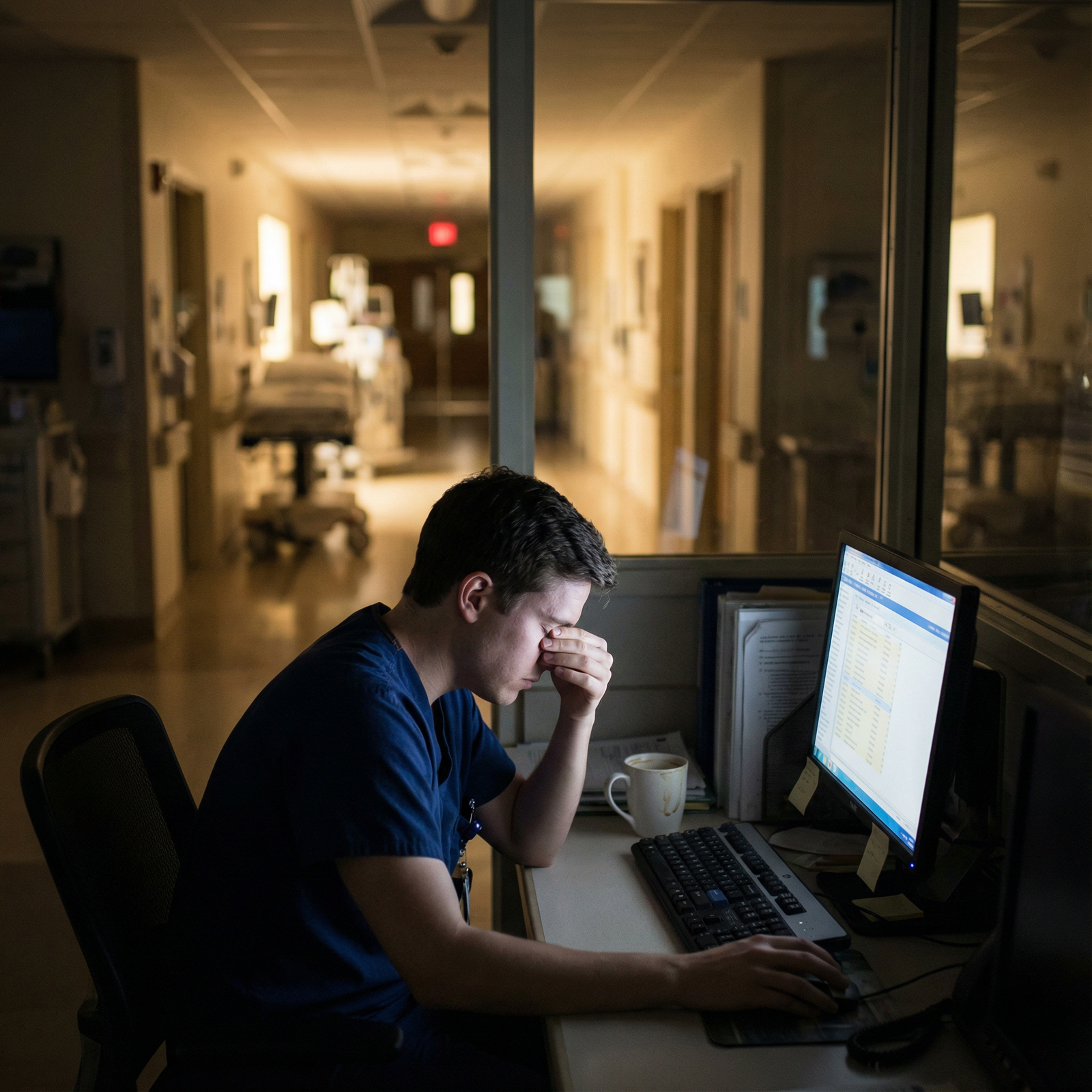
 and duty hours Surgical residents reviewing [call schedule](https://residencyadvisor.com/resources/residency-duty-hours/why-some-chiefs-get-](https://cdn.residencyadvisor.com/images/articles_v1_rewrite/v1_RESIDENCY_LIFE_AND_CHALLENGES_RESIDENCY_WORK_HOURS_residency_program_compliant_work-step2-tired-resident-physician-resting-in-call-8354.png)
Where This Leaves You
You’re walking a tightrope between two risks: harming a patient because you were too proud to speak up, and harming your career because you spoke up poorly or too often.
You will not get perfect at this on day one. But you can be deliberate.
Stop saying “I’m too tired to operate” as a generic complaint.
Start talking like a physician assessing functional capacity and patient safety.
And understand that, like it or not, every attending who hears you is making a judgment that will echo far beyond that one night on call.

FAQ
1. What if my attending ignores my fatigue and tells me to operate anyway?
Document objective facts in a neutral way: “On call since X, last break Y, number of hours worked Z.” Communicate clearly, “I’ve told Dr ___ that I’m concerned I’m not safe to lead this case; I’m available to assist.” If it’s truly unsafe, escalate through chief, program leadership, or the safety hotline. You’re protecting the patient and your license. Do not just silently accept and then complain later.
2. Will speaking up about fatigue tank my evaluations or fellowship chances?
Not if you’ve banked credibility and you speak in terms of function and safety rather than generic complaint. One or two well-framed, justified instances won’t hurt you; a pattern of avoiding work absolutely will. People don’t remember the specific words—you said “I’m unsafe”—they remember the pattern—“they’re always opting out.”
3. How do I know if I’m truly too impaired to operate vs just tired and miserable?
Look for concrete signs: microsleeps despite stimulation, losing track of steps you know well, repeated small errors, struggling to focus on a single conversation, feeling slow to process even simple questions. If you wouldn’t trust someone else in your state to operate on your family member, that’s your answer.
4. Is there any way to repair my reputation if I already got labeled as “too soft”?
Yes, but it takes time and consistency. Stop using fatigue language for anything short of real impairment. Volunteer for a few hard rotations or extra calls. Be visibly prepared and engaged, especially on busy days. Find a supportive attending and ask directly, “I’ve gotten feedback that I seem overwhelmed at night—what would you need to see from me to change that impression?” Then actually do it. People update their stories about you when your behavior changes and stays changed.
Key points: attendings interpret “I’m too tired to operate” through the lens of your prior behavior, their training era, and their risk calculus. You protect both patients and your career by talking about function, not feelings, and by backing that up with a consistent pattern of reliability when you’re not truly impaired.



















