The official night float rules are written for the ACGME inspector. The real rules are written in whispered sign-outs at 7 p.m.
Let me spell out the ones no one explains to you.
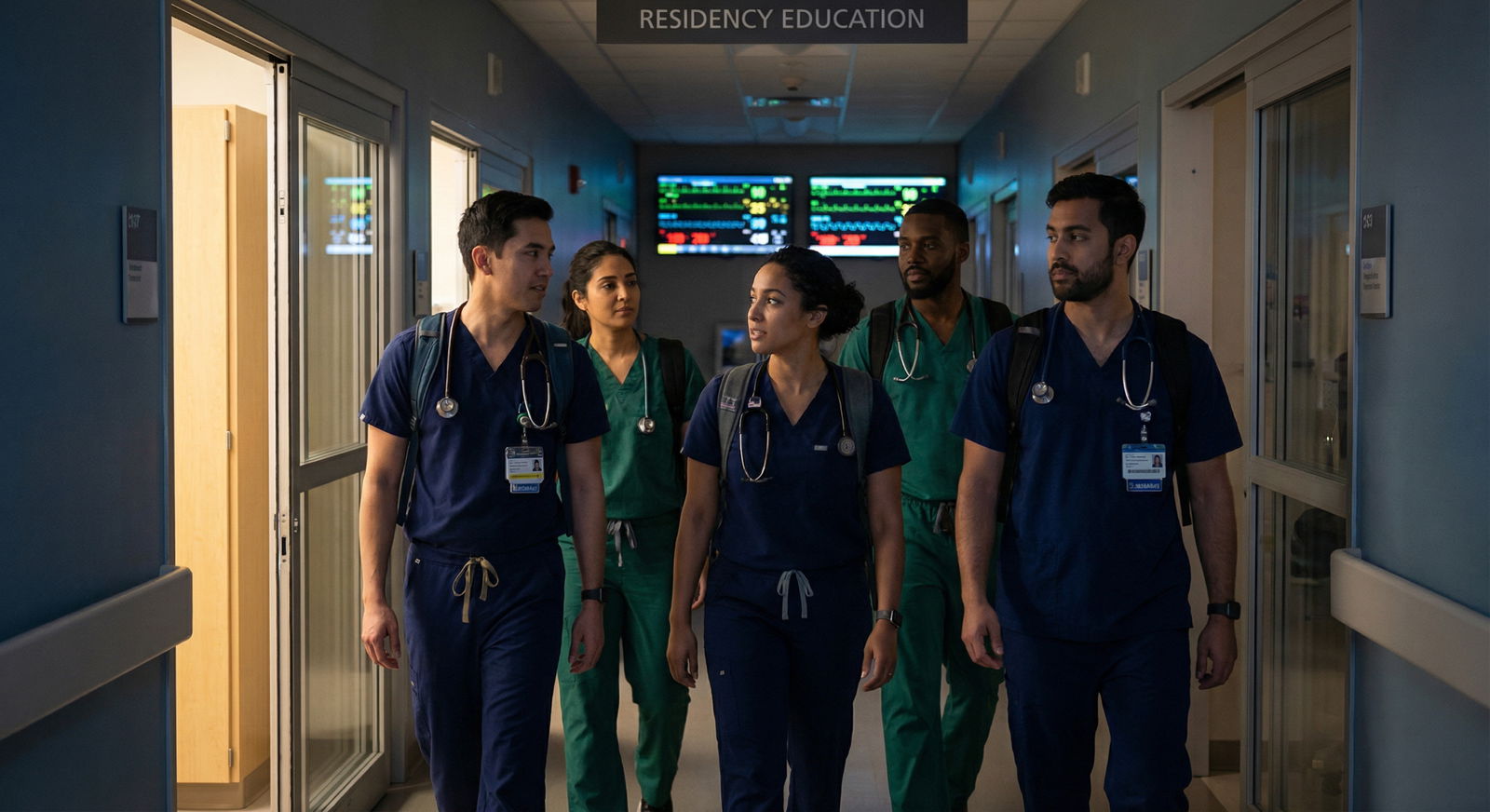
What Night Float Actually Is (From the People Scheduling You)
On paper, night float is a humane alternative to 30-hour calls. In practice, it’s a pressure valve that programs use to keep the daytime service from imploding.
Program directors will never say this on a Zoom town hall, but I’ve heard it in closed-door meetings more than once:
“We’ll push that admit to nights—days are already drowning.”
Here’s how most programs actually think about night float, regardless of specialty:
- It absorbs admits days don’t want.
