Only 11% of residents on night float get the recommended 7 hours of sleep in a 24‑hour period.
Let me be blunt: night float does not just “shift your schedule.” It dismantles your sleep architecture and then dares you to function as if nothing happened. If you treat it like a minor inconvenience, you will feel terrible, perform worse, and cut ethical corners you never thought you would.
Let’s walk through what actually happens to your sleep stages on night float, how quickly they break, and what you can do—specifically—to protect yourself and your patients.
1. What “Normal” Sleep Architecture Looks Like (So You Recognize When It’s Broken)
Before we talk about night float, you need a clear baseline. Normal adult sleep is not just “8 hours.” It is a structured pattern of stages that repeat in ~90–110 minute cycles.
Roughly, in a normal, healthy, non‑call schedule:
- N1 (lightest sleep): 5–10%
- N2 (intermediate, light non‑REM): 45–55%
- N3 (slow‑wave / deep sleep): 15–25%
- REM: 20–25%
First half of the night: more N3 (deep sleep).
Second half: more REM.
That distribution is not decorative. It maps to specific functions:
- N3: physical restoration, growth hormone release, immune modulation, glymphatic “cleaning,” memory consolidation for factual material. If you keep losing N3, your body breaks first—immune, metabolic, pain thresholds.
- REM: emotional memory processing, procedural learning, mood regulation. If you strip REM, people become irritable, impulsive, cognitively sloppy, and frankly unsafe.
Circadian timing matters. The brain is wired to:
- Put more slow‑wave sleep in the early night (roughly 22:00–02:00)
- Put more REM in the late night / early morning (roughly 03:00–07:00)
So when you “just sleep during the day,” you do not get the same proportions. Your internal clock resists you. Hard.
2. What Night Float Actually Does to Your Sleep Stages

| Category | Value |
|---|---|
| N1 | 15 |
| N2 | 55 |
| N3 | 10 |
| REM | 20 |
On night float, three things hit your sleep architecture simultaneously:
- Circadian misalignment (you are trying to sleep during the brain’s “day”)
- Environmental disruption (light, noise, pages, family life)
- Sleep fragmentation (broken sleep periods, irregular timing)
Here is what I have consistently seen in residents’ sleep (and what lab data backs up).
2.1 Reduced and shifted slow‑wave sleep (N3)
You still get some N3 when you sleep after a night shift. But:
- You get less total N3 than you would at night.
- N3 is delayed and compressed. It does not show up as quickly or last as long.
- If you nap at the wrong times, you further cannibalize what little deep sleep you might get in your main block.
Practical meaning:
Your body never really catches up on physical restoration. DOMS from a single workout lingers for days. Your cold from last week hangs around. That low‑grade “everything hurts and I am 32 going on 82” feeling? That is chronic slow‑wave debt.
2.2 REM gets pushed, fragmented, and often pre‑empted
Remember: REM is naturally weighted toward early morning.
Night float pattern:
- You are working during the natural REM‑rich window (03:00–07:00).
- You try to “replace” that REM when you crash at 08:00 or 09:00.
- Light exposure, short sleep windows, and noise fragment that REM, turning it into useless bits.
So even if your total sleep time seems reasonable (“I got 6.5 hours after shift, what is the problem?”), your REM density and continuity are worse. That is why mood, emotional reactivity, and empathy tank so fast on night float.
2.3 Massive jump in light sleep (N1, N2)
Daytime sleep on night float tends to look like:
- Increased N1 (you are drifting in and out, hyper‑arousable, awaken easily)
- Dominant N2 (the “middle” stage, decent but not truly restorative in large doses)
- Decreased and delayed N3 and REM
Subjectively, this feels like: “I slept but it did nothing.”
2.4 Fragmentation is the real killer
Architecture is not only about percentages. It is about uninterrupted cycles.
Every phone alert, every roommate door slam, every Amazon delivery at 13:00 bounces you out of deeper stages back to lighter sleep or full wakefulness. You keep restarting the cycle from N1 and N2. You never spend sustained time in N3 or REM.
