It is 6:45 a.m. You are in borrowed hospital scrubs, already sweating a little. First day on a high-volume surgical service. The attending walks into the OR, glances at you, then at the resident and says, “Who’s this?”
You open your mouth and say the sentence that quietly ruins more future surgical careers than a bad Shelf score:
“I’m just observing.”
The scrub tech nods, translates that as: “Useless body taking up space.” The resident mentally crosses you off the list of people to teach. The attending barely registers your existence. And the case starts without you.
You think you were being polite. Non‑demanding. Low maintenance.
You were actually telling everyone in the room, “Do not invest in me. I will not be here long. I am not serious.”
Let me walk you through how that tiny phrase kills surgical case volume, mentorship, letters, and future chances—and what to say and do instead before you silently delete your own opportunities.
The Hidden Message Behind “I’m Just Observing”

You think “I’m just observing” means:
“I do not want to be in the way, but I am interested.”
Here is how OR staff actually hear it:
- The attending: “Not worth my time to teach. They will not be here long.”
- The resident: “Extra mouth breather. If I give them the knife, they will panic.”
- The scrub tech: “No need to set up a student gown or extra instruments.”
- The circulating nurse: “Not primary team. Ignore.”
You have announced you are a transient spectator, not part of the team. In a high-pressure environment where everyone is overextended, that matters.
Because in surgery, inclusion equals responsibility. Responsibility equals teaching. Teaching equals case volume and skills. If you tell them you are “just observing,” you opt out. Voluntarily.
And that choice has consequences.
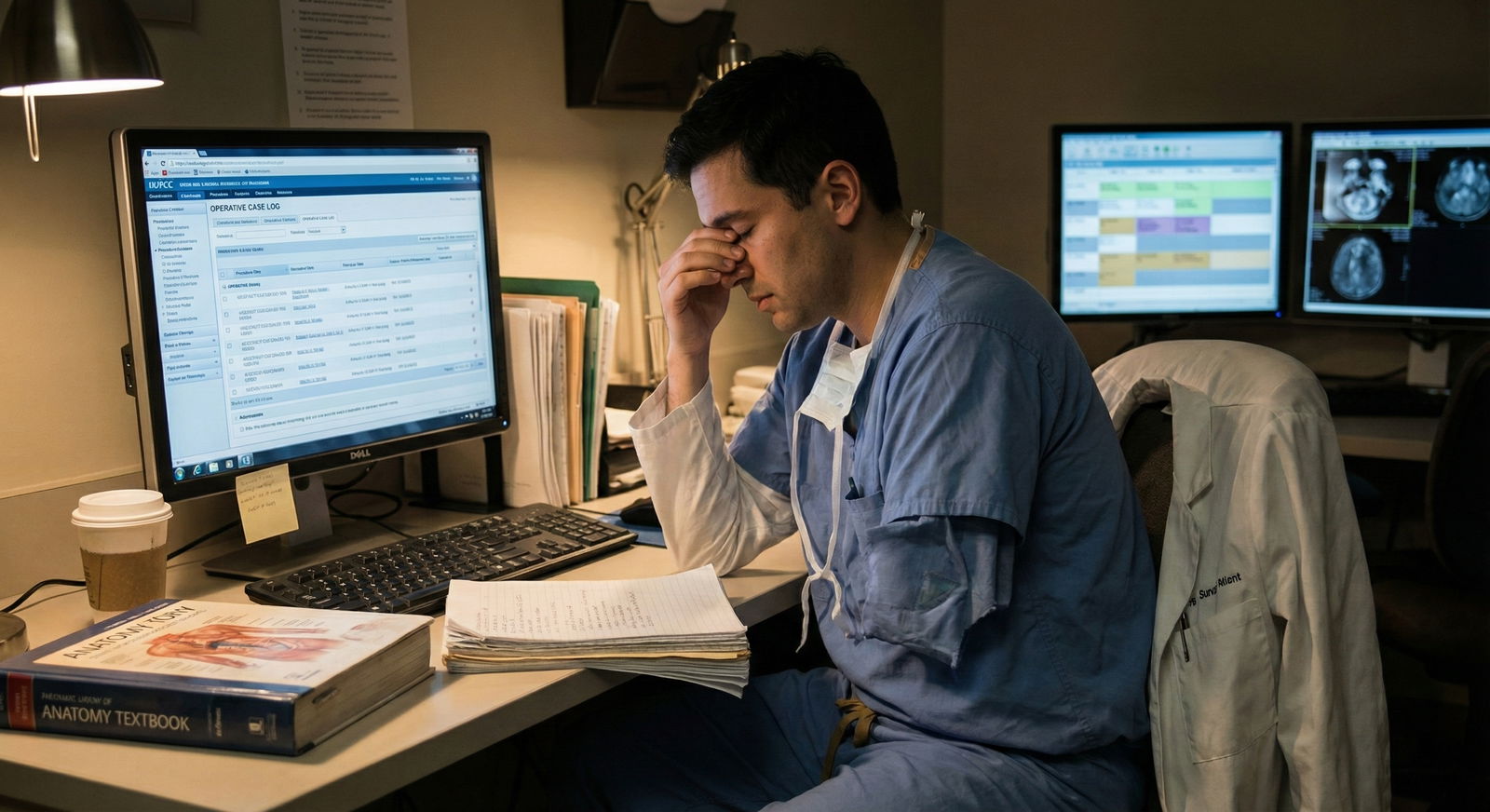
Mistake #1: Turning Yourself into Furniture in the OR
“I stand in the corner and watch. That way I do not bother anyone.”
