
What happens if you’re the last resident on the floor every single night… and people start to notice?
Because that’s the nightmare loop, right?
You’re slow. Everyone else finishes. You’re still charting at 8:30 pm while the rest of the team is already at dinner or home. Attendings think you’re incompetent. Co-residents think you’re dead weight. Program director thinks, “liability.” You think, “Did I make a huge mistake going into medicine?”
Let’s walk straight into that fear instead of pretending it’s not there.
The Ugly Truth: Yes, Some Residents Really Are Slower
Let me say the thing you’re scared to say out loud: yes, there are people who are slower than average in residency.
Not imaginary slow. Not “I’m hard on myself” slow. Actually staying 1–3 hours later than everyone else, consistently.
I’ve seen:
- The intern still writing H&Ps at 9 pm on wards while everyone else left at 6:30.
- The EM resident who needs 40+ minutes to dispo one patient because they’re triple-checking everything.
- The ICU resident still finishing progress notes while night float is already pre-rounding.
So no, you’re not uniquely broken if that’s you.
But here’s the important part: “slow” doesn’t automatically mean “bad resident” or “doomed career.”
Sometimes “slow” means:
- You’re early in the year and still building pattern recognition.
- You’re extra meticulous because you’re terrified of missing something.
- You’ve never been taught good workflow, so you brute-force everything.
- Your service is understaffed, your patients are complex, or your documentation burden is insane.
And yes, sometimes “slow” means you have real efficiency issues that you do need to fix.
The key question isn’t: "Am I slower than others?"
The question is: "Am I stuck, or am I improving?"
What Programs Actually Care About (Spoiler: Not That You Stay Late)
Here’s the thing programs do care about:
- Are you safe?
- Are you teachable?
- Are you improving over time?
- Are you burning out or breaking down?
They don’t sit in conference and go, “So, who’s slower than average?” They talk about the intern who can’t keep up and then gets defensive when given feedback. Or the one who makes the same mistake 5 times. Or the one so overwhelmed that they’re missing critical tasks.
Staying late by itself doesn’t trigger “remediation meeting.”
Being unsafe, disorganized, or unaware does.

| Category | Value |
|---|---|
| Safety | 90 |
| Efficiency | 70 |
| Professionalism | 60 |
| Knowledge Gaps | 65 |
Notice how “efficiency” isn’t at the top. Patient safety and reliability are.
I’ve heard attendings say stuff like:
- “Yeah, she’s slow, but she cares, and she’s getting faster.”
- “He stays late, but his notes are good and his patients are always followed up on.”
- “I’m more worried about the fast guy who misses things than the slow one who’s meticulous.”
Nobody likes a system where you stay late every day. But people will tolerate “slow but safe” a whole lot longer than “fast but sloppy.”
So if you’re thinking, “If I don’t magically transform into a machine by October, I’m getting fired,” that’s not how this works. Terminating a resident is rare and dramatic. Programs bend over backwards to support improvement before they go nuclear.