- It hides staffing gaps from the outside (and sometimes from the GMEC).
- It lets attendings “round fresh” because someone else slogged through the 3 a.m. disasters.
- It’s the rotation most easily abused because the public only sees daytime medicine.
If you understand that framing, the rest of the “unwritten rules” suddenly make sense.

| Category | Value |
|---|---|
| Day Rotation | 60 |
| Night Float | 72 |
Those numbers are conservative. The ACGME caps are one thing. The extra “just stay 30 minutes to help” culture is another.
The Hidden Hierarchy of Night Float
Here’s the dirty secret: not all night float is created equal, and programs know it.

There are three tiers, whether anyone admits it or not:
- Core-service night float (IM, surgery, OB)
- Non-core night float (subspecialty, consults)
- Fake night float (home call dressed up as “night coverage”)
Programs quietly use these to reward or punish.
Core-service night float: the meat grinder
This is the traditional IM or surgery NF: 5–6 nights per week, 2–4 weeks in a row, covering:
- All cross-cover for a big chunk of the hospital
- All new floor/stepdown admits overnight
- Decompensations, codes, transfers, ICU bumps
The unwritten truths here:
- Intern-level night float is often where programs “test” your floor skills under stress. Struggle too visibly here, and people start talking about you at CCC meetings.
- Senior-level night float is where they decide if they trust you alone. Your reputation as “solid” or “dangerous” is often made at 02:30 when no one else is around.
I sat in a CCC once where an associate PD said flat-out:
“Days think he’s fine, but all the codes at night say otherwise.”
That resident never got the letter he wanted for fellowship.
Non-core night float: the “cushion” rotation
Cards, GI, neuro consult nights, etc. Looks brutal in theory. It’s usually more controlled chaos than constant hell.
Unwritten rule: this is where upper levels sometimes get “recovery” months disguised as nights. PDs don’t advertise that, but faculty know who needs a softer block after ICU.
If you see a senior who just finished MICU magically assigned to “Neuro Night Consults” with protected golden weekends? That’s not random. That’s politics.
Fake night float: home-call masquerade
Some programs call it “night float” to make the duty hours math look good, but you’re actually home with a pager:
- Triage calls
- Occasional come-in for OR or deliveries
- A flurry of activity from 11 p.m.–1 a.m., then silence
The real trick here: home call often doesn’t get logged honestly. So your program quietly solves staffing with your sleep. You either push back and become “difficult,” or you play the game and protect your record.
How Coverage Really Shifts at Night (Not What the Policy Says)
Day coverage looks like a brochure. Night coverage looks like a Jenga tower held together by one tired resident and a cross-cover list.

| Step | Description |
|---|---|
| Step 1 | Day Team - 4 Residents |
| Step 2 | Evening Signout |
| Step 3 | Night Float Resident |
| Step 4 | Night Float Intern |
| Step 5 | All Cross Cover |
| Step 6 | Admits and Floor Calls |
| Step 7 | Escalate to On Call Attending |
What actually happens between 6 p.m. and midnight is not what’s written in the coverage grid posted in the workroom.
The “silent load transfer”
Around 4–5 p.m., attendings start off-loading decisions they do not want at 10 p.m.
- Borderline transfer to ICU? “Let’s just give a little fluid and see how they do overnight.” Translation: you decide later and hold the bag.
- Questionable discharge? “Let’s keep them one more night, can be dispo’d by NF in the morning.” Translation: you get to argue with case management at 6 a.m.
By 7 p.m., your list is bigger, sicker, and more fragile than anything the day team had when they rounded at 9 a.m. You signed up to “cover.” You inherited a minefield.
The “sudden attending amnesia”
A lot of overnight work gets done on the assumption that attendings will back you up in the morning. Often they do. Sometimes they don’t.
Real story: Night float intern in IM. Admitted a borderline chest pain from the ED after phone discussion with the attending. Next morning on rounds, same attending says (loudly):
“I’m not sure why this patient was admitted. They clearly could have come to clinic.”
Guess what stuck? Not the phone conversation at 2 a.m. The public shame at 9 a.m.
Unwritten rule: protect yourself with one-line documentation and precise pages. “Discussed with Dr. X at 01:32; plan to admit to telemetry.” You’re not writing for medico-legal reasons at that point. You’re writing to make selective memory harder.
The Real Social Rules of Night Float
No one tells you this at orientation. They should.

Rule 1: You live or die by how efficiently you end sign-out
The fastest way to become hated on both sides: drag sign-out past its expected end time with unfocused questions.
Program directors love to preach “thoroughness.” Residents living on 28 hours of sleep across four days love “get me out of here.”
