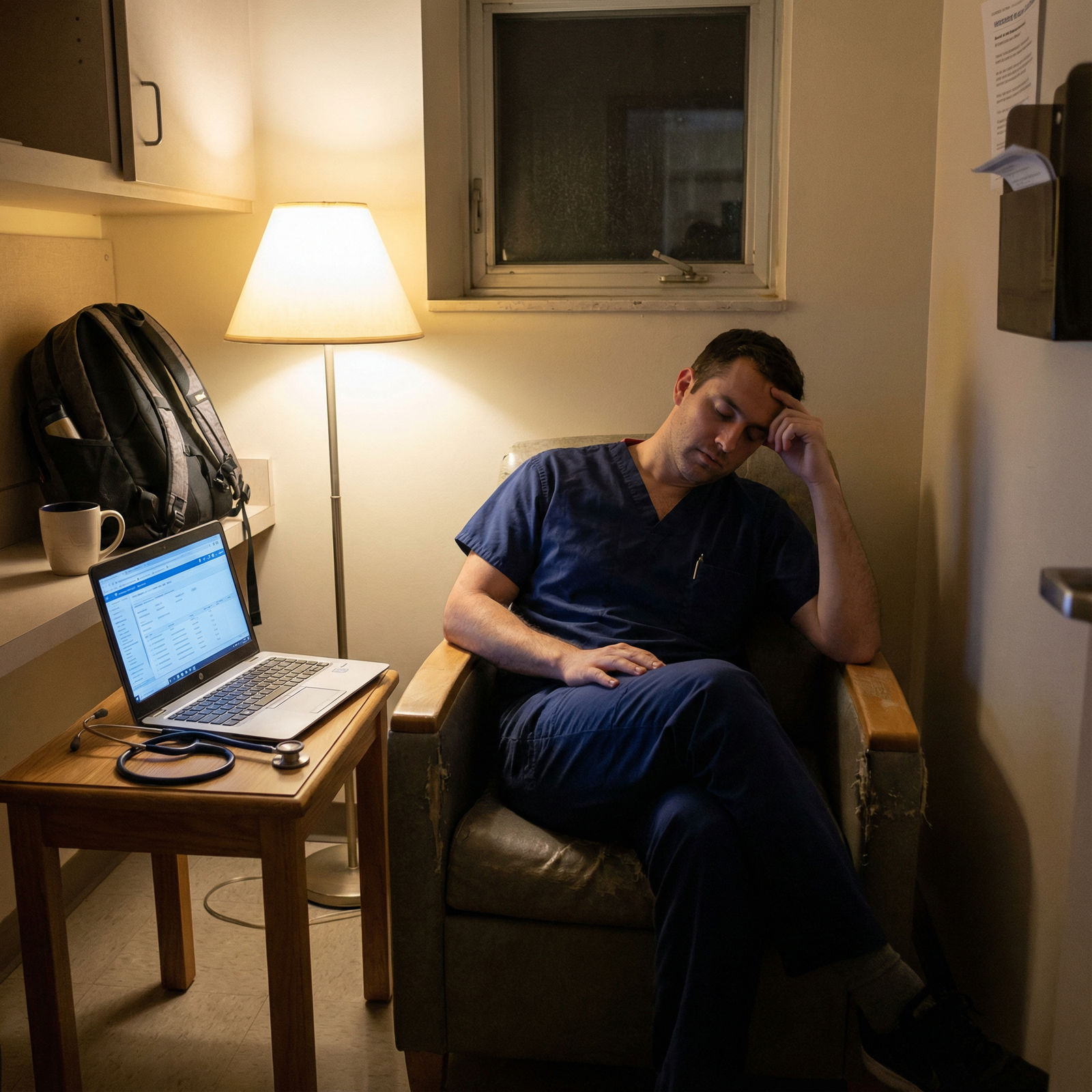
What happens if you finally get the specialty you fought for… and the hours slowly make you start to hate it?
Because that’s the nightmare, right? Not failing. Not going unmatched. But matching… and realizing the thing you built your whole identity around feels like a trap you created for yourself.
Let me say this bluntly: you are not the first person to have this fear, and you absolutely won’t be the last.
The Ugly Truth About Long Hours (That Nobody Likes Saying Out Loud)
Everyone talks about “passion” and “calling” when you choose a specialty. Nobody puts on the brochure: “By PGY-2 you might be crying in your car at 5:30 am, wondering how the hell you’re supposed to do this for the rest of your life.”
