
The myth that burnout is just a “mid-year slump” in intern year is wrong. It spikes in predictable waves, and if you do not prepare for them month by month, they will steamroll you.
I am going to walk you through intern year chronologically. Not theory. The actual emotional and physical pattern most interns live: when it gets dark, when it gets dangerous, and what you should be doing at each point so you do not torch your career or your sanity.
Big Picture: The Burnout Curve of Intern Year
Before we go month-by-month, you need the map.

| Category | Value |
|---|---|
| July | 4 |
| Aug | 6 |
| Sep | 7 |
| Oct | 8 |
| Nov | 9 |
| Dec | 9 |
| Jan | 8 |
| Feb | 7 |
| Mar | 7 |
| Apr | 6 |
| May | 5 |
| Jun | 4 |
Here is the pattern I see over and over:
- July–August: Adrenaline + anxiety. Tired but motivated. Burnout smoldering, not yet raging.
- September–October: Reality sets in. Errors, feedback, fatigue. First serious doubts.
- November–January: Peak burnout. Holidays on call, cumulative sleep debt, moral distress, loneliness.
- February–March: Adaptive phase. You get more efficient or you crumble.
- April–June: Late-year fatigue but also control. Thinking about PGY-2, moving, next steps.
June: Pre-Intern Year – Set Your Systems Before the Fire Starts
Burnout prevention does not start in July. If you wait until orientation, you are already behind.
At this point you should:
Lock in basic life logistics.
- Housing close enough to walk or with a reliable commute.
- Automatic payments set for rent, loans, utilities. You will forget otherwise.
- Backup transport plan for post-call (Uber budget, partner pickup, etc.).
Design your “minimum viable life” rules. You need non-negotiables. Not goals. Rules.
- Sleep floor (example: “Never less than 5 hours unless actively on call.”).
- Food rule (“No 24-hour period with zero real meals. I can snack, but I must sit for 10 minutes at least once.”).
- Communication rule (“Daily check-in text with partner/friend no matter what, even if just a ‘still alive’ message.”).
Clarify your ethical backbone. You will be pressured—subtly or openly—to cut corners.
- Write down 3 lines you will not cross. Example:
- “I will not falsify vitals or exam findings in the chart.”
- “I will escalate safety concerns even if the resident seems annoyed.”
- “I will not ignore a patient explicitly asking for help because ‘they always do that.’” Put it in your phone notes. When you are exhausted at 2 a.m., you need pre-committed ethics, not abstract values.
- Write down 3 lines you will not cross. Example:
Create a burnout “distress signal” plan. Decide:
- Who will you tell first if you start thinking, “I hate this, I may have made a mistake”?
- What are your local resources? (GME mental health, resident support, chaplaincy, employee assistance programs).
- What early warning signs you want others to watch for (irritability, missing meals, isolating).
You are building a safety harness before climbing. Do it now.
July–August: Orientation High, Anxiety Underneath
Early intern year is deceptive. You are terrified, yes, but you are also energized. Everyone checks on you, co-signs your orders, tells you “Ask anything, that’s why you are here.” Support feels abundant.

| Period | Event |
|---|---|
| July | Orientation, shadowing, first calls |
| Late July | First independent nights |
| Early August | Start to recognize patterns |
| Late August | Decreasing supervision intensity |
At this point you should:
Obsess over systems, not speed. Burnout later is fueled by chaos now.
- Build your own admission checklist (in a note or template). Use it every time.
- Create a “sign-out script” and stick to it.
- Standardize your pre-rounding routine by the end of July.
Your goal: by August 31, you do not reinvent your workflow every shift.
Actively practice saying, “I need help.” You are never more allowed to ask “too many questions” than in July.
- Force yourself to ask at least one clarifying question on each new admit.
- Say out loud: “Before I go home, anything else you need from me?” to your resident. That verbal habit will save you in October when shame starts muting you.
Start a simple reflection habit. Five bullet points in your phone after each shift:
- 1 thing you did well
- 1 clinical question to look up
- 1 moment that bothered you ethically
- 1 thing you will do differently tomorrow
- 1 thing you are grateful for
Do not write essays. You are training situational awareness about your own moral and emotional state.
Protect your off-day like an ICU bed. One full day off should actually be off.
- No “just swinging by” the hospital.
- No major life admin beyond what is truly urgent.
- One thing purely for pleasure, not productivity.
If you think you are “handling it fine” right now: good. Bank that confidence, but do not get arrogant. The real test has not started.