That is why one uninterrupted 5‑hour block on night float is often more restorative than 7 choppy hours broken into bits.
3. Timeline: How Fast Things Break on Night Float

| Period | Event |
|---|---|
| Pre-rotation - Day -2 to 0 | Normal sleep, mild anxiety about nights |
| Early nights - Night 1-2 | Acute sleep loss, high adrenaline, performance preserved |
| Mid-rotation - Night 3-4 | REM reduction, mood lability, cognitive slowing |
| Late rotation - Night 5-7 | Cumulative N3+REM debt, microsleeps risk, errors increase |
A lot of people feel like night float “is not that bad” for the first couple of nights. That is adrenaline and novelty lying to you.
Pattern I see repeatedly:
Nights 1–2
You are tired but wired. You overestimate your functioning. Architecture is already skewed, but debt is small.Nights 3–4
Your sleep drive cranks up. You start having trouble sustaining attention at 04:00–06:00. Mood becomes brittle. This is usually when you snap at a nurse for a perfectly reasonable page.Nights 5–7+
Cumulative N3 and REM debt show up as:- Slowed reaction time
- Decision fatigue
- Short‑term memory errors (“Did I order that CT?”)
- Microsleeps at the computer (terrifying and common)
Most “scary near‑miss” stories I have heard from residents on nights cluster in that day 4–7 window. That is not random.
4. Why This Becomes an Ethical Problem, Not Just a Lifestyle Problem
You are in the “Work Life Balance” bucket, but this is also squarely about medical ethics. Because impaired sleep architecture does not just hurt you. It warps your capacity to be a safe, ethical clinician.
Four very real ethical drifts:
Autonomy – Poor REM and chronic fatigue impair complex communication:
- You cut explanations short.
- You over‑simplify risks to “get consent done”.
- You avoid hard conversations at 05:30 because you do not have the emotional bandwidth.
Beneficence – Fatigue biases you toward “default” or “least effort” decisions:
- You accept prior plans that no longer fit.
- You round superficially at the end of a busy night.
- You postpone re‑evaluating that borderline patient because walking back to the ED is “one more thing.”
Non‑maleficence – Let’s be harsh: running on shredded sleep architecture is a modifiable risk factor for causing harm:
- Dosing errors.
- Failure to notice subtle deterioration.
- Slower recognition of “sick vs not sick.”
Justice – Night float often pushes the most vulnerable clinicians (interns, IMGs, pregnant residents, those with chronic illness) into the most physiologically brutal schedule. Without true choice. That asymmetry is an ethical problem for departments to own.
So no, this is not just “ugh, nights suck.” This is: your sleep architecture is being systematically disrupted in a way that increases risk to patients and strains your ability to uphold your own ethical standards.
You cannot eliminate the problem. You can reduce it. Significantly. But you have to be intentional.
5. Concrete Strategies: How to Protect Your Sleep Architecture on Night Float
This is the part everyone wants, but most advice is garbage like “exercise and hydrate.” Let me narrow this to physiology‑aligned, actually realistic tactics for residents.