The Emotional Spiral: Shame, Comparison, and Silent Panic
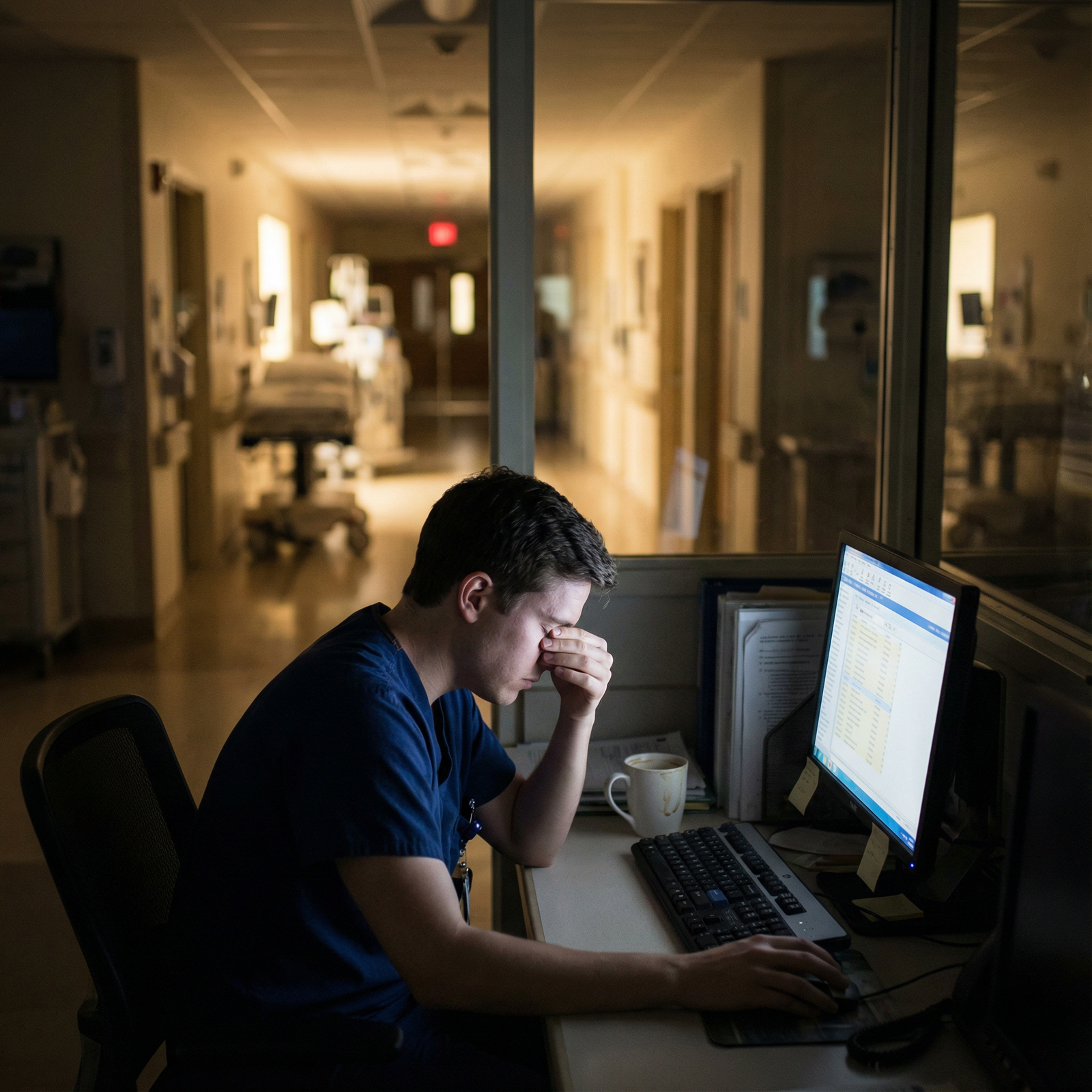
Let’s be honest about the emotional part, because that’s what’s really killing you.
You stay late. Everyone else is gone. Chairs are empty. The workroom is quiet. Cleaning staff rolls the trash can through. You’re still typing.
You start thinking:
- “They all finished. Why can’t I?”
- “I must be dumb.”
- “They’re talking about me.”
- “I’m going to fail this rotation.”
- “I’m going to fail residency.”
The shame is heavy. It makes everything worse because:
- You double-check more, out of fear -> that makes you slower.
- You hesitate to ask for help -> that makes you slower.
- You ruminate instead of acting -> that makes you slower.
You start hiding how long you’re staying. You stop talking about it. You quietly close notes after hours at home. You pretend you’re fine. That’s where people actually get into trouble. Not because they were slow. Because they went silent and isolated.
If this is you, I want you to name it clearly in your own head: “I’m not lazy. I’m scared.”
Those are very different problems.
