If you liked all your interviews, you have a problem. A good problem—but still a problem. And if you do not handle it with a clear system, you will randomize your future.
This is fixable. You need a concrete, mechanical tie‑breaking system that forces vague “vibes” into hard choices.
I am going to give you one.
Step 0: Stop Asking “Which Is Best?” And Ask “Best For What?”
Most applicants get stuck because they are asking the wrong question.
They keep trying to answer:
“Which program is better: Program A or Program B?”
Wrong frame.
You need to ask:
“Better for what specific outcome in my life and career?”
You are not picking a trophy. You are picking:
- A training environment that will shape your clinical habits
- A professional network that will open or close doors
- A daily life you must tolerate at 3 a.m. on your 19th straight day
Before you rank anything, you need to define what “better” means for you in the next 3–10 years.
That is where the system starts.
Step 1: Build Your Personal Priority Stack (Non‑Negotiables vs Preferences)
You cannot compare programs until you know what actually matters to you in order.
Not 20 equal “important” factors. That is useless. You need a priority stack:
- Non‑negotiables – If a program fails here, it drops to the bottom. No debate.
- High‑weight factors – These decide close calls.
- Low‑weight factors / tie‑decorators – Nice to have; used only at the very end.
1A. Define Your Non‑Negotiables
Be ruthless. If everything is “non‑negotiable,” then nothing is.
Typical non‑negotiables (examples, not a checklist):
- Must be in commuting distance of partner / kids / sick parent
- Must have strong training in a specific career path (e.g., interventional cards exposure, strong outpatient peds, trauma volume)
- Must not be in a location that worsens a medical or mental health condition (e.g., severe winters if that is a trigger, lack of specific specialists you need)
- Must meet visa or licensing needs (for IMGs, J‑1 vs H‑1B, etc.)
- Must not have malignant culture or clear red flags
Write down 3–5 maximum. If you have 10, you are lying to yourself.
Now go down your list of programs. Any program that clearly fails one non‑negotiable: mark it. That program is out of contention for the top spots. It might still be on the list (NRMP says rank every place you are willing to work), but you are not agonizing over it.
, Location/personal life, Fellowship prospects, Culture/support, Schedule/wellness](https://cdn.residencyadvisor.com/images/articles_svg/chart-example-priority-weights-for-residency-ranking-8059.svg)
| Category | Value |
|---|---|
| [Training quality](https://residencyadvisor.com/resources/residency-ranking-strategy/balancing-location-vs-training-quality-a-practical-ranking-framework) | 30 |
| Location/personal life | 25 |
| Fellowship prospects | 20 |
| Culture/support | 15 |
| Schedule/wellness | 10 |
1B. Choose 3–5 High‑Weight Factors
Now pick the 3–5 things that will do the heavy lifting when programs seem equal.
Common high‑weight factors:
- Training quality / case volume
- Fellowship or job placement
- Location and support system
- Program culture and resident happiness
- Schedule structure and call model
- Research or niche opportunities (global health, QI, MedEd, etc.)
You need to rank these factors themselves. That is where people usually fail.
For example, your stack might look like:
- Training quality and volume
- Location / partner’s job
- Fellowship placement in cardiology
- Culture / how residents actually look and sound on interview day
- Schedule / night float structure
Once that is clear, decisions become much less emotional. You have a hierarchy.
1C. Low‑Weight Tie‑Decorators
These are the “I kind of like that they have…” items:
- Brand name / prestige ego boost
- In‑house gym
- Free food / parking
- Weather
- Newer hospital building
- Slightly nicer resident lounge
These should never overturn a decision driven by high‑weight factors. Use them only if everything else is truly equal.
