The popular narrative about burnout is lazy. “Everyone’s burned out.” “It’s just depression from work.” That’s not what the data show—and pretending burnout is just depression in disguise is bad science and even worse policy.
Let’s be blunt: burnout and depression overlap, but they are not the same thing. Conflating them has turned into a convenient excuse for institutions and a trap for clinicians who start thinking their distress is purely a personal weakness or a serotonin issue.
You deserve a clearer answer than that.
What Burnout Actually Is (And Is Not)
First, definitions. If we can’t define the thing, we definitely can’t treat it.
The classic model of burnout comes from Christina Maslach’s work. She and others describe burnout as a work-related syndrome with three main components:
- Emotional exhaustion – feeling used up, drained, unable to give more at work.
- Depersonalization (or cynicism) – treating patients or coworkers like objects, distancing yourself, becoming sarcastic or bitter.
- Reduced personal accomplishment – feeling ineffective, like nothing you do matters or works.
Depression, on the other hand, is a clinical mood disorder defined by criteria like:
- Persistent low mood or loss of interest/pleasure.
- Sleep changes, appetite changes, low energy.
- Poor concentration, guilt, hopelessness.
- Suicidal thoughts or behavior.
Depression shows up across all life domains: home, work, hobbies, relationships. Burnout is supposed to be specifically tied to the work context.
Notice the word “supposed.” In real life, things blur. Work stress bleeds into home, home stress bleeds back, and many clinicians don’t turn off their brain at the door.
But the conceptual difference matters. Burnout is about the relationship between a person and a toxic or mismatched work environment. Depression is about a broader disturbance in mood, biology, and thinking—often independent of job conditions.
What the Research Actually Shows About Overlap
You’ve probably heard some version of: “Burnout is just workplace depression.” That line gets repeated because it sounds neat and simple. It also happens to be only half true.
Let me walk you through what the literature says.

| Category | Value |
|---|---|
| Burnout Only | 40 |
| Both Burnout & Depression | 35 |
| Depression Only | 25 |
Those numbers aren’t from a single definitive paper—they approximate what many meta-analyses and large cohorts converge on:
- A chunk of people have burnout symptoms without meeting criteria for depression.
- Another chunk meet criteria for depression and also look burned out.
- A third group is depressed irrespective of work.
Specific findings:
- Systematic reviews on physicians and nurses routinely find moderate correlation between burnout scales and depression scales—often around r = 0.5–0.6. That’s overlap, not identity. For context, height and weight correlate too; that doesn’t mean they’re the same construct.
- Studies that use the Maslach Burnout Inventory (MBI) plus standard depression scales (PHQ‑9, Beck Depression Inventory, etc.) consistently show:
- Plenty of people high on emotional exhaustion but not meeting depression criteria.
- Strong associations between exhaustion and depressive symptoms—but weaker or inconsistent links for depersonalization and personal accomplishment.
Translation: the “tired, drained, can’t do this anymore” part of burnout tracks closely with depressive symptoms. The “cynical, detached, my work is pointless” pieces behave differently and are more specifically work-linked.
When researchers run factor analyses (the statistical tool you use to see if items form distinct constructs), they often find:
- Burnout items and depression items cluster into related but separable groups.
- Emotional exhaustion tends to “lean” toward depression, but depersonalization and low accomplishment form their own patterns.
So no: burnout is not just misdiagnosed depression. It’s messier.
Why The “It’s All Depression” Story Is So Appealing (and So Wrong)
Here’s the uncomfortable part. A lot of people—especially administrators and some clinicians—want burnout to be the same as depression. For different reasons.
If burnout = depression, then:
- For organizations: it becomes an individual medical issue. You send people to therapy, maybe hand out an app subscription and a meditation room, check some wellness box, and keep RVU expectations the same.
- For clinicians: there’s a familiar narrative—“I’m mentally ill, I should medicate/therapy my way out”—and less pressure to confront the reality that your work environment is structurally harmful.
The data do not support that simplification.
Key differences the evidence keeps showing:
Burnout is more strongly tied to job conditions than personal traits.