Where Being Slow Does Start to Hurt You
Let me not sugarcoat this: there is a point where slowness becomes a real problem.
Red flags:
- You routinely hand off major incomplete tasks because you ran out of time.
- Nurses are regularly paging night float about stuff you “were going to get to.”
- Your notes are so late they’re basically historical documents.
- Consultants complain they can’t find updated documentation.
- You miss conferences because you’re always “catching up on notes.”
That’s when faculty start to think: “This isn’t sustainable. Is this a knowledge issue? Workflow? Something else?”
Your program has a duty-hour cap on paper, but everyone knows residents stretch. The concern isn’t “you stayed 13 hours once.” The concern is “you’re at 14–15 hours every single ward day, and you look like you’re about to collapse.”
There’s also a perception problem if you look disorganized all the time:
- Juggling papers
- Forgetting your list
- Not knowing your patients’ basic info when asked
- Constantly saying “let me check” on simple questions
That doesn’t necessarily mean you’re truly worse; it just feeds the narrative in people’s heads. And narratives stick.
So no, you’re not insane for worrying. There is a point where being consistently much slower than your peers becomes something that needs active attention, not just “it’ll get better on its own.”
What Being “Faster” Actually Means in Residency (It’s Not Just Typing Speed)
People think “fast” means “I can write notes quickly.” That’s a tiny part of it.
Residents who look fast usually have:
- Pattern recognition: They’ve seen similar cases, so they’re not reinventing the wheel.
- Aggressive prioritization: They know what’s urgent vs what can wait.
- Parallel processing: They start orders while evaluating, not after everything’s done.
- Lower anxiety: They’re not mentally catastrophizing every single decision.
- Shortcuts: Smart phrases, pre-built templates, streamlined exam, solid signout format.
A lot of your “slowness” might just be bad workflow and sky-high anxiety, not incompetence.
Example: Two interns with the same census.
Intern A:
- Sees all patients first, writes nothing down, then tries to remember everything later.
- Writes each note from scratch each time.
- Calls consultants at the end of the day.
- Checks labs only once, at the very end.
Intern B:
- Pre-charts key vitals/labs before seeing patients.
- Uses smart phrases/templated structure.
- Orders stuff as they go.
- Calls consults early, then finalizes the plan after.
- Updates signout as they go, not at 6 pm.
Guess who goes home first? It’s not because Intern B is “smarter.” It’s because their system doesn’t fight them.

Concrete Ways to Stop Being the Last One Out (Without Selling Your Soul)
You’re not going to magically become a speed demon overnight. But you can stop being that person who’s hours behind everyone, every single day.
Here’s how, in a way that doesn’t require pretending you’re not anxious.
Ask directly for workflow feedback, not “general” feedback.
Instead of: “Am I doing okay?”
Try: “I’m consistently staying 1–2 hours later than my co-residents. Can you watch my workflow for a bit and tell me where you think I’m losing time?”Shadow a faster co-resident for 30–60 minutes.
Literally watch how they:- Structure prerounds
- Take notes in the room
- Place orders
- Dictate/write notes
Then steal shamelessly. Everyone I’ve seen make a big leap in efficiency copied someone else’s system.
Front-load the day.
Do the heavy lifts early:- Pre-chart before touching a patient.
- Put in obvious orders early (labs, imaging, consults).
- Call social work / case management before noon, not at 4 pm.
Time-box yourself.
This is huge if you’re anxious:- “I get 7 minutes per preround patient.”
- “I get 25 minutes to write this note.” When the time hits, you move on even if it’s not perfect. Perfection is a luxury you don’t have.
Build ruthless templates.
Make smart phrases that:- Pull in objective data automatically
- Have standard assessment/plan outlines for common problems (CHF, COPD, sepsis, etc.)
Then you just tweak, not compose from scratch every time.
Ask seniors to help you triage your list.
Example: “Here’s my to-do list. If this were your day, what order would you do these in?”