Step 2: Score Every Program—But Do It Right
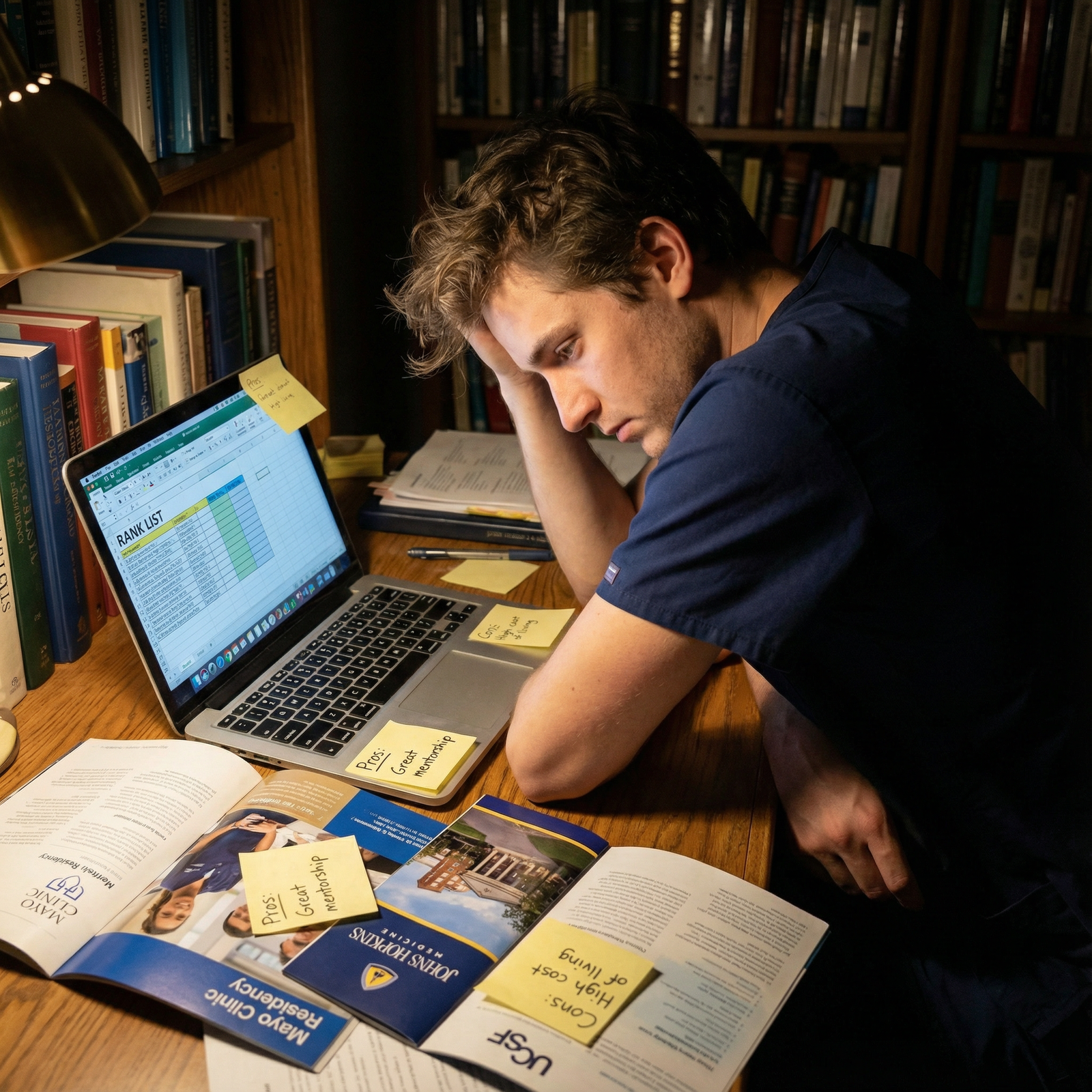
Now you create a scoring system. Not because numbers are magic, but because your brain will happily lie to you under stress. A spreadsheet will not.
2A. Create a Simple Scoring Grid
Open a spreadsheet. Put programs in rows and your 3–5 high‑weight factors in columns.
Use a simple 1–5 scale for each factor:
- 1 = Actively bad
- 2 = Below average
- 3 = Decent / acceptable
- 4 = Strong
- 5 = Excellent / ideal
Then assign weights to each factor based on your priority stack.
