
Night float was sold as a safety intervention. In practice, it’s mostly a scheduling trick with mixed consequences that nobody wants to admit.
You’ve heard the script: long 24–30 hour calls are dangerous, residents are zombies after midnight, and patients deserve “rested” doctors. So programs cut traditional call and installed night float systems—shorter shifts, more handoffs, more “protected” days.
The problem? The evidence that night float meaningfully improves patient safety is weak, inconsistent, and in some settings, flat‑out negative. We traded one set of risks (fatigue) for another set (fragmentation and handoffs) and then pretended the trade was obviously better.
Let’s walk through what the data actually show, and what it means for you grinding through residency nights.
How We Got Here: The Myth of “Fatigue Fixes Everything”
After the Libby Zion case and the 2003 ACGME duty-hour rules, residency programs scrambled. The narrative hardened quickly: long shifts equal dangerous errors. Shorter shifts equal safety.
So they pushed three big ideas:
- Cap weekly hours (80-ish).
- Cap continuous work hours.
- Use night float to “cover” nights without 30‑hour calls.
On paper, night float sounds like progress. A resident works, say, 6–7 pm to 7–8 am for several nights in a row, then has days to recover. Continuity of nights but limited duration per shift. Fewer marathon calls. More days off post‑nights. Everybody wins, right?
Except you do not magically remove fatigue by rearranging it. You just move it, compress it, and add new failure points.
What the early research actually found
Look at the big, influential trials and reviews, not the rosy summaries at GME town halls.
The FIRST trial (surgery) and iCOMPARE trial (internal medicine) looked at flexible vs more restricted duty hours (which usually involved more night float / shift-like setups). They didn’t find the big safety wins people expected:
- No improvement in 30‑day mortality.
- No consistent reduction in complications.
- No clear reduction in readmissions or major adverse events.
Residents were not suddenly better-rested and flawless. They were differently tired, often more fragmented, and dealing with more cross‑coverage.
Fatigue matters. But the fantasy was that cutting continuous hours was a one-way street to safer care. It isn’t.
The Hand-off Problem: Night Float’s Dirty Secret
If there’s one thing night float absolutely increases, it’s the number of handoffs. That’s not controversial. That’s math.
Every transition is an opportunity to lose information. And we are terrible at admitting how much gets lost.
I’ve watched this play out on sign-out:
- “Bed 6 has some abdominal pain, CT pending, probably appy, surgeon aware.”
- Fast-forward 6 hours. The CT comes back ugly, but the night float has never met the patient, the note is vague, and the surgeon is “aware” in theory but scrubbed in another case. The night resident is deciding between wake-everyone-up vs wait-an-hour.
The literature on handoffs is remarkably consistent: more handoffs → more communication errors. The I-PASS study showed structured handoffs can reduce medical errors, which is great, but look carefully at what that implies. They had to build an entire system to compensate for the risk we introduced by cracking continuity apart.
Night float inflates:
- The number of times a plan changes hands.
- The number of cross‑cover patients one resident “knows” only through a 60‑second summary.
- The chances that a “soft concern” in someone’s gut disappears in translation because it never made it into Epic.
This isn’t theoretical. There are multiple observational studies showing that increased handoffs are associated with more preventable adverse events. The effect isn’t huge in every dataset, but it’s not trivial either.
You reduced one kind of error (extreme fatigue) and injected another kind (handoff failures). The net result? Much closer to neutral than the pro‑night‑float narrative suggests.
Fatigue: Still There, Just Distributed Differently
Night float doesn’t eliminate fatigue; it rearranges your circadian wreckage.
Here’s the misconception: “Shorter shifts at night mean you’re less tired.” No. Shorter continuous shifts at the wrong circadian phase can be just as impairing.