September–October: Competence vs. Exhaustion Clash
This is where many interns hit their first major dip. The novelty is gone. The learning curve is still steep. Supervision feels lighter. You have had your first error or near-miss. And the call schedule starts to wear grooves into your body.
At this point you should:
Tighten your sleep discipline ruthlessly. You cannot “catch up” on sleep exclusively on weekends. That fantasy dies here.
- Set a hard bedtime window on non-call nights (for example, 10:30–11:30 p.m.).
- Create a 15–20 minute decompression ritual: shower, no screens, dim lights.
- Use earplugs and a sleep mask without apology. Your neighbors do not care about your wellness.
Burnout peak in December is heavily seeded by sleep debt in September–October.
Audit your daily time like an attending audits notes. For one week, track:
- Arrival time, departure time
- Actual time on direct patient care vs. notes vs. scut
- Time wasted on avoidable tasks (looking for forms, re-entering data, chasing labs you could have auto-paged)
Then cut:
- One unnecessary daily task (for example, double-checking something you can safely check once).
- One self-imposed perfection habit (writing novel-length notes when concise is enough).
Recognize the “quiet moral injuries.” Around now you start to see:
- Patients boarded in hallways for days.
- Discharges driven by bed pressure rather than patient readiness.
- Language used by staff that dehumanizes patients.
Your ethical burnout often precedes your emotional burnout. Make a rule:
- When something feels wrong:
- Name it in your head (“This feels like premature discharge.”).
- Ask one question (“Is there any flexibility on keeping them one more night?”).
- Debrief with someone you trust before going home (“That case did not sit right with me.”).
Silence + shame is gasoline on burnout.
Decide your social minimums. You cannot be at every dinner, every birthday, every call home. But you can pick:
- Weekly: One real conversation (20+ minutes) with someone outside medicine.
- Monthly: One meal or event that has nothing to do with the hospital.
If you feel yourself thinking, “Everyone else seems fine, maybe I am just weak”: you are not. They are just not talking about it.
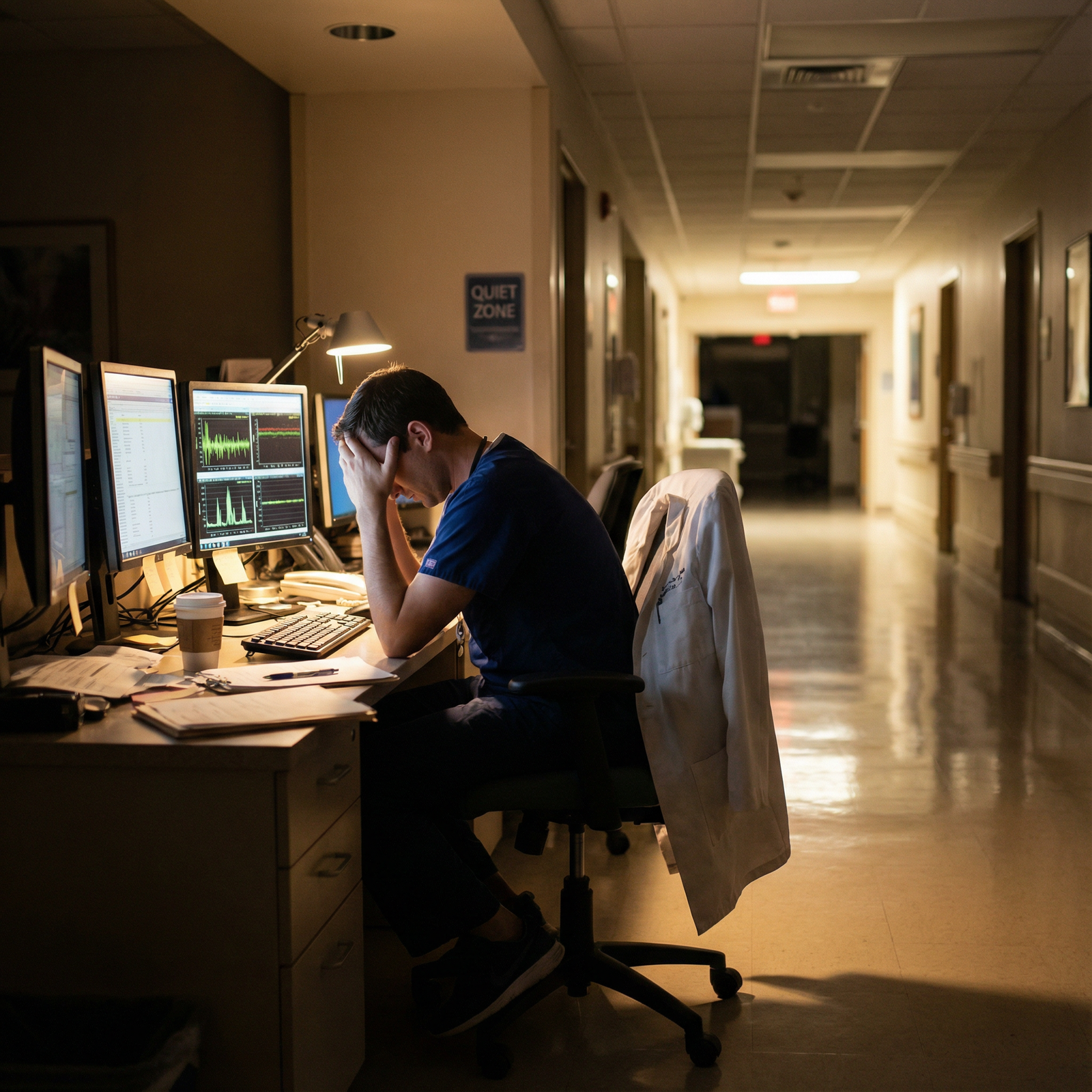
November–January: The Burnout Peak (Holidays, Darkness, Doubt)
This is the danger zone. Short days, back-to-back holidays on call, flu season, staffing shortages, and cumulative emotional debris from the first half of the year. Suicidal ideation in trainees spikes here. I have seen residents quietly disappear for “leave” that everyone knows was a breakdown.
At this point you should:
Lower the bar on everything except safety. You cannot be a perfect doctor, perfect partner, and perfect friend while on back-to-back holiday calls. Choose.
- Non-negotiable: Safe orders, timely critical actions, truthful documentation.