Here’s what actually happens when the hours get brutal:
- You stop recognizing yourself outside the hospital.
- The thing you loved about the specialty gets drowned in pages, notes, and endless scut.
- You start wondering if you made a catastrophic, irreversible mistake.
And then your brain goes into overdrive:
- “If I hate this, I’ve wasted my 20s.”
- “What if I’m too weak for this field?”
- “Everyone else seems fine. Why am I the one falling apart?”
I’ve seen versions of this in:
- Surgery residents who loved the OR but hated the 4am wakeups and 80-hour weeks.
- IM residents who liked thinking through cases but felt like note-writing machines.
- OB/GYN residents who loved deliveries but were destroyed by nights and constant emergencies.
Here’s the part people don’t tell you: feeling like you “hate” your specialty during the worst parts of residency does not automatically mean you chose wrong.
Sometimes it just means you’re exhausted. And exhaustion colors everything.

| Category | Value |
|---|---|
| PGY1 | 45 |
| PGY2 | 60 |
| PGY3 | 55 |
| PGY4+ | 50 |
Burnout rates are insanely high in residency. That alone should tell you: if you’re struggling, that’s normal. Not a moral failure, not proof you ruined your life.
How To Tell If It’s The Hours… Or The Specialty
This is the question that haunts people at 2am in the call room:
“Do I hate my specialty, or do I just hate my life right now?”
There’s no flawless test, but there are patterns. When I’ve seen residents truly in the wrong field versus residents who are burned out but ultimately okay, they usually sound different.
You might be dealing with mostly burnout/hour issues if:
- On your best days (reasonable census, decent sleep, cases go well) you think, “I actually like this.”
- You enjoy the core tasks: the surgeries themselves, the diagnostics, the deliveries, the clinic visits… when you’re not utterly fried.
- Your thoughts sound like: “If I just had fewer patients / better staffing / better schedule, this could be great.”
You might be dealing with a deeper mismatch if:
- Even on lighter rotations, you feel dread and emotional resistance to the core work.
- You find yourself envying completely different specialties on a daily basis (e.g., you’re in surgery constantly thinking “I wish I were doing outpatient psych right now”).
- Your thoughts sound like: “Even if I slept 9 hours and had a perfect schedule, I wouldn’t want to do this type of medicine.”
Let me break that into something more concrete.
| Situation | More Likely Burnout/Hours | More Likely Wrong Specialty |
|---|---|---|
| Feel better on easier rotations | Yes | Not really |
| Dread even on chill rotations | Maybe | Yes |
| Still like patients/content | Yes | Less likely |
| Fantasize about totally different field | Sometimes | Often |
| Main complaints = sleep, hours, workload | Yes | Not enough on its own |
None of this is perfect. You can be burned out and in the wrong place. But you need some way to separate “my brain is on fire from sleep deprivation” from “I hate the core identity of this job.”
If you can honestly say: “When I’m rested, I don’t hate it” — that’s huge. That suggests your fear is more about the training environment than the specialty itself.
Worst-Case Scenarios (Let’s Actually Look At Them)
Your brain is probably running worst-case simulations anyway, so let’s drag them into the light and actually examine them.
Worst-case fear #1: “I’ll be trapped forever in a specialty I hate”
No, you won’t.
Is it easy to switch specialties? No.
Is it impossible? Also no.
People switch:
- From surgery to anesthesia.
- From OB/GYN to family or hospitalist work.
- From radiology to psychiatry.
- From competitive to less competitive specialties.
- From hospital-based to outpatient-heavy jobs.
Do you pay a price? Time, money, extra training. It sucks. But it’s survivable. And people on the “other side” will tell you they’re glad they did it, even if it meant starting over as a PGY-1 again.
Here’s what usually makes switching tricky:
- Visa issues (if you’re an IMG on a visa).
- Massive loans and delay in attending salary.
- Competitive-to-competitive switch (e.g., plastics to derm).
- Program drama / references.
Still. Not a death sentence. Just annoying and painful.
Worst-case fear #2: “What if I stay, and my life just… sucks forever?”
Residency ≠ real life as an attending.