You’re still:
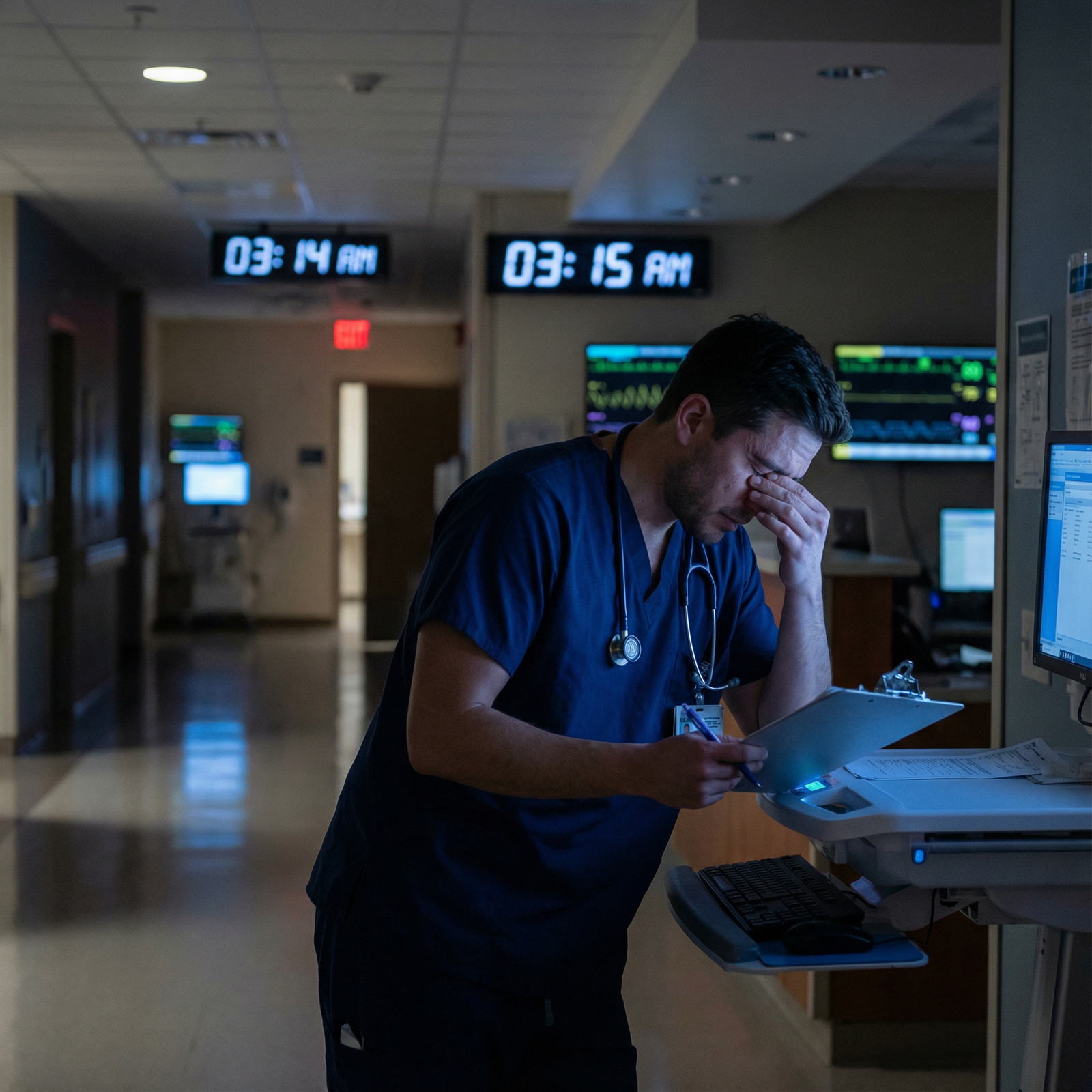
- Working in the biological low (2–6 am) when cognitive performance drops.
- Sleeping at abnormal times, often poorly, with daytime noise and light.
- Flipping between day and night schedules in quick succession.
Sleep research is ruthless on this point: circadian misalignment can impair alertness and decision-making as much as total sleep deprivation. You can get a theoretical 7 hours of daytime sleep and still function like you’re half-drunk at 3 am.

| Category | Value |
|---|---|
| 09:00 | 1 |
| 13:00 | 1.1 |
| 17:00 | 1 |
| 21:00 | 1.2 |
| 01:00 | 1.5 |
| 05:00 | 1.8 |
So when a hospital brags about “safer nights” because nobody is working 28 straight hours anymore, remember:
- The absolute worst cognitive performance still happens overnight.