- Flexible: Perfectly written notes, elaborate differentials for straightforward cases, volunteering for extra committees or projects.
If something must slip, let it be reputation for “always saying yes,” not patient safety or your mental health.
Name your burnout level honestly every week. Use a simple 0–10 scale for yourself:
- 0–3: Tired but stable
- 4–6: Edgy, cynical, but functioning
- 7–8: Purposeless, detached, maybe hopeless
- 9–10: Daily thoughts like “If I got hit by a bus, it would be a relief.”
When you hit 7 or higher for more than two weeks:
- Tell someone in your program explicitly (chief, PD, trusted attending).
- Contact mental health support (resident clinic, therapist).
- Strip away nonessential commitments (research meetings, teaching extras) for at least one month.
This is not weakness. This is maintenance.
Guard against ethical numbing. Classic signs right now:
- Referring to patients only as “the GI bleed” or “the drunk in 12”.
- Laughing at things that actually disturb you.
- Stopping yourself from feeling sad when a patient you liked dies.
You do not need to be a wreck, but you must stay human.
- Once a week, choose one patient and learn one personal detail (job, favorite food, who they live with).
- Allow yourself a small ritual after a death: a 10-second pause, a step outside, a brief note in your reflection log.
Create “tiny joys” on call. Massive self-care will not happen when you are cross-covering 60 patients. Aim small, repeatable:
- Your favorite snack only on night shifts.
- A 60-second stretch or walk at the top of every hour overnight.
- One song you play walking into night float to mark the transition.
Plan one concrete break after this stretch.
- Block a post-holiday weekend in February or March as completely as your schedule allows.
- Mark it on your calendar now. Mentally walk toward it.
If you find yourself thinking “I do not care what happens to these patients,” treat that as a red-alert symptom the same way you would treat chest pain in a 60-year-old smoker.
February–March: Adaptation or Collapse
By late winter, something shifts. You either:
- Become more efficient, set better boundaries, and build resilience, or
- Slide into a bleak, chronic burnout that becomes your new normal.

| Category | Direct Care (hrs/day) | Documentation (hrs/day) | Inefficiency/Scut (hrs/day) |
|---|---|---|---|
| July | 3 | 6 | 3 |
| Jan | 4 | 5 | 2 |
| May | 4 | 4 | 1 |
At this point you should:
Streamline your work deliberately.
- Cut chart review bloat. You do not need to read every note from 2015.
- Use templates intelligently, not lazily. Default smart phrases that still allow individualized key details.
- Batch tasks: write all discharge instructions in one block, then call all families, then finish orders.
Every 30 minutes saved is another 30 minutes you are not hating your life at 8 p.m.
