The fear that you’re going to miss something overnight is not irrational. It’s the cost of being the last line between a patient and disaster.
The Fear: “What If Someone Crashes And I Miss It?”
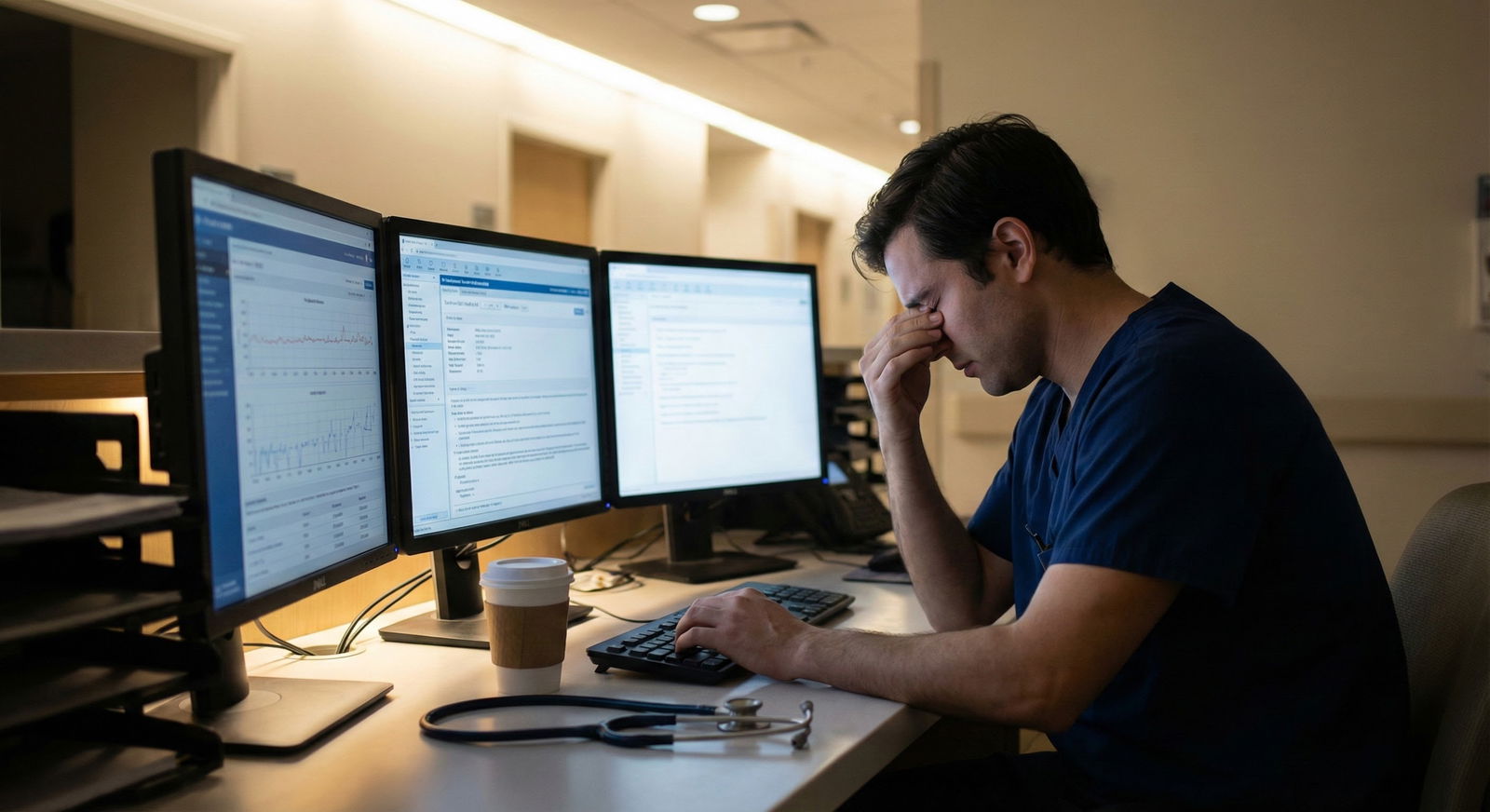
You know that moment. You’re halfway through a note, pager finally quiet for ten seconds, and your brain whispers: What if someone is silently decompensating on the floor and I’m just… sitting here?