- Night float residents often stack multiple nights with inadequate daytime recovery.
- There’s solid evidence that rotating shifts hammer mental health, reaction time, and mood.
You are less likely to be completely shattered at noon post‑call. But at 4:30 am on your fifth night in a row? You’re not a beacon of clarity.
The stronger claim—that night float makes care meaningfully safer across the board—just isn’t supported.
What the Big Trials and Reviews Actually Say
The duty hour discussion often gets hijacked by feelings and anecdotes. Let’s anchor in data for a minute.
| Study | Specialty | Intervention | Patient Mortality Change | Resident Sleep/Wellbeing |
|---|---|---|---|---|
| FIRST | Surgery | Flexible vs restricted | No significant difference | Similar overall |
| iCOMPARE | IM | Flexible vs standard | No significant difference | Small mixed changes |
| Meta-analyses | Mixed | Shorter vs longer shifts | Inconsistent, mostly neutral | Slight sleep gains but shift-related issues |
The punchline from large, reasonably designed studies:
- No consistent improvement in hard safety endpoints (mortality, major complications).
- Some modest benefit in self-reported sleep and burnout in some subgroups, but not across the board.
- No slam-dunk evidence that shorter shifts + more night float is a major safety upgrade.
There are smaller studies suggesting benefits for certain processes (like fewer serious errors in interns under specific shorter shift regimes), but they usually come with tradeoffs: more handoffs, more fragmentation, worse continuity.
The honest conclusion: night float is not a magic safety tool. At best, it’s safety-neutral when implemented well, and harmful when implemented lazily.
Continuity, Ownership, and the “Who Actually Owns This Patient?” Problem
Traditional call had an obvious downside: crushing fatigue. But it had a hidden strength. Ownership.
You admitted the patient, you knew the nuance, you watched them decompensate at 2 am, you rounded on them the next morning. The story stayed in one head. Or at least in one small team.
Night float shatters that ownership:
- Day team admits, crafts a plan, then disappears.
- Night float covers dozens of patients they’ve never met.
- Complicated overnight event? The person who learns the most about it often goes home before the attending ever hears their side in detail.
I’ve seen this countless times on rounds: Day team: “Overnight the patient had some tachycardia, but it resolved.” Attending: “What did it get to? What triggered it?” Day intern: “Not sure, note says ‘self-resolved’.”
That gap isn’t laziness. It’s structural. The night resident handled it but is now asleep. The nuance is gone. The plan is now based on a watered-down secondhand version of a critical event.
Continuity matters for pattern recognition. For that “something’s off” feeling that doesn’t fit into a checklist. You can’t fully replace that with a meticulously formatted sign‑out.
Resident Education and Skill Development: Collateral Damage
We’re allegedly training physicians, not just staffing a 24/7 service. Night float tends to erode a few key elements of real training.
Fewer complete arcs of care
Admitting, managing, and seeing the early outcomes of your decisions is how judgment forms. With night float:
- Night residents admit but rarely see past day 1–2.
- Day residents inherit complex cases they didn’t evaluate at the critical decision point.
- Complications that arise at 3 am are managed by someone who will never follow that patient longitudinally.
That’s not “learning the natural history of disease.” That’s plugging leaks on a sinking ship and never seeing how the story ends.
Procedural and cognitive atrophy
Certain skills—airway, acute sepsis management, stroke codes—cluster at night. If nights are covered by a small fixed set of night float residents, others simply see fewer high-acuity events.
Intern A on q4 call: lots of chances over the year to lead codes, push levophed, call ICU. Intern B who dodges most nights due to scheduling quirks: vastly fewer reps.
Night float can create uneven exposure depending on how rotations are built. And when you staff nights with your “strong” or “experienced” residents to keep the place safe, you widen that gap.
The Mental Health Cost Nobody Really Counts
Programs sometimes point to “less 30‑hour call” as a resident wellness win. That’s only half the story.
Rotating night shifts, even “soft” ones like night float, are brutal on:
- Mood and anxiety
- Sleep quality
- Social life and relationships
- Physical health markers (metabolic, cardiovascular risk)

| Category | Value |
|---|---|
| Traditional Call | 65 |
| Mixed Call + Night Float | 60 |
| Heavy Night Float | 72 |
That hypothetical chart is not an exaggeration. Studies of resident burnout often show:
- Overall high burnout regardless of system.