High workload, lack of control, administrative burden, moral distress, poor staffing, electronic health record chaos—these are the strongest predictors of burnout scores. Personality traits and “resilience” measures have effects, but they’re smaller.Depression doesn’t drop simply by changing shifts or clinics.
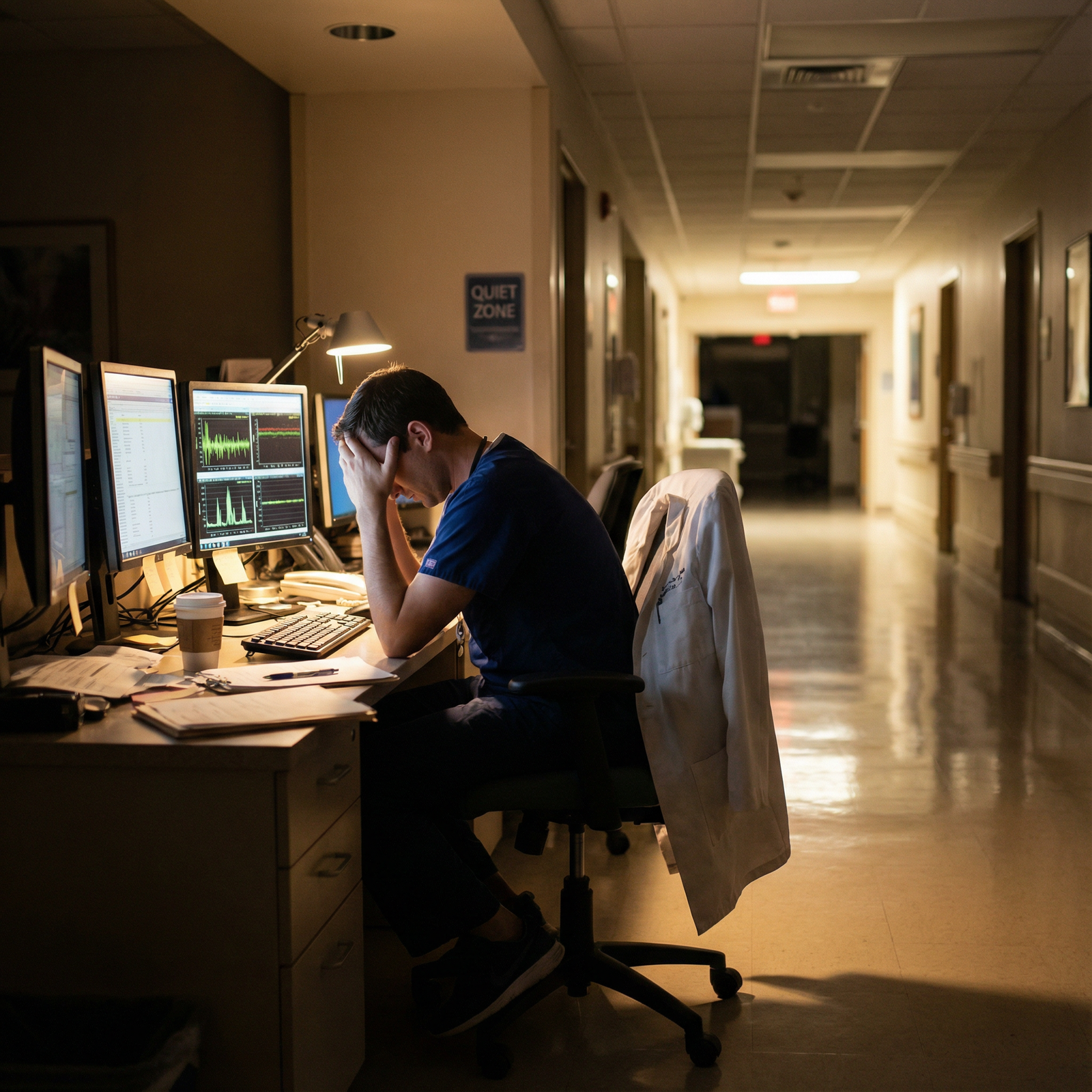
I’ve seen physicians move to a different service, cut hours, or change jobs and watch their burnout score nosedive, while their underlying depression symptoms or anxiety barely budge. And vice versa.Burnout clusters in units and specialties; depression clusters in people.