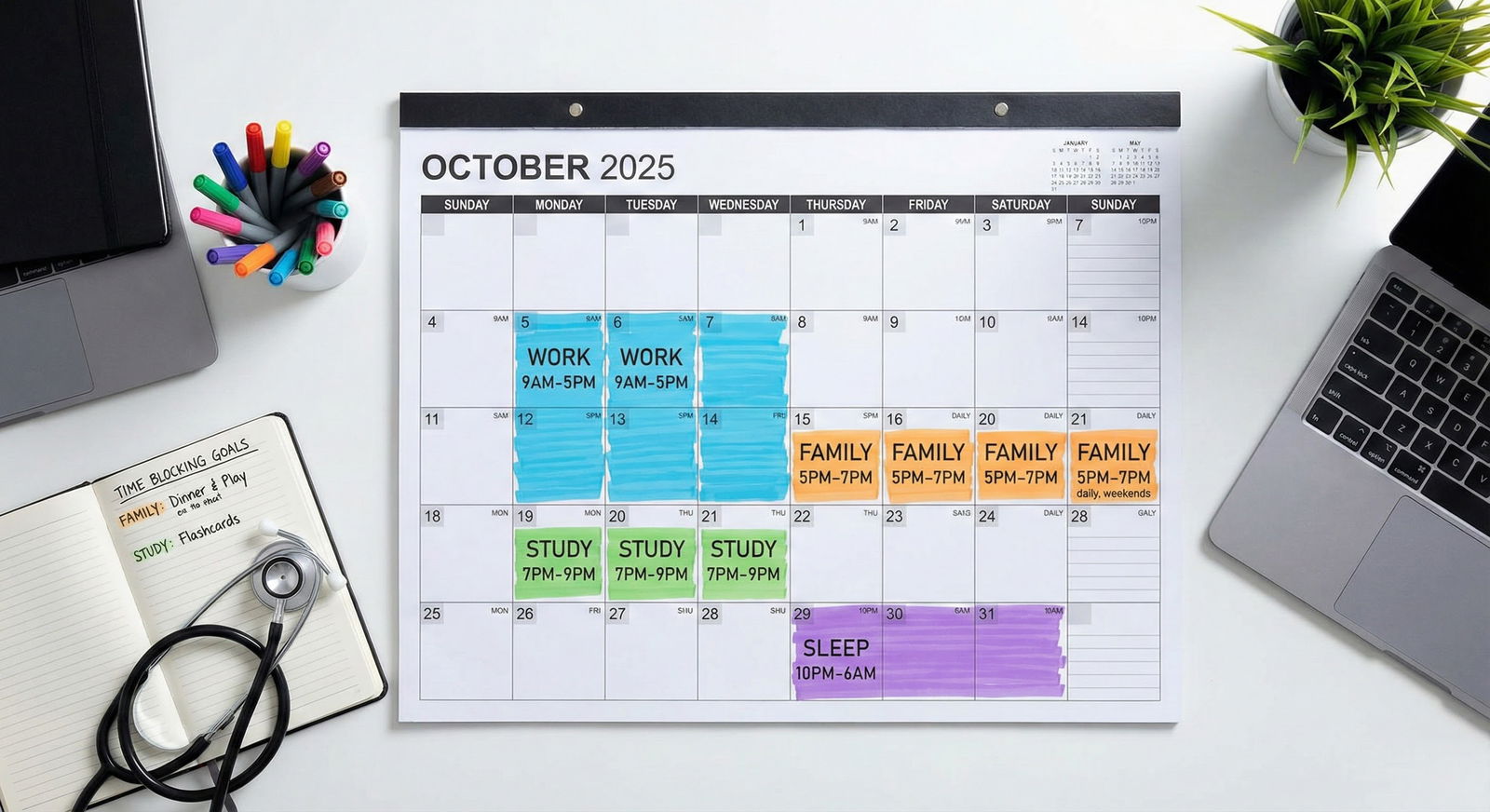
5.1 Before the rotation: shift, but do not wreck your week
Ideal world: you start to delay your sleep by 1–2 hours per night for 2–3 nights before starting nights.
Real world: you have clinic, social commitments, maybe kids. So here is a bare‑minimum, realistic pre‑night shift plan for a 7‑night block starting Monday:
| Day | Bedtime Target | Wake Time Target | Key Action |
|---|---|---|---|
| Friday | 00:00–01:00 | 07:00–08:00 | Mild delay, no naps |
| Saturday | 01:00–02:00 | 09:00–10:00 | Delay, morning light |
| Sunday | 02:00–03:00 | 10:00–11:00 | Plan long afternoon nap |
| Monday | Nap 14:00–17:00 | Wake by 17:00 | Start first night shift |
Focus on two things:
- Push bedtime later by 1–2 hours on the weekend before.
- Protect a solid pre‑shift nap before night 1.
Do not try to invert your schedule fully beforehand. You will just arrive at night 1 already sleep‑deprived.
5.2 During the rotation: protect one main sleep block and stop randomizing your naps
This is where most residents sabotage their architecture without realizing it.