Training is front-loaded suffering. You have:
- Less control over your schedule
- Less control over patient load
- Less say in who you work with
- More overnight call, more random weekends, more arbitrary rules
Attending life is wildly variable. There are:
- Outpatient jobs with 4-day work weeks
- Hospitalist gigs with 7-on-7-off
- Subspecialty jobs with minimal nights
- Academic positions with protected time
If you like the medicine but hate the lifestyle right now, you still have levers to pull later:
- Choosing a different practice setting (academic vs community vs outpatient)
- Negotiating schedule
- Cutting FTE (0.8, 0.9 instead of 1.0) when loans aren’t crushing you
- Moving to a different region with better staffing/work-life balance
You are not signing a blood oath in residency to do 80-hour weeks until you die.
Worst-case fear #3: “If I admit I’m struggling, they’ll think I’m weak”
Honestly? Some people will. The wrong people.
The right people — the residents one or two classes ahead who quietly tell you: “Yeah, PGY-2 almost broke me too” — will get it.
I’ve watched people white-knuckle it in silence because they were terrified of looking weak, only to end up:
- On probation
- On the edge of quitting
- In full-blown depression
Versus the ones who finally cracked and told their PD or chief, “I’m not okay,” got:
- Adjusted rotations
- Therapy time carved out
- Support from co-residents
- Real talk about options
Is every program safe and supportive? No. Some are toxic. That’s another conversation. But hiding it 100% of the time because you’re terrified of judgment usually backfires.
Concrete Things You Can Actually Do (Not Just “Practice Self-Care”)
Let’s say you’re already in residency and you’re spiraling about this. What the hell do you do today?
1. Track your feelings on different types of days
Don’t rely on vague memory. Your brain lies when you’re wiped.
For 4–6 weeks, jot down:
- Sleep hours
- Rotation/type of day (clinic, OR, call, wards, consults)
- 1–10 rating: “How much do I hate this specialty today?”
- 1–10 rating: “How much do I hate my life today?”
Patterns matter. If your “hate my specialty” score drops on clinic days or post-call days off, that tells you something. If it’s a rock-solid 9/10 no matter what, that tells you something too.
2. Talk to a PGY above you who you actually trust
Not the always-positive robot who “loves every minute of it.” Someone real.
Ask them:
- “Did you ever think you chose the wrong specialty?”
- “Was there a specific year/rotation that was the worst?”
- “Do you still feel this way now, or did it pass?”
I’ve had senior residents admit:
“I almost applied out during PGY-2. Now, as a chief, I’m glad I stayed — but I would never judge someone who decided to leave.”
You need that context. Because your brain will tell you you’re uniquely broken. You’re not.

3. Get brutally specific about what you actually hate
Vague “I hate this” feelings are overwhelming. Specific ones are actionable.
Hate:
- Waking up at 4am?
- Being in the OR for 12 hours straight?
- Dealing with families?
- Writing endless notes?
- Overnight admissions chaos?
Write it down. Then ask:
- Is this temporary (a particular rotation, year)?
- Is this modifiable later (as an attending)?
- Is this baked into the specialty forever?
Example:
- Being in the OR at 2am for appys and choles? That’s residency/common early attending stuff.
- Hating the technical aspect of surgery (standing for hours, fine motor stuff, working in a dark hole)? That’s core surgery, forever.
You’re allowed to hate temporary suffering. That doesn’t automatically mean you hate the specialty.
4. Quietly explore what switching would actually involve
Sometimes you need a plan B just to breathe.
Doesn’t mean you’ll use it. But knowing, “If I absolutely needed to pivot, here’s how it would go…” can stop the spiraling.
That might mean:
- Reading your institution’s GME policies on transfers.
- Talking informally (and carefully) to a mentor not directly supervising/evaluating you.
- Researching timeline differences (e.g., IM to anesthesia, Gen Surg to EM, OB to FM).
You don’t announce “I hate my specialty, I’m leaving” on day one. You gather intel like a paranoid raccoon, which frankly is the right approach.

| Step | Description |
|---|---|
| Step 1 | Feeling Miserable |
| Step 2 | Track good vs bad days |
| Step 3 | Explore other fields |
| Step 4 | Talk to senior residents |
| Step 5 | Discreetly research transfers |
| Step 6 | Finish residency, choose better job |
| Step 7 | Talk to trusted mentor or PD |
| Step 8 | Hate content or just hours |
| Step 9 | Improves with time |
5. Mental health care. No, really.
You can’t accurately judge your entire career path when you’re:
- Sleeping 4 hours a night
- Eating graham crackers for dinner
- Silently having panic attacks at sign-out
Therapy is not going to magically make 28-hour calls “fun,” but it will:
- Help you separate “this is miserable right now” from “this will always be miserable”
- Challenge the all-or-nothing thinking (“I ruined my life,” “I’m too weak”)
- Give you coping tools so you’re not making giant life decisions in pure survival mode
And honestly, burnout-depression-anxiety all blend together in residency. If you’re thinking, “If I walk away from this hospital and never come back, that might be a relief,” that’s a red flag to get help — not a moral failing.