Renegotiate your identity. Many interns feel a quiet identity crisis now:
- “I used to be top of my class; now I just feel like a tired order machine.”
- “I am not as compassionate as I thought I was.”
Response:
- Stop comparing yourself to med school. That was performance; this is practice.
- Choose 1–2 qualities you still want to embody (for example, curiosity, honesty) and measure yourself by those, not by productivity or constant cheerfulness.
Revisit your ethical backbone list.
- Have you crossed any of your lines under pressure?
- Have you watched others cross them and stayed silent?
If yes:
- Acknowledge it without sugarcoating.
- Decide how you will respond next time (what you will say, who you will call).
- If it still weighs on you, consider a confidential conversation with an ethics committee member, chaplain, or trusted attending.
Invest in one non-medical part of your life. Burnout thrashes hardest when medicine is 100 percent of your identity.
- Pick something tiny but consistent: language app, weekly run, book club, instrument.
- Minimum: 10 minutes, 3 times a week.
You are not “fixing” burnout here. You are rebalancing the equation so that work is not the only variable.
April–June: Late-Year Fatigue and Future Anxiety
By spring, you are more competent. You get called less frantically. Nurses trust you more. New anxiety emerges: the next step. PGY-2. Fellowships. Maybe switching specialties. Meanwhile, you are just tired.

At this point you should:
Do a full-year burnout debrief. Take one quiet afternoon off and ask:
- What were my three lowest points this year?
- What patterns led there? (sleep, workload, isolation, specific rotations)
- What actually helped? (a specific mentor, therapy, a schedule change, a boundary)
- What did not help at all but I kept doing? (doomscrolling, venting in group chats without action, saying yes to every shift swap)
Write it down. Use it to plan PGY-2.
Adjust your ethical compass for the long game. You have now seen the system’s uglier parts.
- Decide: Will you become indifferent, or will you choose specific battles you will actually fight? Examples:
- You cannot fix hospital boarding, but you can fight for safe discharges.
- You cannot fix every scheduling injustice, but you can protect interns under you from bullying.
Choose 1–2 small ethical commitments for next year:
- “I will never ignore a nurse’s concern about a patient, even if I feel annoyed.”
- “I will not mock patients in front of students.”
Prepare your PGY-2 support structure now. You will have more responsibility and sometimes less formal support.
- Identify 2–3 attendings you respect. Tell them: “I value your perspective; can I continue to reach out next year?”
- If you are changing services (for example, prelim → advanced program), research mental health resources at the new site now.
Clean up your life admin backlog. Burnout is worsened by the constant hum of neglected tasks. In May–June:
- Handle health maintenance: your own PCP, dentist, therapy intake if needed.
- Tackle financial basics: consolidate loan info, set up auto-pay, basic budget.
- Declutter your physical space: you cannot start PGY-2 in a trash heap.
Rebuild a small sense of meaning. Go back through your short reflections from the year (if you kept them).
- Highlight 3–5 moments when you actually helped someone or felt proud.
- Keep those somewhere visible (phone background, printout near your desk).
Burnout erases your memory of why you started. You have to re-insert it deliberately.
Ethical Red Flags: When Burnout Becomes Dangerous
Burnout is not just “tired and cranky.” It becomes an ethical and safety problem when:
- You start cutting corners you know are unsafe.
- You feel actively hostile toward certain patient groups.
- You avoid disclosing errors because you “just cannot deal with it.”
- You fantasize about something bad happening to you so you would be forced to stop working.
| Red Flag | Action Within 48 Hours |
|---|---|
| Persistent 7–10 burnout score | Contact mental health, tell a peer |
| Passive suicidal thoughts | Reach out to crisis/therapist/PD |
| Repeated unsafe shortcuts | Debrief with attending or chief |
| Increasing substance use to cope | Seek confidential support program |
| Total emotional numbness toward all patients | Schedule professional support |
If you see these in yourself, this is non-negotiable: you must tell someone. Chief resident, program director, therapist, trusted attending. Do not talk yourself out of it with “Others have it worse.” That logic kills residents.
Final Step: What You Should Do Today
You do not need a grand plan. You need the next concrete move.
Today, before you forget, do this:
Open your phone and create one note titled “Intern Year Burnout Plan.”
Add four headings: June Prep, Early Months, Holiday Peak, Late-Year. Under each, write one specific action from this guide that you commit to using. One per phase. Not ten.
You can revise later. But start the map now, while you still have the energy to care.



