5.2.1 Choose your anchor: post‑shift main sleep vs split sleep
Option A: Single main block
- Shift ends: 07:00–08:00
- Home, blackout, sleep: 09:00–14:00 or 15:00 (5–6 hours)
- Short nap: 18:00–19:00 if needed
Option B: Split sleep (often works better for people with kids or late‑afternoon responsibilities)
- Short post‑shift sleep: 09:00–12:00 (3 hours)
- Second block: 16:00–19:00 (2–3 hours)
Physiologically, I favor Option A for preserving deeper stages. One uninterrupted longer block allows your brain to at least attempt full N3 and REM cycles, even if the circadian timing is sub‑optimal.
Split sleep can work, but only if both blocks are protected from interruption.
The worst pattern:
Random: 09:00–11:00, then 13:00–15:00, then a crash from 20:00–21:00 on some days, and only 10:00–14:00 on others. That constant variability destroys any chance of partial adaptation.
Pick a pattern. Lock it in for the whole rotation.
5.3 Light: the most powerful (and underused) tool you have
You are not going to out‑willpower your suprachiasmatic nucleus. Use light properly or suffer.

| Category | Value |
|---|---|
| Light exposure | 100 |
| Meal timing | 40 |
| Exercise | 30 |
| Social cues | 20 |
5.3.1 On your way home
Goal: Minimize morning light so your brain does not lock onto “day has started, stay awake.”
- Wear dark wraparound sunglasses on the commute home. Yes, even if you feel ridiculous.
- Avoid grabbing coffee after 05:00–06:00. Caffeine plus bright light in the car is a circadian nuke.
5.3.2 At home before sleeping
- Blackout curtains. Not “darkish.” Real blackout. If your room still glows, tape trash bags or cardboard over the window. Residents have done worse.
- Use warm, low‑intensity light inside. No overhead bright LEDs.
- Absolutely no direct sunlight exposure right after leaving the hospital.
5.3.3 Before shift
Here, you flip the script.
- 30–60 minutes of bright light 2–3 hours before your shift (light box or outside).
- Over time, this can nudge your circadian phase slightly later, making night wakefulness less brutal.
If you can only implement one science‑based strategy on nights, fix your light exposure. It shapes your architecture far more than “relaxing music” ever will.
5.4 Caffeine use that does not wreck your later sleep stages
Resident classic: dead until midnight, slam a double espresso at 01:00, heart racing at 08:00, then “I cannot fall asleep during the day, nights are the worst.”
Caffeine half‑life is ~5–6 hours. Quarter‑life ~10–12 hours. You drink 200 mg at 01:00, you still have ~50 mg on board at 11:00–13:00. That light N1/N2, difficulty getting into deep sleep? Not just circadian. Pharmacologic.
Rule set that actually works:
- Stop all caffeine 5–6 hours before end of shift. For a 07:00 sign‑out, last caffeine by 01:00–02:00.
- Front‑load smaller doses earlier: 50–100 mg doses at 22:00, 00:00, 02:00 rather than one 300 mg hit at 02:00.
- Use strategic naps at 02:00–03:00 (even 15–20 minutes) instead of an extra coffee at 04:00–05:00 when microsleeps start creeping in.
5.5 Pharmacologic help: use a scalpel, not a sledgehammer
You will see three main categories used on night float: melatonin, sedative‑hypnotics (zolpidem, etc.), and sedating antidepressants/antihistamines.
Let me be clear: you can easily make your architecture worse if you use these poorly.
5.5.1 Melatonin
Best for shifting the clock, not for “knocking you out.”
For night float:
- 0.5–3 mg taken about 30–60 minutes before your intended daytime sleep.
- Dark environment to let it work.
- Do not chase failed sleep with more melatonin a few hours later; it will not fix fragmentation and may just leave you groggy.
I have seen plenty of residents take 10 mg at 09:00 in a fully lit apartment and then complain melatonin “does not work.” That is not a melatonin failure.