You try to ignore it. You re-check the census. You scan vitals again. You reread the sign-out. Still feels like you’re one oversight away from killing someone.
I’m going to be blunt: you will miss something at some point. Everyone does. Interns, seniors, attendings who’ve been doing this for 25 years. The point of a safety net isn’t to make you perfect. It’s to:
- Catch most problems early enough
- Make the misses less dangerous
- Let you sleep for more than 90 seconds at a time without spiraling
You’re not trying to become omniscient. You’re trying to become systematically paranoid.
Let’s build that system.

| Category | Value |
|---|---|
| Missing deterioration | 85 |
| Code response | 70 |
| Documentation errors | 55 |
| Medication mistakes | 60 |
| Angry families | 40 |
Step 1: Build A Ruthless Sign-Out Filter
Everyone says “good sign-out is key” and then hands you chaotic monologues at 6:45 pm.
You can’t control what they say. But you can control what you pull out of them.
When you’re getting sign-out, don’t just listen. Interrogate. Your inner monologue should basically be: How is this patient going to try to die on me tonight?
For every patient, force three things out of the day team:
Biggest active problem
Not their entire medical history. What could hurt them tonight?- “Hypoxic pneumonia, on 4L, sat 92–94.”
- “GI bleed, Hb dropped from 9 to 7.5 today, already transfused 1 unit.”
- “Alcohol withdrawal, CIWA 15 this afternoon, got Ativan x3.”
What they’re worried about overnight
This is where a ton of failures happen—no one says the quiet part out loud. Ask:- “What are you most worried will happen between now and 7 a.m.?”
- “If I get a call on this patient, what is it most likely to be?”
Clear “if-then” plans
If you wake up at 3 a.m. and your brain is mush, you need recipes, not philosophy.- “If SBP < 90, give 500 mL LR, recheck, page me / ICU if still low.”
- “If CIWA > 15 even after meds, call me and consider phenobarb load.”
- “If increased work of breathing, put on NRB, STAT CXR, call rapid if not improving.”
If they can’t give you an if-then plan for a risky patient, that’s a red flag. Push a little:
- “Can we agree on some parameters for calling you or ICU?”
- “If their oxygen needs go up, where’s your threshold for moving them?”
Write these if-then’s in your own words in your sign-out so they’re not buried in a 40-line HPI.

Step 2: Create A Mental “Watch List” – And Treat It Like An ICU
Your whole census is not equally dangerous. Your brain acts like it is, especially at 2 a.m., but it’s lying to you.
You need a watch list. Not 20 patients. Not half the service. The 3–10 that could actually tank tonight.
How to pick them:
- Anyone who changed O2 requirements in last 24 hours
- Anyone with soft BPs, sepsis, or new tachycardia
- Anyone with active bleeding, chest pain, or neuro changes
- Anyone where the day team said, “I’m just a little nervous about them”
Put a symbol next to them in your list, or keep a short separate list. These are your “ICU-lite” people, even if they’re on the floor.
For each watch-list patient, know:
- Code status and goals of care
- Last vitals trend (not just one snapshot)
- Fluid status (giving, restricting, or clueless)
- One concrete trigger to re-evaluate them
Then—this is key—build in intentional check-ins.
- Early night: glance at their vitals and nursing notes after you’ve settled from sign-out
- Mid-shift: do a “vitals sweep” on them even if no one’s paged you
- Late night: before you even think about sleeping, check them one more time
If something feels off on the screen—slight trend in RR, more frequent PRNs, nurse notes saying “appears more confused”—go lay eyes on them. 3 minutes at bedside can prevent your worst-case code-at-4 a.m. nightmare.
Step 3: Use Nurses As Your Early Warning System (For Real, Not In Theory)
Every resident says “Nurses are my eyes and ears.” Then spends the night low-key annoyed at pages.
You’re scared of missing something? Then your best move is to turn nurses into collaborators, not adversaries.
At the start of the shift, if you can, say something like:
- “Hey, I’m on cross-cover tonight. I really want to know if anyone is making you even a little nervous. I’d rather be over-paged than miss something big.”
But—and this matters—add boundaries to protect yourself:
- “If it’s about pain meds or sleep meds and they’re stable, batching those pages together is super helpful.”
Give nurses permission and structure:
- Ask: “Who are you most worried about tonight?”