The real balance:
- Ask targeted safety questions: “Anyone you’re actually worried about tonight?” “Anyone likely to go to ICU?”
- Don’t autopsy the daytime workup. If it’s not life-or-death between 7 p.m. and 7 a.m., it can wait for morning medicine.
Day teams quietly rank night residents by:
- “Safe and efficient”
- “Asks too many questions, slows everyone”
- “Doesn’t ask anything, then freaks out at midnight”
You want the first bucket.
Rule 2: How you present pages sets your reputation
Nurses talk. A lot. And your reputation as “helpful, responsive, not an ass” or “nocturnal disaster” is mostly built by 30-second interactions over the phone.
Unwritten expectations from nursing:
- You answer pages in a reasonable time. Not instantly every time, but also not 25 minutes later when the patient is hypotensive.
- You do not reflexively order “Tylenol and trazodone” to every page about “patient uncomfortable” without at least scanning the chart.
- When they say “I’m really worried about this one,” you actually go see the patient.
Here’s what attendings never tell you: nurses will bring your name up. In huddles. To chief residents. To the nurse manager who “casually” chats with the PD’s spouse at a hospital event.
I’ve watched a resident’s entire persona get rewritten because night shift nurses started calling them “MIA after midnight.”
Rule 3: Senior residents judge you by what you wake them for
There’s a very real invisible metric: “What does this person handle alone, and what do they escalate?”
Wake the senior or attending for everything, and you’re labeled anxious and inefficient. Wake them for nothing, and you’re labeled reckless.
They’ll never give you a checklist for this. So here’s the unsanitized version:
You should be waking people up for:
- New O2 need > 4 L or rapid escalation
- Sustained SBP < 90 in a patient who wasn’t borderline before
- Rapid neuro change, chest pain with concerning features, any new code status discussion
- Anything where you’re about to do something you’d be terrified to defend alone at M&M
You should probably not be waking them up for:
- Mildly high BP in a chronic hypertensive without symptoms
- Insomnia in a 24-year-old
- “Mild abdominal pain” in a constipated, stable patient that hasn’t changed from daytime exam
Key nuance: your threshold changes across the year. An intern calling too much is forgivable. A senior calling for “can I give 5 units of insulin?” is career-limiting.
How Programs Quietly Use Night Float to Test You
Here’s the part they definitely do not say out loud: night float is one of the most data-rich rotations for the Clinical Competency Committee.
Think about it: they see you when you’re tired, unsupervised, and constantly triaging.
| Night Behavior Pattern | CCC Interpretation |
|---|---|
| Never calls for help | Judgment / safety risk |
| Calls for every minor issue | Lacks confidence / skill |
| Frequent overnight ICU bumps | Weak floor management |
| Smooth sign-outs, few escalations | Ready for senior role |
| Nurse complaints about coverage | Professionalism concerns |
I’ve watched this exact table, almost word-for-word, come up behind closed doors.
Specific unwritten evaluations they make based on NF:
- Can you prioritize? If your ICUs are full and you still manage to avoid codes, that’s noticed.
- Do you panic? Attendings know what “it was crazy” actually means when they look at the numbers the next day.
- Are your notes coherent at 4 a.m.? They skim them. They can see your brain unravel across the night.
This is why certain residents mysteriously get more night float than others. Sometimes it’s random. A lot of the time it’s, “We need more data on them in an unsupervised setting.”
