The biggest misconception about DO vs MD clinical training is this: people obsess over the letters and ignore the rotation ecosystem that actually shapes how they become physicians.
Let me break this down specifically: “community-heavy DO clinical models” and “academic MD tracks” are not vague vibes. They are very different structures with predictable strengths, gaps, and consequences for residency competitiveness, comfort level, and long‑term practice style.
If you are premed or early in med school and you are not thinking about where you will rotate (not just what school name is on the building), you are already behind.
1. The Two Dominant Models: What They Actually Look Like on the Ground
Forget the marketing language. Let’s define what people actually mean when they say “community-heavy DO model” vs “academic MD track.”
Community-heavy DO clinical model
This is what you see at many (not all) DO schools, especially newer, regional, or “mission-driven” ones.
Core features in real life:
- No single large university hospital owned by the school
- Clinical years (3rd and 4th) built from a network of:
- Community hospitals
- Private practice groups
- Federally Qualified Health Centers (FQHCs)
- Rural or suburban health systems
- Rotations often spread across multiple sites, sometimes across different towns or states
- Heavy use of preceptor-based teaching:
- You and one attending physician
- Maybe another student or occasional resident
- Limited or no in-house residency programs at the site
- Less standardized day-to-day structure
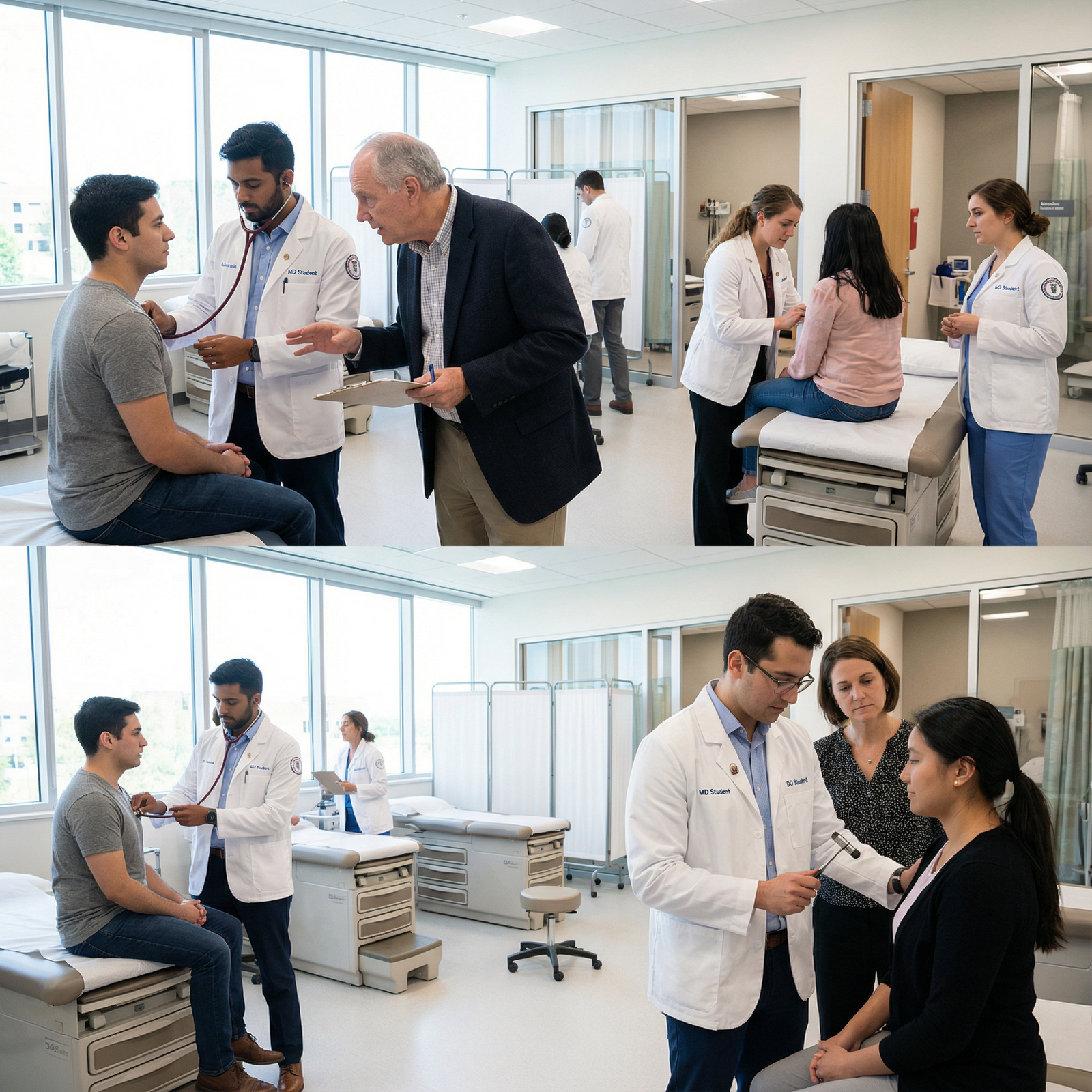
What it feels like as a student:
You walk into a community clinic at 8 a.m. It is you, your preceptor, 15–20 patients on the schedule, and a single MA. The attending throws you in: “You take room 3, full H&P, come present.” No big teaching team. No daily noon conference. But a lot of raw reps. You see the reality of outpatient medicine very fast.
