
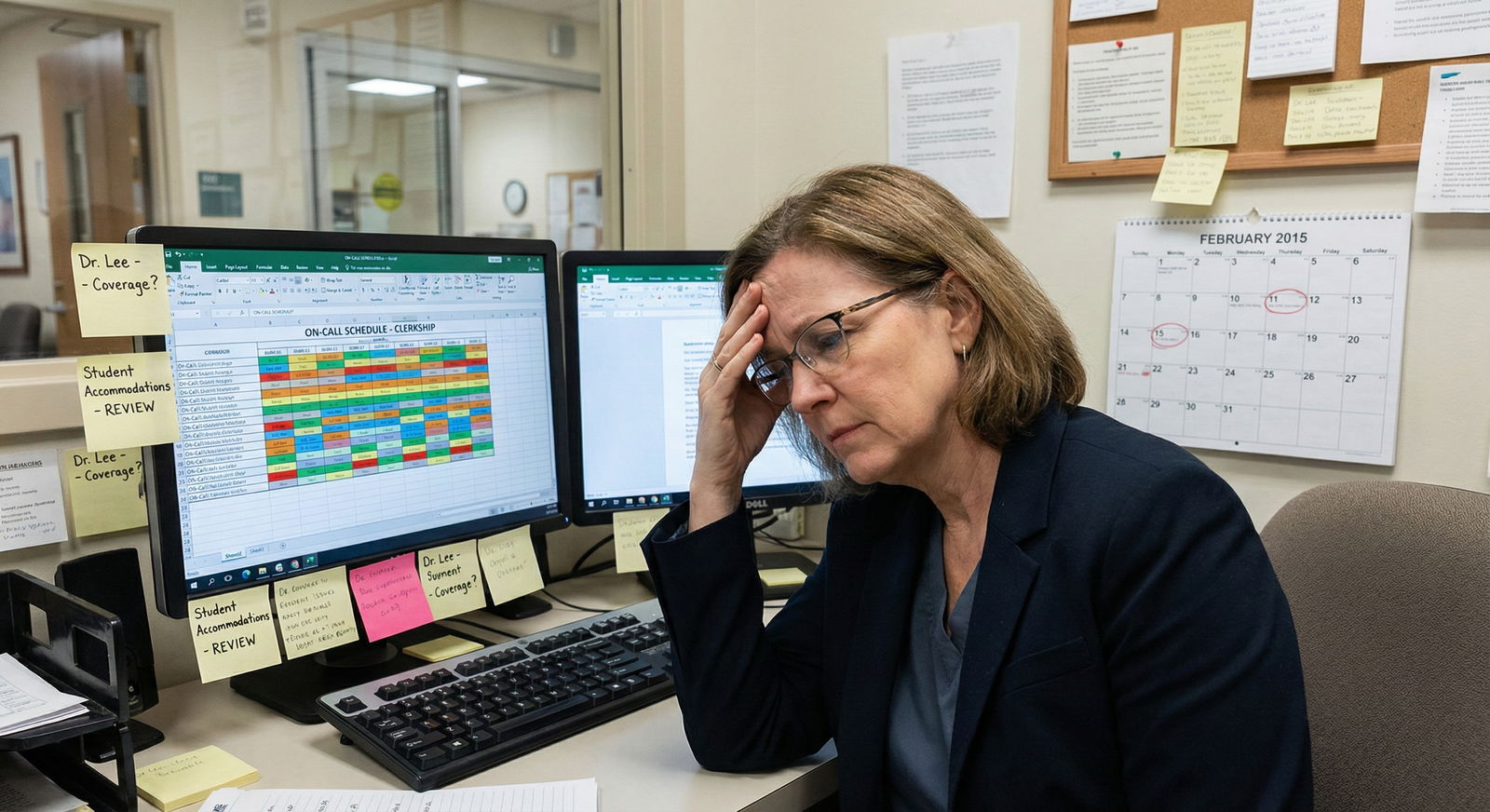
The standard culture around clinic work is broken for disabled clinicians and trainees. The unspoken rule is: “If it is on the template, you must do it yourself.” That rule is wrong. And unsafe.
If you cannot safely perform certain procedures, your job is not to “tough it out.” Your job is to re-engineer the work so patients are safe, you are safe, and your employment is sustainable. That requires negotiation. Systematic, structured, documented negotiation — not vague “I will just tell my preceptor.”