ER teams, ICU nurses, EM residents, or primary care docs in certain systems show very high burnout as a group. Depression rates climb somewhat, but not in lockstep. If burnout were just depression, you’d expect more exact parallels.
| Predictor | Stronger Link To | Weaker Link To |
|---|---|---|
| Excessive workload | Burnout | Depression |
| Loss of autonomy/control | Burnout | Depression |
| Moral injury / ethical conflict | Burnout | Depression |
| Prior personal mental health hx | Depression | Burnout |
| Supportive leadership | Burnout | Depression |
None of this says depression is irrelevant to burnout. They reinforce each other. But treating them as identical is like saying “hypertension is just anxiety in disguise” because both raise your heart rate.
That’s not analysis. That’s laziness.
Moral Injury: The Elephant Everyone Keeps Relabeling
Another piece most simplistic “burnout = depression” takes ignore: moral injury.
Moral injury is what happens when you’re repeatedly forced to act (or prevented from acting) in ways that violate your core values—for instance:
- Discharging a patient earlier than is safe because insurance won’t pay.
- Rushing through 20 visits in a morning knowing you’re missing things.
- Watching systems prioritize metrics over actual care.
This isn’t about serotonin. It’s about ethics.
Plenty of burned-out clinicians don’t say, “I feel sad.” They say things like:
- “I feel like a cog in a scam.”
- “I can’t give the care I know is right.”
- “I’m constantly choosing between my conscience and my job.”
That’s moral injury. It expresses as burnout—cynicism, exhaustion, detachment—but its root is ethical, not exclusively psychological.
And here’s the kicker: treating moral injury as depression is almost insulting. It pathologizes your appropriate reaction to a broken system.
The Clinical Risks of Mislabeling Burnout as Depression
This isn’t just semantics. Mislabeling has consequences.
If burnout is treated as nothing but depression, several bad things tend to happen:
Under-diagnosis of real depression.
People who truly meet criteria for major depressive disorder get waved away as “just burned out” and told to do yoga, use the wellness app, or take a long weekend. Their suicidal ideation gets minimized as “work stress.”Over-medicalizing normal outrage.
If your system is abusive—unsafe ratios, impossible documentation loads, chronic understaffing—feeling exhausted and angry isn’t a disease. It’s an appropriate human response. Labeling that as “mental illness” lets the system off the hook.Self-blame ramps up.
When you internalize the idea that this is “your depression,” you start thinking: “If I were stronger, more grateful, more resilient, I’d be fine.” Meanwhile, the schedule is inhumane and the culture rewards self-neglect.Solutions target the wrong level.
Individual psychotherapy and SSRIs are appropriate for depression. They’re not structural fixes for garbage EHR design, punitive productivity metrics, or leadership hostility.
Let me be clear: if you think you might be depressed, you should absolutely seek proper assessment and care. Mental health treatment is not optional in this profession anymore; it’s survival gear.
But don’t let anyone gaslight you into believing that systemic abuse is just a neurochemical glitch in your head.
How Studies Distinguish Them (When Done Correctly)
The better-designed studies do a few key things:
- Use validated burnout scales (like the full MBI, not the butchered two-item versions) and validated depression scales (PHQ‑9, HADS, BDI).
- Treat them as separate but correlated variables, not synonyms.
- Analyze how changes in work conditions affect each over time.
Patterns that emerge:
- Interventions that target workload, workflow, autonomy often reduce burnout scores significantly while having a smaller or delayed impact on clinical depression.
- Purely individual-focused interventions (mindfulness courses, resilience training) may boost coping or lower depressive symptoms moderately, but they barely touch burnout if the environment remains toxic.

| Category | Value |
|---|---|
| Systemic workflow changes | 45 |
| Schedule flexibility | 30 |
| Mindfulness courses | 15 |
| Mandatory wellness modules | 5 |
Again, those numbers are an illustration, but they align with the general pattern in the literature: system-level changes > schedule tweaks > individual coping hacks > performative wellness nonsense.