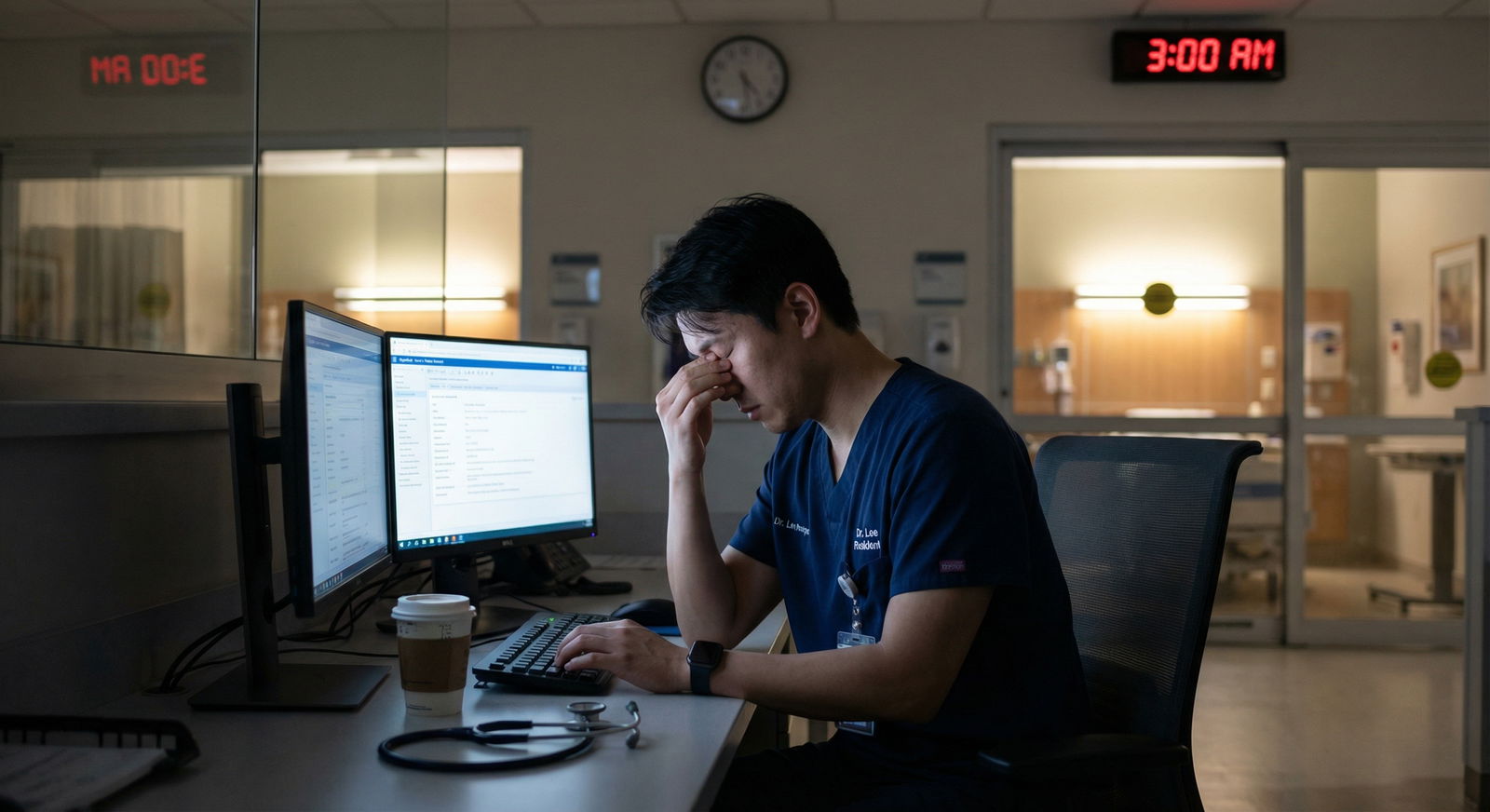
The Real Physiology and Time Distortion of Night Float
The wellness lectures about sleep hygiene do not touch what happens on week 2 of a straight night block when your circadian rhythm is wrecked and your empathy is on a delay.

| Category | Value |
|---|---|
| Night 1 | 80 |
| Night 3 | 65 |
| Night 7 | 50 |
| Night 10 | 40 |
| Night 14 | 35 |
Those numbers are pulled straight out of resident self-reports I’ve seen on anonymous surveys. And they match what I’ve watched on the wards.
What you don’t hear in orientation:
- Your tolerance for nonsense plummets. A family calling at 3 a.m. to ask for “something to help him sleep” will provoke an internal rage you didn’t know you had.
- Your threshold to snap at people drops. That one sarcastic remark to a nurse who pages you for the third time in 20 minutes? It will be remembered. You were on night 12. They don’t care.
- Your clinical intuition dulls slightly around 4–5 a.m. That’s exactly when the worst stuff happens.
The insider adjustment residents figure out by the second block:
You must pre-plan your vulnerable hours.
If you know you’re a zombie between 3–5 a.m., you:
- Pre-round on anyone even slightly shaky by 2 a.m.
- Set mental red flags: “If any vitals change on these three patients between 3 and 5, I’m going to the bedside, no arguing.”
- Force yourself to put eyes on sick patients even when your brain screams “just reorder labs and go back to the call room.”
No one writes this in a handbook. But the residents who do not understand their “danger window” are the ones who rack up avoidable disasters.
Time Management: The Unspoken Triage Game
At night float, you are not really managing medicine. You are managing queue theory.