Example for Internal Medicine applicant:
- Training quality: weight 3
- Location/family support: weight 3
- Fellowship prospects: weight 2
- Culture: weight 2
- Schedule/wellness: weight 1
So the formula for total score =
(Training × 3) + (Location × 3) + (Fellowship × 2) + (Culture × 2) + (Schedule × 1)
| Factor | Weight | Program A | Program B | Program C |
|---|---|---|---|---|
| Training quality | 3 | 5 | 4 | 3 |
| Location/support | 3 | 2 | 5 | 4 |
| Fellowship prospects | 2 | 4 | 3 | 3 |
| Culture | 2 | 3 | 4 | 4 |
| Schedule/wellness | 1 | 2 | 3 | 4 |
Compute totals. You will see patterns fast.
2B. Use Relative, Not Absolute, Judgement
You are not grading in a vacuum. You are choosing between your actual options.
So think like this:
- “Which program clearly has the best training among my list?” → That one gets a 5.
- “Which has the worst?” → That one gets a 1.
- Others are sorted in the middle.
This avoids everyone getting 4’s and 5’s because “they are all good programs.”
2C. Pay Attention to Huge Gaps, Not Tiny Differences
If Program X scores 42 and Program Y scores 40, that is a wash. Use tie‑breakers later.
If Program X scores 45 and Program Y scores 32, something is very different. Respect that.
The score is not your final rank. It is your starting point.
Step 3: Do the “Future You” Simulation
Now we get out of the spreadsheet and into real life.
Numbers are great, but they will not tell you how it feels to walk to your car post‑call in January.
You need to do three mental simulations for each program:
3A. Worst‑Day Scenario
Picture your worst realistic day as a resident there:
- You are post‑call, exhausted. Code at 4 a.m., terrible interaction with a consultant, you made a small but painful mistake.
- It is cold, or sweltering, or raining sideways.
- Your partner had a bad day too, or you are alone in a city where you know no one.
Now ask:
- “In that moment, do I feel trapped here or supported here?”
- “Is this a city where I can decompress in a way that actually works for me?”
- “Do I trust this program’s leadership and culture to back me when things go wrong?”
If you notice dread or a heavy “I would hate my life there on days like that,” that program drops—no matter how shiny the name.
3B. Best‑Opportunity Scenario
Now picture your best realistic opportunity during residency:
- The attending who can get you into your dream fellowship
- The mentor who will put your name on papers
- The leadership role or niche (ultrasound, MedEd, quality improvement)
Ask:
- “Where is it most likely that this kind of opportunity actually happens?”
- “At which program do I see myself being noticed and pushed forward, not just tolerated?”
This heavily favors places where residents say: “Our PD really goes to bat for us,” and where alumni lists match your goals.
3C. “5‑Year Look‑Back” Question
Last mental test:
Imagine you have finished residency and you are 2 years into fellowship or attending life.
You look back and say: “I am really glad I trained at ___ because…”
Fill in that blank for each program. If you can only come up with:
- “The name sounds good,” or
- “My parents were impressed,”
that is weak.
If for another program you think:
- “That is where I met my mentor and got my first research project.”
- “That is where I learned to run a code with zero hesitation.”
- “That is where I had friends who kept me sane,”
pay attention. That program deserves to climb.
Step 4: Use Structured Tie‑Breakers When Scores Are Close
Now you have:
- A priority stack
- A weighted score for each program
- A gut sense from the future‑you simulations
But you still have multiple programs that feel tied. Fine. Now we bring in a tie‑breaking ladder.
Use this order, top to bottom, and stop the moment one program wins that step.
Tie‑Breaker 1: Training vs Life Tradeoff
Ask yourself point‑blank:
“If Program A gives me clearly stronger training but a clearly worse lifestyle / location, which side of that tradeoff am I willing to sacrifice for three years?”
Be honest. Many people say they value lifestyle, then put the harsh, prestigious program #1 and regret it. The reverse is also true.
Explicit test:
- “If I become an attending and feel slightly undertrained but I saw my family more, can I live with that?”
- “Or would I rather be very well trained even if I was miserable at times?”
Your answer decides the direction.
Tie‑Breaker 2: People You Actually Met
Think about specific people, not abstract “culture.”
- The PD who remembered details about you
- The chief you talked to during breakout
- The resident who answered you bluntly but kindly about their worst rotations
Ask:
- “Whose face do I see when I picture myself as a PGY‑2 asking for help?”
- “Where did I feel I could actually show weakness and not be punished?”
Programs are their people. If one had a PD you trusted instantly and another felt polished but distant, rank the one with real humans higher.