I have heard that exact sentence from dozens of students who then complain they “never got to do anything.”
Let me be blunt: the OR already has equipment that does nothing but watch. They are called cameras.
When you position yourself as a passive onlooker:
- You get placed physically out of the field
- You miss anatomy because you cannot see the screen or incision angle
- You are invisible when opportunities arise
- You do not build the micro‑trust that leads to “Do you want to close?”
Here is how it plays out. I have seen this a hundred times:
Case: Laparoscopic cholecystectomy.
Two students in the room.
Student A introduced themselves to everyone, offered to help position the patient, held the leg while the SCDs were placed, and asked to scrub if possible.
Student B said, “I’m just observing,” and stood by the wall scrolling their mental To‑Do list.
Guess who got handed the camera.
Guess who got to close the port sites.
Guess who the attending called by name at the end of the day.
You are not punished for being quiet. You are punished for being absent.
Mistake #2: Killing Your Surgical Case Volume Before It Starts
You want surgical exposure. Case numbers. Log entries. Stories for your personal statement.
But you show up to the OR, say “I am just observing,” and then walk out at 10 a.m. to “go check on notes.” You just torched your own case volume.
Here is the harsh reality: most services will not schedule cases for you. Case volume comes from:
- Being physically present when add‑on cases appear
- Being trusted enough to be invited in quickly
- Being known by name by the OR staff who call for help
If the OR staff think of you as “that observer,” they will not come find you when the emergency appendectomy is rolling in at 4 p.m.
Let us be specific.
| Student Type | Days on Service | Avg Cases In Room | Avg Cases Scrubbed | Avg Times Allowed to Suture |
|---|---|---|---|---|
| Passive Observer | 20 | 40 | 8 | 1 |
| Engaged Participant | 20 | 60 | 35 | 15 |
| Known Workhorse | 20 | 70 | 50 | 25 |
Those are rough but realistic proportions from what I see in busy general surgery and ortho services. The difference is not Step scores. Not class rank. It is simply: did you act like “just an observer,” or part of the team?
The biggest mistake: thinking case volume is “given” by the service, rather than earned by presence and engagement.
Mistake #3: Losing Mentorship and Letters You Don’t Even Know You Lost
Attending surgeons are constantly scanning for 2–3 people per year they will actually invest in. They do not have time for 20.
How do they triage? Very simple:
- Who shows up early and stays late consistently
- Who looks like they want to be there
- Who takes small tasks seriously and reliably
The moment you introduce yourself as “just observing,” you fall into a mental bucket:
“Non‑surgical, just passing through.”
You just opted out of:
- Candid feedback
- Extra cases (“Hey, come scrub this hernia before you go home.”)
- Serious letters (“This student truly functioned like an intern…”)
You will never know what you missed, because no one announces, “I was going to offer you this, but then I remembered you said you are just observing.”
They simply offer it to the next person.
Mistake #4: Confusing Humility with Self‑Erasure

| Category | Value |
|---|---|
| Fear of looking stupid | 40 |
| Not wanting to be in the way | 30 |
| Assuming no one wants to teach | 20 |
| Genuine lack of interest | 10 |
Most students who say “I am just observing” are not arrogant. Usually they are nervous, conflict‑avoidant, or trying to be low maintenance.
The intent is respectful. The effect is self‑erasure.