5.5.2 Z‑drugs / benzos
Yes, they can knock you down. They also:
- Distort sleep architecture (suppress REM, alter N3).
- Create dependence if used nightly.
- Impair cognition if residual effects linger into the start of your shift.
If you use them:
- Use the lowest effective dose.
- Use them intermittently, not every single post‑shift day.
- Do not take them fewer than 8 hours before you need to be up and clinically functional.
Frankly, for healthy residents, I am not enthusiastic about routine use. Architecture is fragile enough.
5.5.3 Antihistamines / sedating antidepressants
Diphenhydramine, doxylamine, trazodone, low‑dose mirtazapine. Residents treat these like candy.
Problems:
- Anticholinergic load (bad long‑term, and cognitively dulling).
- Lingering sedation into pre‑shift hours.
- Many of them are blunt instruments for sleep staging.
If you are reaching for these daily, your schedule and environment are usually the bigger problem.
5.6 Environment and boundaries: boring, but decisive
The residents who survive night float best are not the fittest or the most resilient. They are the ones who enforce boring rules.
- Phone on Do Not Disturb with a whitelist (program and family only). Package deliveries can wait.
- White noise or fan to mask daytime noise. Earplugs if tolerable.
- Explicit agreement with roommates/partners: “From 09:00–15:00, I am effectively in another country. Unless the apartment is on fire, I do not exist.”
You are not being “extra.” You are protecting your N3 and REM like critical medications. Because they are.
6. How to Function Ethically When You Are Still Not Sleeping Well
You can do everything right and still feel like trash on night 5. This is where ethical practice under impaired conditions becomes a skill.
6.1 Build cognitive scaffolding for your tired brain
Assume during night float that:
- Your working memory is degraded.
- Your attention is spotty.
- Your error detection is slower.
Compensate explicitly:
- Use checklists for high‑risk tasks: sign‑out, ICU transfers, code carts, post‑op orders.
- Force yourself to do a brief “10‑second check” before every high‑risk order: drug, dose, route, patient.
- Offload memory to the EMR or a pocket note; do not trust “I will remember to follow up that troponin.”
6.2 Increase team transparency about fatigue
The unhealthy culture: everyone pretends they are “fine” because nights are “just part of training.”
The better culture (that you can help build):
- State out loud on sign‑out: “It is my fifth night in a row, I am more tired than usual; I may be slower, so please double‑check me on dosing.”
- Encourage nurses to call if “something feels off” with your orders. Make that an explicit invitation.
You do not win points for hiding fatigue. You increase risk.
6.3 Know your personal danger window
Most people have a brutal dip somewhere between 03:00 and 06:00. That is when reduced REM, high sleep pressure, and circadian nadir all collide.
During that window:
- Avoid starting complex, non‑urgent tasks (e.g., building an elaborate multi‑step order set you could do at 01:00 instead).
- Choose checklists over free‑form.
- If you catch yourself re‑reading notes multiple times, that is a red flag. Pause. Stand up. Walk. Reorient.
If you feel your eyes snap shut at a workstation for even a second, that was a microsleep. You are not “a little tired.” You are physiologically unsafe. Ask a colleague to cover for a 10–15 minute nap if at all possible.
7. After Night Float: Repair, Do Not Whiplash
Most residents make the same mistake after their last night: they try to be “normal” the next day and end up wrecking their recovery.

7.1 The classic bad pattern
Last night ends at 07:00. You go home, decide to “stay up all day so I can sleep at night,” feel horrific by 15:00, crash on the couch for 3 hours, then cannot fall asleep before 02:00. You spend 3–4 days half‑adjusted and miserable.
7.2 A better taper‑off strategy
For a 7‑night block finishing Friday morning:
- Sleep a shorter block after your last night: 09:00–12:00 or 13:00. Set an alarm.
- Get up, go outside, bright light exposure in afternoon. Mild activity.
- Target a relatively late but still “normalish” bedtime: 22:00–23:00.
- Accept that you will still feel like you have jet lag for 48–72 hours. Do not schedule important exams, big family events, or major decisions this weekend if you can avoid it.