Tie‑Breaker 3: Exit Data—Where Do Graduates End Up?
Look at actual outcomes, not marketing slides.
- Fellowship match lists (if you want fellowship)
- Where hospitalists / primary care grads are working (if you want a job straight out)
- Academic vs community breakdown
- Geographic spread of alumni
If your dream is a cardiology fellowship:
- Program X: “We match 2–3 into cards every year, and you can cold‑email three recent grads.”
- Program Y: “We had one cards match five years ago.”
Do not pretend those are equal because “I liked both interview days.”
Tie‑Breaker 4: Specific Red or Yellow Flags
Go back through your notes and emails. Look for any of these:
- Residents looked exhausted and flat when leadership was not in the room
- Dodged questions about duty hours with jokes
- PD or faculty bad‑mouthed other programs or specialties
- Vague answers about how they handle struggling residents
- Consistent online chatter about toxicity that nobody addressed clearly
If two programs are tied, the absence of red flags wins.
Tie‑Breaker 5: Gut Check—The 24‑Hour Rule
If you are still stuck:
- Pretend you must submit a rank list now with Program A above Program B.
- Write it down. Then walk away for 24 hours.
- Notice any mental friction.
If during that 24 hours you keep thinking, “I really hope I do not match A over B,” that is a signal. Reverse them.
This is not magical intuition. It is you noticing where your values are not aligning with your stated logic.
Step 5: Use a Visual Timeline to Pressure‑Test Your List
For some people, seeing their future laid out helps more than any score.
Take your current top 5–7 programs and run them through a timeline thought exercise.

| Period | Event |
|---|---|
| Residency (PGY1-3) - Learning curve | Strong vs Moderate vs Weak training |
| Residency (PGY1-3) - Support system | Family nearby vs Long-distance |
| Early Career (Years 4-6) - Fellowship or Job | Matched dream vs Acceptable alternative |
| Early Career (Years 4-6) - Confidence level | High vs Adequate |
| Later Career (Years 7-10) - Career doors | Broad options vs Limited |
| Later Career (Years 7-10) - Lifestyle habits | Sustainable vs Burned out |
Now literally speak this out or write it:
- “If I go to Program A: For 3 years I live in ___, with ___ support, get ___ training, and am most likely to end up in ___ job / fellowship.”
- “If I go to Program B: For 3 years I live in ___, with ___ support, get ___ training, and am most likely to end up in ___ job / fellowship.”
Seeing the trajectory often makes one program feel obviously better aligned, even if interview day felt the same.
Step 6: Beware the Three Biggest Ranking Traps
People do dumb things at this stage. Here are the ones I see repeatedly, and how to avoid them.
Trap 1: Chasing Brand Name Over Fit
I have seen applicants put a top‑5 name #1 even though:
- It is across the country from any support
- It has a reputation for brutal schedules
- They left the interview day feeling small and anxious
Then they end PGY‑1 in tears, saying, “But it is [insert name].”
You are training to become a competent, functioning physician. A fancy name with poor fit is a bad trade.
Use this rule:
Only let prestige break a tie when the fit is already acceptable in your top priorities. Never let prestige override your non‑negotiables.
Trap 2: Letting Other People’s Anxiety Rank For You
You will hear:
- “My attending said I would be crazy not to put X first.”
- “My parents really want me to stay close.”
- “Everyone on Reddit worships this program.”
These people do not do your call shifts. They do not sit with your patients. They do not share your rent or your loneliness.
You can consider their input, but your priority stack controls the final order. If there is a mismatch, side with the person who has to live the life: you.
Trap 3: Overweighting Interview Day Vibes
Interview days are staged. Everyone is on good behavior. Food is better, attendings show up, residents are told not to scare you.
Yes, your comfort there matters. But:
- One super charismatic resident does not fix mediocre training.
- One slightly awkward PD does not negate rock‑solid support and happy residents.
- Weather on the interview day means nothing.
Return to data:
- Rotation schedules
- Call structure
- Case volume
- Fellowship outcomes
- How residents actually talked about their days, not the rehearsed slides

| Category | Value |
|---|---|
| Prestige chasing | 80 |
| Family pressure | 60 |
| Interview vibes only | 70 |
| Ignoring red flags | 90 |
(Think of those numbers as “regret potential” on a 0–100 scale. High is bad.)