You can be humble and still make it clear you want in. There is a huge difference between:
“I am just observing.”
and
“I am a third‑year on my surgery rotation. I would be grateful for any chance to help—happy to retract, hold the camera, close, or just watch if that is all that is appropriate.”
Same humility. Totally different signal.
Humility says, “I know my place on the team, but I want to contribute.”
Self‑erasure says, “Pretend I am not here.”
Guess which one builds surgical skills.
Mistake #5: Forgetting There Is a Long Memory in Small Fields
Surgery is not anonymous. People talk. They remember.
The resident you brushed off as “too intense” during your M3 year may be the fellowship director five years later. The scrub tech you never bothered to meet may be the one who whispers to the attending, “That student actually helps.”
I remember a student who, on day one of trauma, literally said to the chief, “I am just observing this week because I have an exam.”
That line got repeated (with eye rolls) on rounds, in the call room, and two years later when that same student applied for a sub‑I. They did not get it.
Not because of one sentence. Because that sentence matched their behavior: leaving early, skipping consults, never checking on post‑ops.
Words and actions together build a story about you. “Just observing” is the opening chapter of the wrong story if you want a future anywhere near the OR.
What To Say Instead: Phrases That Create Opportunity

| Step | Description |
|---|---|
| Step 1 | Arrive to OR |
| Step 2 | Introduce to team |
| Step 3 | State interest and limits |
| Step 4 | Ask how to help |
| Step 5 | Get assigned task |
| Step 6 | Offered more responsibility |
| Step 7 | Reflect and adjust |
| Step 8 | Asked about role? |
| Step 9 | Task done well? |
You avoid most of these mistakes by changing a few sentences and backing them with consistent behavior.
When someone asks who you are or what you are doing there, try:
“I am the medical student on this case and would really like to help however is useful. I am comfortable with basic tasks and eager to learn more.”
“I am a third‑year on my surgery rotation. If there is a chance to scrub or even just hold retractors, I would appreciate it. I am happy to step back if the room is too full.”
For anesthesia or other teams: “I am on surgery but trying to understand the whole OR. Is it alright if I stand here and watch? If I am in anyone’s way, please tell me and I will move.”
Notice the pattern:
- You declare your role
- You state your interest
- You show respect for boundaries and space
You are not demanding. You are available.
What To Do Instead: Behaviors That Earn You Case Volume
Words matter, but the OR rewards actions.
Here is the simple, unglamorous playbook that actually increases your case volume and future options.
Before the Case
- Show up early enough to see the patient in pre‑op. Introduce yourself.
- Read the one‑page version of the procedure the night before. Not a textbook. Just enough to know the steps and indications.
- Ask the resident quietly, “Is it alright if I scrub on this one? Anything specific you want me to focus on?”
In the Room
Do not hover motionless. Do not clutch your phone.
Instead:
- Help move the bed or transfer the patient if allowed.
- Ask the scrub tech: “Where would you like me to stand after I scrub so I am not in the way?”
- If you are not scrubbing, position yourself where you can see the field or monitor. If you cannot, ask once, politely, if you may move.
During the Case
Your priorities:
Do your assigned task flawlessly before asking for more.
If you are holding retractors, hold them like your life depends on it. Never let the field drift.Ask short, relevant questions at natural pauses.
“Is this the cystic artery?” beats “What is your advice for future surgeons?”Watch your body language.
Lean in. Track the action. Do not look bored, tired, or checked out. Surgeons watch this constantly.
After the Case
This step gets skipped, and it costs students trust.
- Help with bed transfer and moving the patient out (if permitted).
- Thank the attending, resident, and scrub tech by name.
- If you learned something specific, say it: “Thank you for letting me help close. I had never done subcuticular sutures that way.”
Then—and this matters—show up again the next day. Same energy. Same commitment. Reliability is what converts one good impression into lasting opportunity.
The “Future of Medicine” Trap: Hiding Behind Observation

There is a modern twist to all this.
You will hear people say, “Surgery is changing. Robotics and AI will do so much. Maybe observation is all we will do someday.”
That is a seductive excuse to stay passive. To stand back, watch the robot arms move, and tell yourself you are being “future‑oriented.”
Here is the problem.
The future of surgery does not need more passive observers. It needs people who:
- Understand anatomy intimately because they have been in the field
- Can manage complications when the robot fails or the plan changes
- Have situational awareness that only comes from active participation
Machines can watch. Algorithms can observe data streams. What they cannot do (yet) is feel tissue tension through your fingers, smell bowel ischemia, or predict the moment a resident is about to tear a vessel because they are pulling the wrong way.