Your architecture will take a few days to re‑consolidate. Let it.
8. Program‑Level Changes: What You Should Advocate For
You are not powerless here. Many programs simply have not thought about sleep architecture beyond ACGME hour limits.
Reasonable, evidence‑aligned asks:
- Cap consecutive night float shifts (e.g., 5–7 nights) with guaranteed recovery days.
- Standardize shift times so your body can at least partially adapt; random 19:00–07:00 then 21:00–09:00 rotations are unnecessary cruelty.
- Napping norms: explicit permission and expectation of short off‑duty naps during low‑acuity periods. This is basic fatigue risk management.
- Access to a proper nap room: dark, quiet, no pager noise, close to main work areas. Call rooms that double as storage closets do not count.
- Formal education on sleep and fatigue as part of professional ethics and patient safety curriculum, not just an optional wellness talk.
When you frame this as a patient safety and ethics issue, not a “millennial wellness” issue, leadership is more likely to listen.
FAQ (Exactly 6 Questions)
1. Is it better to stay on a night‑shift schedule on my days off or flip back to normal days?
For a short block (≤7 nights), it is usually better to partially flip back on days off so you can handle essential life tasks. For longer blocks (2–4 weeks of nights), staying closer to a nocturnal pattern even on days off can help your circadian system stabilize, but that is often impractical socially. The worst option is random oscillation: staying up all day one off‑day, then sleeping till 16:00 on the next. Mild, predictable adjustments beat chaos.
2. Are “sleep trackers” or smartwatches useful for monitoring my sleep architecture on night float?
They are decent for tracking total sleep time and general consistency. They are terrible at precisely measuring N3 or REM in a clinical sense. Use them to see patterns (“I slept 4.5 hours, fragmented, three days in a row”) rather than to obsess over exact stage percentages. If the watch says you got 7 hours but you feel wrecked, trust your body, not the gadget.
3. If I can only change one thing during night float, what has the biggest payoff?
Light management. Dark glasses after work, blackout room for day sleep, and bright light before your shift. It reshapes your circadian drive and indirectly improves how much valuable N3 and REM you get in that daytime block. That single intervention is more powerful than every supplement your co‑resident will recommend combined.
4. Is it ever acceptable to use stimulants beyond caffeine to get through nights?
Using prescribed stimulants (e.g., for ADHD) is one thing. Using non‑prescribed stimulants to compensate for self‑inflicted sleep deprivation is an ethical and safety problem. You are masking fatigue signals that exist to protect patients. You may feel sharper while your fine judgment and emotional regulation are actually worse. If you consistently “need” stimulants just to function at baseline on nights, your schedule, sleep strategy, or workload is the issue—not a stimulant deficiency.
5. How do I handle night float if I already have a sleep disorder like insomnia or delayed sleep‑wake phase?
You need a tailored plan. That usually means involving occupational health or a sleep specialist and, frankly, advocating for reasonable accommodation in your schedule. For some, night float is slightly easier (delayed phase), for others it is brutal (insomnia, circadian rhythm disorders). Pushing through “like everyone else” is how you end up severely decompensated. Documented conditions deserve structured support, not stoicism.
6. What are red‑flag signs that my sleep on night float is becoming dangerous, not just uncomfortable?
Three big ones: 1) repeated microsleeps (brief head nods) at the computer or in conference, 2) near‑miss clinical errors you only catch by luck or by someone else, and 3) marked mood changes—rage, tearfulness, or numbness that feels alien to you. If those show up, you are beyond “normal tired.” You need immediate adjustments: protected naps, help from co‑residents, possibly stepping out of clinical duty briefly. Ignoring those signs is how bad outcomes happen.
Key takeaways: Night float does not just shorten your sleep; it distorts your sleep architecture—especially N3 and REM—in ways that directly affect cognition, mood, and ethics. You cannot make nights healthy, but with structured light management, consistent sleep scheduling, and ruthless protection of one main sleep block, you can make them significantly safer for you and your patients.



