| Step | Description |
|---|---|
| Step 1 | New Page |
| Step 2 | Go to bedside now |
| Step 3 | Handle within 10 min |
| Step 4 | Batch for later |
| Step 5 | Phone order or defer |
| Step 6 | Life threat? |
| Step 7 | Time sensitive? |
The seniors who look like wizards at night are just ruthless about one thing: they never treat all pages as equal.
Unwritten techniques they use but rarely articulate:
- They mentally queue tasks into “now, soon, or never.” “Never” really means “this is morning work disguised as night work.”
- They sort pages by floor geography. If they’re going to 7 West for a rapid, they’ll swing by 7 East to eyeball the chronically hypotensive patient they’ve been worried about—before the nurse even calls.
- They consciously protect 30-minute blocks for admits. They do not let themselves get nibbled to death by order entry while trying to sort out a septic patient.
New night residents drown because they try to resolve each page to completion in the order received. That’s how you end up writing a full insomnia note while someone else’s patient’s lactic acid climbs quietly from 2.5 to 5.8.
Politics Around Swapping, Complaining, and “Taking One for the Team”
You cannot talk about night float without talking about the politics of coverage.
Here’s what’s really happening behind the assignments:
- Chiefs are balancing service needs, fairness, and who’s already on their “problem list.”
- PDs care more about avoiding duty-hour violations and disasters than your birthday plans.
- Residents are constantly trying to trade into or out of specific blocks for life events.
The unwritten social rules:
- If you always say no to swaps that benefit others but expect everyone to save you before your wedding, people notice.
- If you volunteer occasionally for a bad NF block to help a co-resident in crisis, chiefs remember. That can pay you back later in more subtle scheduling favors.
- Chronic complaining about nights, especially in front of attendings, gets you labeled as “fragile.” That word comes up in ranking and fellowship letters a lot more than anyone admits.
I’ve watched a PD cross a resident off a chief shortlist after one too many “I can’t believe I have to do another night shift” comments during a faculty meeting week.
Complain strategically:
- Upward (to leadership) only when you can tie it to safety, not your comfort.
- Laterally (to peers) sparingly—everyone’s miserable. You’re not unique.
- Never about specific nurses or staff in emails. Those get forwarded. Often.
Documentation and Cover-Yourself Moves People Learn the Hard Way
No one sits you down and explains how to protect yourself on NF when things go bad at 3 a.m. So residents either over-document (paralyzed) or under-document (exposed).

Unwritten best practices that I’ve seen save careers later:
- One-liner after major phone calls: “Discussed with Dr X at 02:17, agrees with plan to…” You’re not being paranoid. You’re anchoring the story.
- Explicit stability statements: “At time of evaluation, patient hemodynamically stable on 2 L NC, no increased work of breathing.” When the code happens at 6 a.m., this matters.
- Time stamps that make sense. If your note says you examined the patient at 03:05 and the rapid was called at 03:06, people will ask questions.
Also: know when not to write a novel. If you clutter the chart with 35-word salad notes about “patient comfortable, no acute distress,” no one can see the one actually important entry.
FAQ: The Things You’re Asking Yourself But Won’t Say Out Loud
How much should I actually wake the attending overnight?
More than the most macho senior tells you, less than your 3 a.m. anxiety wants. If you’re making a decision that could plausibly show up in M&M—ICU transfer, major change in code status, refusal of critical care, unexpected rapid deterioration—you call. If it’s a borderline admit vs discharge and you’re truly torn, call. If you’re mostly seeking emotional reassurance about a stable patient, write your assessment clearly and let days clean it up.
Is it career-damaging to say night float is killing me?
Only if you say it the wrong way, to the wrong audience, over and over. If you frame it as, “I’m worried we’re unsafe with one resident covering 80 patients and six admits a night,” leadership may actually respect that. If you frame it as, “This is unfair, I’m tired, other programs do it better,” you’ll be filed under “complainer.” Same feeling. Different packaging. Very different consequences.
What’s the single biggest mistake new residents make on night float?
Treating every page as identical and reacting in chronological order. That’s how you burn out, miss the real emergencies, alienate nurses, and look disorganized when attendings review the night. The residents who thrive learn to instantly sort pages into “must see now,” “can fix from the computer,” and “morning problem disguised as night problem.” That triage skill is the real curriculum of night float—everything else is just service.
If you strip away the glossy talk, three things remain:
- Night float is where your judgment, not your textbook knowledge, gets tested and remembered.
- How you manage people—nurses, attendings, co-residents—matters as much as how you manage patients.
- The system will not protect you by default. You have to learn the unwritten rules, or you end up learning them the hard way at 3 a.m. with your name in the morning email.



