You’re not just asking for help—you’re learning how they think.

| Step | Description |
|---|---|
| Step 1 | Pre-chart labs and vitals |
| Step 2 | Preround on patients |
| Step 3 | Enter obvious orders early |
| Step 4 | Call consults and services |
| Step 5 | Write and sign notes |
| Step 6 | Update signout list |
| Step 7 | Check for loose ends |
When You Should Actually Talk to Someone (And What to Say)
If you’re consistently:
- Going over duty hours
- Crying in the car on the way home
- Dreading every shift because you can’t keep up
- Feeling physically sick seeing your patient list in the morning
you’re past “I’ll figure this out on my own.”
You talk to:
- A trusted senior resident
- Your chief
- An APD or PD you don’t hate
- Or even GME / mental health support if it’s that bad
You don’t go in with, “I’m failing, help.”
You go in with something like:
“I’m consistently staying 1–3 hours later than my colleagues to finish notes and follow-up tasks. I’m worried this means there’s something wrong with my efficiency, not my work ethic. I want to improve, but I’m not sure what I’m doing wrong. Can you help me identify specific things to work on, or connect me with someone who can?”
That sounds teachable, self-aware, and motivated. Not like a meltdown. Programs love that.
Worst-case scenario in your head: “They’ll think I’m incompetent and put me on probation.”
Realistic scenario: “They’ll say they’ve noticed I’m slow, they’re glad I came forward, and they’ll help create a plan.”
The Part You’re Afraid to Ask: Could I Actually Get Kicked Out for This?
Can being slow get you dismissed from residency?
By itself? Almost never.
Residents typically get removed when there’s a pattern:
- Clinical safety issues
- Repeated failure to respond to feedback
- Professionalism problems (lying, disappearing, hostility)
- Major knowledge deficits that don’t improve despite support
Being slower than your co-residents is usually a symptom, not the diagnosis.
If you’re:
- Showing up on time
- Owning your patients
- Responding to feedback
- Actively working on your workflow
- Honest when you’re struggling
then “slowness” becomes a developmental issue, not a character indictment.
The resident who’s at risk is the one who:
- Gets feedback about efficiency and gets defensive
- Blames everyone else
- Hides their struggles
- Keeps making the same mistakes
- Shows no change over months and months
So if you’re sitting here overthinking this article and worrying that you’re falling behind—that alone almost guarantees you’re not in that last category.
A Quick Reality Check on Co-Resident Comparison
One more thing: you’re probably comparing your worst day to someone else’s best day.
- The fast PGY-2 on wards? They were drowning as an intern.
- The EM senior dispo-ing patients in 5 minutes? They once stayed 3 hours late every shift.
- The ICU fellow who “never sits”? They used to double-chart everything out of fear.
You just don’t see that version of them.
| What You See | What’s Usually True |
|---|---|
| Co-resident leaves at 5 | They stayed late all intern year |
| Attending fast on rounds | 10+ years of pattern recognition |
| Senior never flustered | They had panic attacks as a PGY-1 |
| You always last to leave | You’re earlier than last month |
You’re in the part of the story where it feels awful and embarrassing and endless. It’s not the whole story.
If You Remember Nothing Else
Keep three things in your head:
- Being slower than your co-residents doesn’t mean you’re a bad doctor; it means you’re either early, anxious, disorganized, or all three—and all of those are fixable.
- Programs care more about safety, improvement, and honesty than raw speed. You get in trouble for being unsafe and unresponsive, not for staying an extra hour to finish your notes.
- Silence is what sinks you. If you’re consistently staying late, talk to someone, get specific workflow help, and treat this like a skill you can learn—not a permanent flaw you have to hide.
You’re not the only one who’s stayed under those fluorescent lights long after everyone else went home. The question isn’t whether you’re behind. It’s whether you’re willing to let people help you move forward.



