Let me walk you through exactly how to do that.
Step 1: Get Clinically Precise About What You Can and Cannot Safely Do
Hand-waving about “I have limitations” does not work. You need a clear, clinically framed skills profile.
Break it down like a pre-op risk assessment:
- List all expected clinic tasks and procedures
- History and physical exams
- EHR documentation and order entry
- Phone/telehealth visits
- Injections (IM, subcutaneous, joint)
- Phlebotomy
- Pap smears and pelvic exams
- IUD insertions/removals
- Endometrial biopsies
- Wound care and debridement
- Minor skin procedures (shave biopsy, punch biopsy, cryotherapy)
- Orthopedic injections
- Office spirometry, ECG setup, etc.
You know your setting. Add the exact procedures your clinic uses, not some generic list.
- Classify each item into 3 bins
- Safe Independently – You can perform these reliably under normal clinic conditions.
- Safe With Adaptations – You can perform these if specific changes are made (equipment, time, staffing).
- Unsafe / Cannot Perform – Doing these yourself risks harm to you or the patient.
Be brutally honest. This is not an identity question. It is a patient safety question.
- Write it down in clinical language
Example of bad wording:
- “I just have trouble with procedures.”
Better wording:
- “Due to limited grip strength and tremor in the right hand, I cannot reliably maintain needle stability for intra-articular injections or deep IM injections in the dorsogluteal site. These procedures are unsafe for me to perform independently.”
That difference matters. Administrators and risk management understand “unsafe to perform independently.” They do not respond well to “I get anxious when I do X” without a safety frame.
You should end up with a short document (1–2 pages) that clearly lists:
- Tasks safe as-is
- Tasks safe with specified adaptations
- Tasks that are unsafe and require reassignment or coverage
This becomes your backbone for accommodation discussions.
Step 2: Translate Limitations into Concrete Accommodation Options
Saying “I cannot do IUDs” is only half the work. You need a concrete alternative plan for how the clinic can still function.
For every unsafe or adapted task, propose at least one operational solution.
Common categories:
- Reassignment to another clinician
- Coverage by procedure-focused sessions
- Use of assistive devices
- Extended time / altered scheduling
- Alternative techniques
Example breakdown:
Joint injections
- Problem: Requires two-handed stability and force you do not have consistently.
- Options:
- All joint injections on your template are redirected to a designated “procedure clinic” session with another clinician.
- Or they are scheduled on days when a colleague with procedural interest is present and agrees to cover them.
Phlebotomy
- Problem: Fine motor demands and positioning incompatible with your physical limitations.
- Options:
- All labs drawn by nursing or phlebotomy staff (which many clinics already do).
- If clinic currently expects clinicians to do blood draws, negotiate a standardized policy shift to nurse-led phlebotomy “for all providers,” which quietly solves your problem.
Pelvic exams and Pap smears
- Problem: Positioning, dexterity, or endurance issues.
- Options:
- A chaperone or nurse positions equipment, adjusts stirrups, and handles specimen labeling.
- If you cannot do them at all, route those visits to another clinician while you absorb more complex diagnostic or chronic disease visits to maintain equity in workload.
The formula:
Limitation → Risk → Proposed adaptation → Net effect on clinic
You want to walk into negotiations with a menu of reasonable options, not just “I cannot do X.”
Step 3: Know the Legal and Policy Backbone Before You Ask
You are not begging for favors. You are requesting reasonable accommodations under disability law and institutional policy.
You need three pillars in your head:
Disability law principles (e.g., ADA or equivalent in your country)
- You are entitled to reasonable accommodations if you:
- Have a qualifying impairment that substantially limits major life activities, and
- Are otherwise qualified to perform the essential functions of the job/role with or without reasonable accommodation.
- Institutions are not required to remove essential job functions. But people over-label tasks as “essential” out of habit, not logic.
- You are entitled to reasonable accommodations if you:
“Essential function” vs “traditional expectation”
- Essential function ≠ “we always did it this way.”
- Ask: Could the clinic still safely care for patients if this procedure were reassigned?
- Yes? Then it is likely negotiable.
- No? Then you must focus on adaptation rather than removal.
- Example: For many internists, doing IUD insertions is not an essential function; it is optional advanced training.