If You’re Still Pre-Residency And Terrified Of This Happening
You might not even be in residency yet. Maybe you’re a med student or applicant thinking:
“What if I choose, like, surgery or OB, and then the hours destroy me and I’m stuck?”
You don’t get a 100% guarantee. But you can lower the odds of catastrophic mismatch.
Focus less on:
- Prestige
- What impresses other people
- What sounds cool at parties
Focus more on:
- What type of tired you’re okay with.
Are you okay being physically exhausted (surgery, EM, OB)? Or does emotional exhaustion from difficult conversations drain you more (IM, heme/onc, palliative)? - Whether you like the “baseline day,” not just the highlight reel.
Watching a Whipple is cool. But do you like rounding on post-op day 2, checking drains and electrolytes? - How much control you’ll eventually have over your schedule.
There are flexible paths even inside “brutal” fields, but some are more rigid than others.
Shadow real days, not just procedures:
- A full clinic day, start to finish
- Weekend rounding
- Night shift if possible
Then seriously ask yourself: “If I had to do a version of this for 20–30 years, with more control and better pay… could I live with that?”
Not: “Would I love every second?”
But: “Is this a misery I can tolerate, for a career I overall care about?”

The Part Nobody Says Out Loud
You’re allowed to:
- Regret parts of this path
- Hate whole months or years of your training
- Question your specialty
- Change your mind
- Stay and make it work
- Leave and choose something else
You are not a failure if long hours make you doubt your specialty.
You are a human who’s being pushed to the edge in a system that often chews people up.
If your fear right now is:
“What if long hours make me hate my chosen specialty?”
Here’s the honest answer:
They might make you hate everything for a while. That’s what chronic sleep deprivation and constant stress do.
But over time, patterns emerge. You’ll see whether your anger is at the schedule, the system, the way you’re treated… or at the actual medicine itself.
And if — worst case — you really did pick wrong? There are exits. They’re messy. They’re annoying. But they exist. You are never as trapped as you feel at 3am post-call.
FAQs
1. How long should I “wait it out” before deciding I chose the wrong specialty?
If you’re in your first 6–9 months, your data is distorted by sheer shock and adjustment. Usually by the end of PGY-1 or early PGY-2, you start to see clearer patterns: which rotations you tolerate, which you dread, whether things feel even slightly better with more competence. If by late PGY-2 you still hate the core work on good days, that’s when I’d take the “wrong specialty” possibility seriously and talk to mentors about options.
2. What if everyone else in my program seems fine and I’m the only one struggling?
You’re not seeing the whole story. I’ve watched residents look composed on rounds and then cry in the stairwell between pages. Some people are just better at front-stage acting. Also, resilience varies. That doesn’t mean you’re weak; it means the job is mismatched with your wiring or your current reserves. One honest conversation with a co-resident often blows up the illusion that “everyone else is fine.”
3. Will switching specialties ruin my career or make programs not want me?
Programs care about whether you can do the work they need, not whether you had doubts before. If you can explain your story coherently — what you learned, why the new field fits better, how you’re not running away but moving toward something — you won’t be radioactive. Is it harder than staying put? Yes. Is it career-ending? Not even close.
4. How do I know if I should talk to my PD about this or keep quiet?
If you’re actively unsafe (suicidal thoughts, can’t function, making dangerous errors), you have to loop in someone with real authority, whether that’s your PD, APD, or GME. If you’re just “questioning” but still functioning, start smaller: senior residents, a mentor outside your program, therapy. Once you have clarity — “I’m burned out but staying” vs “I’m seriously considering switching” — then you decide if/when to involve leadership. You don’t owe them your every fleeting doubt, but you also shouldn’t hide a full-blown crisis until everything explodes.
Key points:
- Long hours can make any specialty feel awful; that alone doesn’t mean you chose wrong.
- Pay attention to how you feel on your best days — that’s the truer signal about fit.
- You’re never as trapped as you feel; there are ways to adjust, switch, or redesign your path, even if it’s messy.



