- No consistent “win” for night float.
- Sometimes higher depersonalization among those with heavy night responsibilities.
You feel less shattered after a single night float than after a 28‑hour call. But after 6–7 nights in a row when you haven’t seen sunlight in days and your friends’ lives are happening between 5–9 pm while you’re already back in the hospital? Different kind of damage.
So Does Night Float Improve Patient Safety?
If you want the unvarnished answer: not reliably, and not by nearly as much as it’s advertised. The benefit is context‑dependent, implementation‑dependent, and often offset by handoff risks and circadian issues.
Where night float can help:
- In services where old-school calls were routinely exceeding 30 hours and residents were dangerously impaired by late morning.
- When combined with rock-solid handoff processes (I-PASS or equivalent), smaller cross‑cover pools, and real attention to circadian science.
- When schedules avoid constant flipping between days and nights and give adequate recovery time.
Where night float can hurt:
- In highly complex services where continuity and longitudinal understanding of patients matter a lot (oncology, transplant, advanced heart failure).
- When night residents are covering absurd numbers of patients they don’t know, with vague sign‑outs and no real backup.
- When programs treat “night float = problem solved” and stop thinking about fatigue, staffing, or support.

The question you should be asking isn’t “night float or traditional call, which is safer?” The real question is: “How do we design coverage that balances fatigue, continuity, supervision, and handoffs in this environment, with these patients?”
Night float is one tool. Not a panacea.
If You’re Stuck in a Night Float System: How to Reduce the Damage
You do not control the schedule. But you absolutely influence how safe nights are for your patients—and how survivable they are for you.
A few high-yield moves, based on what actually mitigates risk:
Treat handoffs as patient care, not paperwork. Slow down. Flag three things clearly: who is unstable or “worrying,” what time‑critical results are pending, and what to do if X happens. Yes, you’re tired. This is where most preventable errors hide.
Shrink your personal chaos. Night float is cognitively expensive. Use checklists, sticky notes, or a personal system so pending tasks don’t live only in your fried working memory at 4 am.
Fight for real recovery. Blackout curtains, phone off, eye shades, no “I’ll just answer a few messages” after a shift. Partial sleep plus constant interruptions is the fastest way to show up on night 4 in cognitive debt.
Pull attendings and seniors in early for borderline calls. You’re working in a system that already trades information quality for coverage. Do not compound that with ego or fear of “bothering” people.
These things matter more than whatever branding your program slaps on its call schedule. The structure sets the baseline risk; your habits determine whether that risk explodes or stays controlled.
The Real Myth
The biggest myth isn’t that night float is evil or perfect. It’s that schedule design alone can guarantee safety.
It cannot.
You can make residents slightly less acutely sleep‑deprived and simultaneously:
- Increase communication failures.
- Dilute ownership.
- Undermine training.
- Worsen circadian disruption.
Or you can design a hybrid system: fewer extreme calls, thoughtfully implemented nights, disciplined handoffs, adequate staffing, and supported residents. That’s where the real gains are.
One final image for how this really works:

| Step | Description |
|---|---|
| Step 1 | Night Float Implementation |
| Step 2 | Reduced continuous hours |
| Step 3 | More handoffs |
| Step 4 | Shifted circadian load |
| Step 5 | Less extreme fatigue |
| Step 6 | Greater info loss risk |
| Step 7 | Persistent performance dips at night |
| Step 8 | Potential fewer fatigue errors |
| Step 9 | More communication errors |
| Step 10 | Mixed safety impact |
That mess in the diagram? That’s reality. Not the clean, feel-good story.
The Bottom Line
Night float does not consistently improve patient safety in a meaningful way; at best, it trades fatigue-related risks for handoff and continuity risks and comes out roughly neutral in many studies.
The details of implementation—handoff quality, patient volume, supervision, circadian design—matter far more than the buzzword on the schedule.
If you are living the night float life, your biggest levers for safety are excellent sign-outs, early escalation for borderline cases, and ruthless protection of your own sleep and cognitive bandwidth.




