Internal policies and disability services
- Hospital/clinic may have:
- A designated ADA/HR disability coordinator
- A faculty or trainee disability office
- A formal accommodation request process
- You want to use those formal channels. Verbal, undocumented agreements fall apart when leadership changes or a preceptor rotates out.
- Hospital/clinic may have:
Do a quick policy recon:
- Search your institution intranet for “disability accommodations,” “ADA,” or “reasonable accommodation.”
- Identify the person/office responsible.
- Note if they separate processes for:
- Employees
- Residents/fellows
- Students
Walk into any conversation knowing the rules better than the average manager. That alone changes the tone.
Step 4: Frame the Conversation Around Patient Safety and System Design
If you frame this as “I need special treatment,” you lose. If you frame it as “Here is how we guarantee safe, reliable care given my physical limitations,” people listen.
When you talk to:
- Program director
- Clinic medical director
- HR / Disability officer
- Preceptor
Use language like:
- “I want to make sure my practice is safe and consistent for patients over the long term.”
- “These specific procedures fall outside what I can perform safely, and I have structured alternatives to keep clinic flow smooth.”
- “Here is a concrete plan for redistribution and coverage that protects patient access and the clinic’s metrics.”
Bring your written skills profile from Step 1 and your adaptation menu from Step 2.
A sample script for opening the negotiation
“I have an established physical disability that limits certain procedural tasks. I have worked through a detailed list of what I can safely do, what I can do with adaptations, and what I cannot safely perform. My goal is straightforward: maintain high-quality patient care while practicing within safe physical limits.
Here is the breakdown, and here are several options for reassigning or adapting procedures that keep the clinic’s needs covered.”
This does three things:
- Signals that you are solutions-oriented.
- Frames the issue as safety and quality, not personal preference.
- Shows you have already done half of their job by creating a plan.
Step 5: Rebuild Your Clinic Template Instead of Reacting Visit-by-Visit
Constantly explaining your limitations at every single visit is exhausting and error-prone. Fix the template, not every individual encounter.
The goal: Patients scheduled with you generally do not arrive for procedures you cannot safely perform.
You can negotiate:
- Visit type filters
- Only certain visit types allowed on your schedule (e.g., “complex chronic care,” “new consult,” “routine follow-up”) while “procedure-only” visits go to a different template.
- Embedded notes in scheduling rules
- A clear but neutral rule in the scheduling system:
- “Procedures X, Y, Z are scheduled in the Procedure Clinic only.”
- Your name does not even have to appear.
- A clear but neutral rule in the scheduling system:
- Time-based segregation
- Example: You do no procedures on your regular clinic days, and procedures go to a shared “interventional half-day” staffed by colleagues who enjoy that work.
- Telehealth-heavy blocks
- If your disability makes physical procedures difficult but cognitive/diagnostic work is intact, construct more telehealth sessions where procedures are structurally impossible.
| Element | Standard Provider | You With Accommodations |
|---|---|---|
| Visit Types | All, including procedures | No procedure-only visit types |
| Procedure Slots | Mixed into schedule | Routed to separate procedure day |
| Telehealth Visits | 1–2 per half-day | 4–6 per half-day |
| Note in Scheduler | None | Rule: Procedures X/Y → proc pool |
The less ad hoc exception-handling you must do, the more sustainable this is.
Step 6: Build a Coverage Model That Feels Fair (So Colleagues Do Not Resent You)
Colleague resentment is real. “Why do I have to do all the joint injections?” is a question I have literally heard in team rooms.
You fix this head-on by:
Balancing the ledger
- If others cover your physical procedures, you take on equivalent work in other domains:
- More complex diagnostic cases
- More chronic disease management visits
- More administrative or quality work
- Leading teaching sessions for trainees
- Make the trade explicit with leadership:
- “I will not perform X procedures, but I can shoulder more of Y that many people dislike, such as high-complexity multi-morbidity visits or prior authorization battles.”
- If others cover your physical procedures, you take on equivalent work in other domains:
Formalizing coverage, not begging for favors
- A clear, written rule:
- “All IUDs are scheduled with Dr. A or B.”
- “All joint injections go to the Tuesday procedure session with Dr. C.”
- Not:
- “We will just find someone on the day of if needed.”