- When they call with a vague concern (“they just don’t look right”), don’t blow it off. That’s often the earliest cue.
You will 100% get some pages that feel unnecessary. That’s the tax you pay for catching the necessary ones early.
| Situation | Good Response | Dangerous Response |
|---|---|---|
| "Patient just looks off" | Go see them, quick exam, trend vitals | "If vitals normal, just watch" |
| New mild tachycardia | Check fluids, pain, sepsis, meds | "It’s just anxiety" |
| Soft BP but asymptomatic | Recheck manually, consider bolus/order | Ignore and continue notes |
Step 4: Create A “When In Doubt” Playbook For Yourself
Most of the overnight terror comes from this thought: What if I don’t know what to do? What if I freeze?
You don’t need to know what to do for every scenario from memory. You need defaults—simple first moves that buy you time and safety.
For common overnight situations, commit to a basic template:
Hypotension (real, not just bad cuff)
- Re-check manually, check HR, mental status, UOP
- If septic/bleeding suspected: fluids (unless clear contraindication)
- If unclear: small fluid challenge, re-eval, consider labs, low threshold to call senior/ICU
New hypoxia
- Check positioning, airway, secretions
- Increase O2, check RR and work of breathing
- Quickly review last CXR, diagnoses
- If any distress: call rapid or at least senior, don’t “watch” escalating O2 needs
Change in mental status
- Check vitals, glucose, meds list (opiates, benzos, anticholinergics)
- Quick neuro exam
- Think: infection, metabolic, drugs, stroke
- If focal deficits or sudden: CT and call someone ASAP
Are these complete algorithms? No. But they’re enough to stop you from doing nothing.
Write your own 1-page “night playbook” and keep it in your white coat or notes app. Not 20 pages. Just:
- Hypotension
- Hypoxia
- Chest pain
- Delirium / agitation
- Fever in a sick person / neutropenia
You’ll still call for help. But you’ll be doing something while you wait.

| Category | Value |
|---|---|
| Month 1 | 9 |
| Month 2 | 7 |
| Month 3 | 6 |
| Month 4 | 5 |
Step 5: Make Your Own “I Checked” Checklist For Every Shift
Your brain loves to torture you with “Did I actually check that?” at 4:30 a.m.
Give it less ammo.
Create a tiny, non-negotiable nightly checklist. Not 30 boxes. 5–7 max. Stuff that directly reduces the chance of catastrophic misses.
Example:
- Reviewed sign-out and clarified plans for all watch-list patients
- Looked at vitals trends for watch-list patients at least twice
- Reassessed anyone with rapid response / big change after intervention
- Checked that any stat orders actually happened (labs, imaging, meds)
- Before lying down: quick scan of vitals on watch-list and any new concerning pages
When your brain screams “What if I forgot something huge?” you can answer it with: “I did my checklist. If something slipped, it slipped in spite of that, not because I was careless.”
That distinction matters. It’s the difference between being reckless and being human.

| Step | Description |
|---|---|
| Step 1 | Start Shift |
| Step 2 | Get Sign-out |
| Step 3 | Create Watch List |
| Step 4 | Talk to Nurses |
| Step 5 | Use Night Playbook |
| Step 6 | Run Mini Checklists |
| Step 7 | End-of-Night Review |
Step 6: Decide Now What You’ll Never “Watch” Alone Overnight
A lot of bad outcomes come from that one word: “watch.”
“We’ll just watch it.”
“We’ll see how they do.”
“I’ll keep an eye on it.”
Decide before you’re exhausted which things you refuse to just “watch” solo:
- Rising O2 requirements
- New chest pain in a cardiac patient
- Drop in SBP with rising HR
- Sudden change in mental status
- New focal neuro deficit
- Neutropenic fever
For those, your rule is: “I am not the only brain thinking about this.” That could mean:
- Calling the senior
- Calling the attending
- Calling ICU / rapid response
You will feel dumb sometimes. You will feel dramatic. You will feel like you’re overreacting.
I’ve watched more residents get in trouble for not calling than for “bothering” someone at 2 a.m. Senior residents complain sometimes, but when stuff hits the fan, what they always say is, “Why didn’t you call me earlier?”
You don’t get extra points for guessing right alone in the middle of the night.