Step 7: Lock In the List, Then Stop Tinkering
At some point, you have to commit. Here is how to make that final push.
7A. Final Consistency Check
Take your almost‑final list and test for priority consistency.
For each pair where a lower‑ranked program beats a higher‑ranked one on your #1 or #2 priority, ask:
- “Do I actually care more about some other factor I did not admit earlier?”
If you catch yourself saying, “Well, I guess I actually care more about being near family than research,” fix your priority list and adjust ranks. Better to correct now than post‑Match.
7B. Do a Forced‑Choice Drill From Top to Bottom
Start with your current #1 and #2:
- “If I only matched at one of these, which would I open the email hoping for?”
- Whichever you pick stays higher. Lock that. Do not re‑open it again.
Now compare that winner to #3. Same question. Work down the list.
You are not just comparing numbers; you are comparing your real emotional response to each forced choice.

7C. Set a Deadline and Walk Away
Set a personal deadline a few days before the actual NRMP deadline.
By that date:
- Enter your list in the system
- Double‑check for obvious errors (e.g., forgetting a program)
- Hit certify
Then stop. No late‑night rearranging because someone on a forum ranked a program differently.
Your system is better than last‑minute panic.
A Concrete Example: Internal Medicine Applicant With 6 Good Interviews
Let me walk you through a real‑world style scenario so you see how this works.
You have 6 IM programs you genuinely liked:
- University A (big academic, across the country)
- University B (regional academic, 2 hours from family)
- Community‑University hybrid C (same city as partner)
- County D (heavy underserved, tougher schedule, great autonomy)
- Community E (suburban, very friendly, fewer fellowships)
- University F (prestigious name, residents seemed tired)
Your priority stack:
- Training quality and autonomy
- Location / partner
- Cards fellowship prospects
- Culture / resident support
- Schedule / wellness
You score each 1–5 on those, weighted as:
- Training: 3
- Location: 3
- Fellowship: 2
- Culture: 2
- Schedule: 1
You end up with total scores like:
- A: 43
- B: 41
- C: 44
- D: 45
- E: 38
- F: 40
So initial sort: D > C > A > B > F > E.
Now tie‑breakers and reality:
- Worst‑day scenario: You realize D’s city would isolate your partner and you would both be miserable.
- Future‑you simulation: You can see yourself being very well‑trained at D, but also potentially burned out. At C, training is slightly less intense but your relationship survives intact.
- People: At C, you really clicked with the PD and a cards‑focused resident. At D, you respected them but felt a bit like a cog.
You decide your stated #2 priority (partner/location) really does matter. You move C above D despite the raw training edge. Final top looks like:
- C
- D
- A
- B
- F
- E
Is that “objectively correct”? No. It is internally consistent with your life and your goals. That is what matters.
How To Use This System When You Truly “Liked Them All”
Here is the stripped‑down protocol you can execute in a weekend:
Write your priority stack:
- 3–5 non‑negotiables
- 3–5 high‑weight factors ranked in order
Score every program on those high‑weight factors (1–5) and use simple weights to get a first‑pass total.
Run mental simulations (worst‑day, best‑opportunity, 5‑year look‑back) and adjust obvious outliers up or down.
Apply the tie‑breaking ladder for close calls:
- Training vs life tradeoff
- Specific people you trust
- Alumni outcomes
- Flags
- 24‑hour gut check
Do a top‑down forced‑choice pass and lock in:
- “If I only match at one of these two, which would I secretly hope for?”
- Use that to set final order.
Certify your list and stop. Do not rewrite your future every night before the deadline.

Bottom Line
Here is what you should carry with you:
- A clear, ranked set of personal priorities beats vague impressions and other people’s opinions.
- A simple weighted scoring system plus structured tie‑breakers gives you a rational way to separate programs you “liked equally.”
- Your final rank list should reflect the life you are willing to live for the next three years, not just the shiniest logo or loudest outside voice.
Use a system. Make the hard calls once. Then let the Match do its job.




