Guess which tier most institutions invest in first? Exactly.
So What Do You Actually Do With This?
You don’t need another inspirational poster about self‑care. You need a clear map of what’s what.
1. Screen Yourself for Both—Separately
Basic litmus tests (not a replacement for clinical evaluation, but a start):
If your mood is low across all areas of life, you’ve lost interest in things you used to enjoy, sleep and appetite are off, and this has persisted for weeks to months: that’s waving a depression flag, whether or not you’re burned out.
If you feel most terrible when thinking about or doing work, and notice:
- Dread on the commute.
- Emotional numbness with patients.
- Counting the hours constantly.
Then burnout is in play, whether or not you’re clinically depressed.
And yes, you can have both.
2. Match the Intervention to the Problem
- For depression: evidence-based therapy, medications when indicated, actual time off, social support, and removing acute stressors where possible.
- For burnout: negotiate workload, change practice settings, reduce non-clinical garbage, find leadership that isn’t tone deaf, or in some cases, change careers.
One more hard truth: “Building resilience” is not a cure for being systemically overused. You don’t fix a gas leak by meditating in the kitchen.
3. Stop Letting Systems Hide Behind The Word “Burnout”
“Burnout” became a convenient term because it implies an almost mechanical failure—like a light bulb burning out after too many hours. It sounds impersonal. Nobody is at fault; the system is “just stressful.”
Moral injury and depression don’t let people off so easily.
- If your distress stems from being forced into ethically unacceptable compromises—that’s moral injury.
- If your functioning across life is collapsing—that’s depression and needs treatment.
- If your energy and engagement have been drained primarily by chronic, fixable work conditions—that’s burnout, and the conditions need to change.

| Step | Description |
|---|---|
| Step 1 | Work Conditions |
| Step 2 | Moral injury |
| Step 3 | Burnout |
| Step 4 | Exhaustion and cynicism |
| Step 5 | Possible depression |
| Step 6 | Primarily work related |
| Step 7 | Ethical conflict? |
| Step 8 | Unsustainable workload? |
| Step 9 | Symptoms across life? |
This is not perfect, but it’s closer to reality than “everything is depression.”
Why This Matters for Medical Ethics
You said this is about personal development and medical ethics. Good. Because the ethical dimension is the part most wellness campaigns sidestep.
Three ethical problems with calling burnout “just depression”:
It individualizes a systemic harm.
Saying “you are depressed” instead of “this system is harming you” moves blame from the organization to the physician. Ethically lazy.It normalizes unsafe practice.
If a whole department is “depressed,” apparently for no reason, the work model itself gets a pass. Burnout data, when properly interpreted, are often evidence of organizational misconduct or neglect.It silences moral protest.
Clinicians’ anger and distress over unsafe, unethical conditions are a kind of whistleblowing. Pathologizing that as “mental illness” is a way to discredit the message by treating it as a symptom.
Your responsibility isn’t only to take care of yourself (though you do have that duty). You also have a professional duty to recognize when the structure you’re in is incompatible with safe, humane care—and to say so.
That starts with refusing to let sloppy language blur the line between personal psychopathology and systemic pathology.

| Category | Value |
|---|---|
| System Factors | 55 |
| Individual Vulnerability | 25 |
| Moral Conflict | 20 |
The Bottom Line: Burnout vs Depression
Let me strip this down to the essentials.
Burnout and depression overlap but are not identical. Burnout is a work-related syndrome heavily driven by system conditions; depression is a broader clinical disorder. Emotional exhaustion sits in the middle and overlaps with both.
Calling burnout “just depression” is scientifically sloppy and ethically dangerous. It hides structural harm behind individual pathology, under-treats real depression, and over-medicalizes appropriate outrage at broken systems.
Your strategy has to match the problem. Treat depression with proper mental health care. Address burnout by changing the work environment or your relationship to it. And do not confuse moral injury—your conscience screaming that something is wrong—with a personal defect you’re supposed to medicate away.



