- A clear, written rule:
Communicating the arrangement once, not every week
- In a team meeting or email:
- “We adjusted templates so that Dr. X focuses on complex chronic disease and consults. Procedure-only visits are clustered in the shared procedure clinic for efficiency.”
- You do not need to disclose the disability details. The operational framing is enough.
- In a team meeting or email:

| Category | Value |
|---|---|
| Procedures | 40 |
| Complex Visits | 70 |
| Admin/QI | 50 |
The chart concept here: You give up some procedure volume, you increase your load of complex visits and system work. That makes the arrangement look like what it is: a redistribution, not a free pass.
Step 7: Document Everything. In Writing. Always.
Verbal promises vanish the moment someone is promoted, retires, or gets annoyed.
You need three layers of documentation:
Formal accommodation letter or agreement
- From:
- Disability services office, HR, or
- Program/clinic director in writing
- Should state:
- That you are entitled to and have been granted specific accommodations
- High-level description of how your duties are adjusted or supported
- From:
Operational implementation plan
- A short document or email that says:
- Which visit types you take
- Which procedures you do not perform
- Where those procedures are routed instead
- Any equipment or extra staffing you require
- Copied to:
- Clinic manager
- Scheduling supervisor
- Relevant colleagues who share coverage
- A short document or email that says:
Personal log
- Keep a simple record (even a private spreadsheet) of:
- Dates when accommodations fail (“scheduled for joint injection despite rule”)
- Any pushback or noncompliance from staff
- Patient safety concerns
- This gives you proof if you need to go back to HR or a disability office later and say, “The plan is not being followed.”
- Keep a simple record (even a private spreadsheet) of:
Do not assume goodwill is enough. People forget. Systems revert to default. Paper protects you.
Step 8: Handle Pushback Without Caving
You will encounter at least one of these responses:
- “But everyone is expected to do all the procedures.”
- “If you cannot do everything, maybe this is not the right specialty.”
- “We will try to make it work informally; no need to involve HR.”
- “Patients will be upset if they cannot get everything done with one clinician.”
Here is how to respond without starting a war.
Response to “Everyone is expected to do all the procedures”
“The legal standard is whether I can perform the essential functions of the role with reasonable accommodation. Many clinicians in this specialty do not perform the full procedural list. I am asking for a structured redistribution of specific procedures I cannot safely do, while taking on compensatory work that maintains clinic function.”
Translation: You are calling out the lazy use of “everyone.”
Response to “Maybe this is not the right specialty”
“I already meet the cognitive and clinical requirements for this specialty and perform the core diagnostic and management functions at a high level. The procedures in question are a small subset that can be reassigned without compromising patient care. Disability law is designed precisely to prevent forced exclusion when reasonable accommodations exist.”
Do not swallow veiled discrimination without naming the standard.
Response to “We will just keep it informal”
“Informal workarounds tend to break down over time and create risk for patients and for the institution. I want a stable, transparent arrangement that new staff and schedulers can follow without guesswork. That is why I prefer we go through the formal accommodation process and update the clinic’s scheduling rules.”
If they refuse, you escalate: disability office, ombudsperson, or HR.
Step 9: Adjust Across Training Phases and Career Stages
The mechanics differ if you are:
- A medical student in a clerkship
- A resident or fellow
- A practicing attending physician
But the framework is the same.
Medical students
Your leverage is lower, but safety and disability law still apply.
- Talk to:
- Your school’s disability office first.
- Then the clerkship director with a clear plan.
- Focus on:
- Core competencies (history, physical exam, reasoning) you can perform.
- Substituting nonessential procedures with:
- Observed participation
- Simulation lab practice
- Written/OSCE-based assessments instead of live procedures, if needed.
Residents and fellows
You are “in training” but also employees in many systems.
- Coordinate:
- GME office
- Disability/HR
- Program director
- You may need:
- Adjusted case logs. For example, you might not meet some procedural minimums but exceed others.
- A formal statement from your program about your modified training plan.

| Step | Description |
|---|---|
| Step 1 | Identify Limitation |
| Step 2 | Disability Office |
| Step 3 | Program Director |
| Step 4 | Define Essential Functions |
| Step 5 | Design Clinic Template and Coverage |
| Step 6 | Document Agreement |
| Step 7 | Monitor and Revise |
Attending physicians
You have more control, but also revenue and productivity pressures.