If you spend your training years “just observing,” you will enter that future with no real sensory database. No procedural muscle memory. No credibility.
You will be outcompeted by the person who used every chance to scrub in, retract, close, and own the mundane tasks that build surgical instinct.
How “Just Observing” Bleeds Into Everything Else
This pattern does not stay in the OR. It spreads.
You say:
- “I am just observing on rounds” → you never present patients, so no one trusts you with new consults.
- “I am just observing in clinic” → you never volunteer to see a patient solo, so you never learn to structure a surgical H&P.
- “I am just observing research” → you become a name on a poster, not a first author with actual skills.
Soon your CV is full of half‑engagements:
- Showed up
- Watched
- Left
Residency programs can smell this. Letters that say “X was present and professional” but not “X drove patient care, took ownership, and functioned at the level of a sub‑intern” are a red flag.
You do not want to be the student described as “reliable observer.” That is death by faint praise.
Simple Reframes to Break the “Observer” Identity

| Category | Value |
|---|---|
| Before rounds | 30 |
| In the OR | 40 |
| In clinic | 15 |
| On call | 15 |
Here is how to catch yourself before you fall into the passive trap, and what to say instead inside your own head.
Instead of:
“I am just observing this week.”
Tell yourself:
“I am a junior team member this week. My job is to make myself useful.”
Instead of:
“I do not want to bother them.”
Tell yourself:
“They are adults. If I cross a line, they will tell me. Until then, I will engage.”
Instead of:
“I am not going into surgery, so it doesn’t matter.”
Tell yourself:
“Every specialty respects people who work hard on tough rotations. This reputation will follow me regardless of field.”
Because here is the twist: even if you are headed for radiology, derm, or psych, being “that student who showed up and worked” helps you. The person writing your letter does not care if you match their specialty. They care if you showed that you can do hard things without disappearing.
Advanced Point: The Quiet Line Between Safety and Cowardice
One caveat, because safety matters.
There are times you legitimately should step back:
- Sterile field is cramped and your presence will risk contamination
- Disaster case with too many bodies and not enough space
- Attending explicitly says, “No extra people in this case”
Do not push past those boundaries. That is not ambitious. That is unsafe and makes you look reckless.
The line you are walking is this:
- Respect safety and hierarchy
- But do not pre‑reject yourself from participation before anyone else has said no
Let them tell you, “This one is too tight, you will watch from the corner.”
Do not walk into the room already banished to the corner by your own words.
When you default to “I am just observing,” you are not being safe. You are being cowardly. You are protecting yourself from possible rejection or embarrassment by eliminating the possibility of engagement altogether.
That is the habit that will haunt your whole career if you do not crush it now.
FAQ (Exactly 4 Questions)
1. What if I genuinely am only allowed to observe a case? Should I still avoid saying it?
You can acknowledge the limit without branding yourself as “just an observer.” Say something like, “I understand I will be observing only for this case, but I would like to stand where I can learn the most, and I am happy to help with anything appropriate before or after.” You accept the constraint but still signal seriousness and interest.
2. I am not going into surgery. Does any of this really matter for my future?
Yes. Programs in every specialty read between the lines of your letters. A student described as “actively involved on a demanding surgical service” gets more respect than one described as “present and observant.” Work ethic, initiative, and ability to join a team under pressure are universal currencies. Surgery just exposes your habits faster.
3. I am introverted and anxious. How do I avoid seeming pushy when I engage more?
You do not need to become loud. You need to become clear. Soft‑spoken but direct works very well: “I am the medical student on this case. If it is possible to scrub, I would like to. If not, I will stand where I am not in the way.” You are not demanding; you are simply not hiding. Pair that with consistent, quiet reliability and you will be respected.
4. How do I recover if I have already been “just observing” for a week? Is it too late?
You can pivot. Pull aside a resident you trust and say, “I realize I have been too passive this week. I would like to be more involved—could you tell me how I can be genuinely useful for the rest of the rotation?” Then change your behavior immediately: show up earlier, ask to scrub when appropriate, volunteer for scut that helps the team. People notice turnarounds, and they frequently reward them.
Key points to remember:
Stop introducing yourself as “just observing.” It quietly erases you from the team and your own future opportunities.
Act like a junior team member, not a visitor. Show up, help, and ask for appropriate involvement.
The OR—and your career—belong to the people who step forward carefully, not the ones who hide in the corner and watch.




