Step 7: Have A Post-Shift Ritual To Keep The Regret Spiral In Check
Another fun part of residency: even when you survive the night, your brain will replay every borderline decision on the drive home.
You can’t stop that entirely. But you can structure it.
Try this after sign-out in the morning, before you leave:
Ask yourself three questions:
“Was there anyone I’m actually still worried about?”
- If yes, tell the day team clearly: “I’m nervous about bed 12, they had X overnight, I’d re-check them early.”
“Did I ignore my gut on anyone?”
- If yes, make a mental note: next time, trust the gut earlier. That’s how you calibrate your instincts.
“Was I safe, even if I wasn’t perfect?”
- Did you check on people? Call for help when needed? Correct things when you realized you were wrong?
You’re allowed to feel like crap about a rough night. But don’t walk away with the vague story: I’m dangerous, I miss things, I shouldn’t be a doctor. Replace it with something more specific:
- “I was late on recognizing X, but once I did, I escalated appropriately. I need to tighten my trigger for calling earlier.”
That’s growth. Not self-destruction.
FAQ (Exactly 6 Questions)
1. What if I miss something and a patient dies—does that mean I’m not cut out for this?
No. It means you’re human in a brutal system. Outcomes are multi-factorial: disease severity, staffing, nurse ratios, timing, handoffs, sheer bad luck. Your job is not to be perfect; it’s to be systematic: decent sign-outs, reasonable watch list, early escalation. When something bad happens (and eventually something will), the question is: did you ignore clear red flags, or did you act in good faith with reasonable steps? If it’s the latter, painful as it is, that’s medicine, not personal failure.
2. How do I know when I’m over-calling versus responsibly escalating?
If you’re calling for help on every mild fever or every BP of 98/60, that’s probably excessive. If you’re calling when there’s a trend, a significant change, or you’re genuinely stuck between two risky options—that’s appropriate. A good rule: if you’d feel sick to your stomach going to sleep without at least telling someone about it, call. Over time, seniors will give you feedback and your threshold will calibrate. Early on, lean toward “too early” rather than “too late.”
3. I’m so anxious overnight that I can’t focus—how do I function like this?
You don’t fight anxiety with vibes. You fight it with structure. The watch list. The mini-checklist. Simple if-then plans. Those external systems keep you moving when your mind wants to spin. Also, micro-breaks matter: 3 minutes away from the screen, deep breath, sip of water. If your anxiety is spilling into panic territory—heart racing, can’t sleep post-call, dread all week—talk to someone: a trusted senior, residency leadership, or mental health support. White-knuckling it forever is not sustainable.
4. What if the day team gives me useless sign-out and I’m set up to fail?
Then you compensate by being a little more aggressive up front. Ask sharper questions. Re-summarize out loud: “So tonight I’m mainly watching X, Y, Z on this patient, and if A happens I’ll do B—does that sound right?” If something really isn’t clear, say: “Before you leave, I need a clear plan for what you’d want done if they decompensate.” They may be tired, but you’re the one holding the bag at 3 a.m. It’s reasonable to insist on minimally decent communication.
5. How many times should I re-check vitals and charts without driving myself insane?
You’re not a telemetry machine. You don’t have to obsessively watch vitals. For most patients, once or twice is fine. For your watch-list patients, two or three deliberate checks over the night is reasonable: early, middle, pre-sleep. The point is intentionality: “I’m going to scan vitals at midnight and 4 a.m. for my risky patients,” not “I’m going to stare at the board in a constant state of panic.”
6. I feel guilty sleeping at all on call—what if something happens while I’m out?
Here’s the cold truth: a completely sleep-deprived resident is less safe, not more. Your safety net is not “never sleep.” It’s: clear sign-out, watch list, nurse communication, and agreed escalation thresholds. Once those are in place, you’re allowed to rest. You’re not abandoning patients; you’re preserving enough brain function to respond when they actually need you. Years from now, no one’s going to hand you a medal for staying awake all night and making worse decisions.
One day you’ll look back and realize the fear of missing something never fully goes away—it just stops owning you, because you’ve built systems around it.
You might not remember every night shift, or every patient, or every lab you ordered at 2:37 a.m.
But you’ll remember that somewhere along the way, you stopped surviving nights by sheer panic and started surviving them by design.




