- You may negotiate:
- Different RVU targets (less procedural, more cognitive)
- Protected time for QI, teaching, or telehealth
- Custom clinic templates and team structures
If your employer refuses all reasonable accommodations and pushes you to do unsafe procedures, that is a red flag for legal consultation, not just another “polite discussion.”
Step 10: Revisit and Refine Over Time
Your condition might change. The clinic might grow. New procedures might appear.
Set a default expectation that this is iterative:
- Schedule a check-in every 6–12 months with:
- Your director
- Clinic manager
- Or disability services contact
- Review:
- What is working
- What keeps breaking (scheduling errors, staffing gaps)
- New demands (e.g., new procedure added to the clinic, new EHR).

| Category | Value |
|---|---|
| Year 1 | 3 |
| Year 3 | 2 |
| Year 5 | 2 |
| Year 8 | 1 |
| Year 10 | 1 |
You want fewer crises and more routine tune-ups as your career progresses.
Example: Putting It All Together
Let me give you a compact scenario that ties all this into something real.
Scenario:
You are a family medicine resident with a neuromuscular condition affecting grip strength, worse with repetition. You can:
- Do basic injections with adapted grips and extra time.
- Not reliably perform IUD insertions or joint injections.
- Otherwise excel in complex chronic disease care.
Your plan:
- Draft a one-page clinical abilities profile:
- List tasks safe, adapted, unsafe.
- Meet disability services:
- Get documentation and recognition of your rights to accommodations.
- Meet program director + clinic director with:
- Abilities profile
- Proposed changes:
- No IUD or joint injection slots on your template.
- All such procedures go to Friday procedure clinic run by faculty X and Y.
- You take additional complex chronic care visits and handle extra care coordination calls to balance workload.
- Update template:
- Remove procedure visit types from your schedule.
- Create clear routing rules in EMR for IUDs/joint injections.
- Document:
- Written agreement from GME and clinic director.
- Email to scheduler and clinic staff summarizing routing rules.
- Monitor:
- Keep a log of any mis-scheduled procedure visits.
- Bring data to quarterly meetings to adjust as needed.
Result: Patients get appropriate care. You practice safely. Colleagues see you pulling your weight, just in different ways.
Common Mistakes to Avoid
I have watched people stumble into three predictable traps.
Trying to “prove” you can do everything
- You hurt yourself. Or you have a near-miss with a patient. Or you burn out.
- Stop using procedures as an audition for worthiness. You already know your limits.
Accepting vague verbal assurances
- “We will try not to schedule you for those.”
- That is not a plan. That is wishful thinking.
- If it is not in the scheduling rules and not documented, it will fail.
Not offering any trade-offs
- If you only present “I cannot do X,” some colleagues will unconsciously see you as less useful.
- Present: “I cannot safely do X, but I can take on more Y and Z that are equally necessary.”

Quick Summary
Keep three things in focus:
You are not the problem. The workflow is.
Rebuild the clinic template, task distribution, and support so that your actual abilities match your assigned duties.Be concrete, documented, and unapologetic.
Specific task lists, specific adaptations, written agreements. No vague “we will see.”Trade, do not just subtract.
If you give up certain unsafe procedures, take on other cognitively demanding or system-critical work. That keeps you indispensable and respected.
You are allowed to be a competent clinician who does not do every procedure on the menu. Negotiate like that is normal—because it should be.
FAQ
1. Do I have to disclose my specific diagnosis to get accommodations for clinic duties?
No. You usually do not need to disclose your exact diagnosis to your program director or clinic leadership. Disability/HR offices may request medical documentation from your treating clinician, but that documentation can focus on functional limitations and restrictions rather than naming the condition in detail. With your direct supervisors, you can keep the conversation on what you can and cannot safely do, and what accommodations are needed, rather than diagnostic labels or private health details.
2. What if my director insists that every clinician “must” perform all procedures to be competent?
Push the conversation toward definitions of “essential functions” and actual practice patterns. Many physicians in the same specialty do not perform every potential procedure (for example, not all internists place IUDs, not all psychiatrists perform ECT). Ask directly which functions are truly essential and which are optional or redistributable. If your director still refuses to consider any accommodations, document the interaction and escalate to your institution’s disability office, HR, or GME leadership. At that point it is no longer a purely educational issue; it is a compliance and discrimination risk for the institution.



