Academic MD clinical track
Common at many established MD programs, especially those with their own university hospital system.
Core features:
- One or more large academic medical centers formally linked to the med school
- Numerous in-house residency and fellowship programs
- Majority of core rotations (IM, surgery, peds, OB/GYN, psych) run on:
- Teaching services
- With residents + attendings
- Embedded structured education (lectures, conferences, M&M, grand rounds)
- Specialty exposure built into the hospital ecosystem:
- Transplant
- NICU level III/IV
- Advanced oncologic surgery
- Interventional cardiology, etc.
- Evaluations often more standardized:
- Shared rubrics across clerkships
- Shelf exams tied to national norms
What it feels like:
You show up to medicine rounds with a team: attending, senior resident, interns, maybe a pharmacist and a couple of students. You pre-round, preround again for your senior, present on rounds, then spend the middle of the day fielding pages and getting pimped. There are conferences nearly every day. You see “complex” medicine, but you might not be the one doing the detailed visit for more than a handful of patients daily.
2. Clinical Exposure: Breadth vs Depth vs Complexity
Here is where people oversimplify. “Community rotations are low-yield” or “Academic hospitals are always better.” Both wrong.
You have three main dimensions of clinical exposure:
- Volume of direct patient encounters
- Complexity of pathology
- Structure and feedback around your learning
Community-heavy DO rotations: high volume, variable complexity
Strengths you actually feel:
You often get more hands-on volume.
- In a rural FM clinic, you might see 10–15 patients yourself in a day, present them, write notes, follow up plans.
- In small EDs, you may get to do more procedures because there is no parallel army of residents.
You see unfiltered real-world medicine.
- Chronic disease mismanagement
- Underserved populations
- Social determinants of health in your face (transportation, no insurance, no follow-up options)
You often develop independence earlier.
- No resident to hide behind.
- The attending may literally say, “What’s your plan?” and then either sign off or dismantle it.
Weaknesses:
- Case mix may skew toward “bread and butter”:
- Tons of hypertension, diabetes, URI, back pain
- Fewer transplant complications, rare autoimmune syndromes, or tertiary oncology cases
- Subspecialty exposure can be limited locally
- If there is no cardiothoracic service, you will not “absorb” that environment
- Teaching style is unpredictable
- Some community attendings love teaching: gold.
- Others see you as an extra task between patients.
Academic MD tracks: higher complexity, more structured teaching
Advantages:
You see more esoteric, complex pathology.
- Decompensated cirrhosis, LVAD management, complex congenital heart disease, chemo protocols.
- You learn to think in layers: primary disease, complications, iatrogenic harm, system issues.
Built-in academic culture.
- Daily or weekly noon conference
- Formal didactics, journal clubs, grand rounds
- Residents who can “translate” content down to student level
You get used to the flow of academic inpatient services.
- Pre-rounds, sign-out, multidisciplinary rounds
- EMR workflows at scale
- Paging culture, cross-coverage logic
Limitations:
- You can end up more observer than doer.
- Interns and residents write most of the orders and notes.
- Procedures (LPs, central lines) go to residents first.
- Outpatient exposure can be weak if clinics are run for resident efficiency, not student learning.
Bottom line: Community-heavy DO = intense ownership, hands-on reps, variable teaching, less ultra-rare pathology. Academic MD = structured teaching, high complexity, more layers between you and the patient.
3. Mentorship, Letters, and Networking: Quietly the Biggest Difference
This is where the model you choose can quietly help or quietly cap your ceiling.
Academic MD tracks: built-in pipeline
At a strong academic MD program, the network is half the value.
You get:
- Attending physicians who sit on national committees, guideline panels, fellowship selection committees.
- Residents who match into competitive specialties and can tell you precisely what programs look for.
- Department chairs who know each other by first name across institutions.
Letters of recommendation here are often:
- Written by people whose names are recognizable to program directors
- Explicit about your rank among students
- Backed by a context: “We take 30 students a year on this service; this one is top 10%.”
And you have repeat exposure to the same departments:
- Medicine rotation MS3
- Sub-I MS4
- Maybe a research month with the same group
You are not just a drifter passing through; you are part of a system.
Community-heavy DO rotations: relationship rich, prestige variable
In community DO models:
- Your preceptor might know every hospital leader in a 100-mile radius but not a single academic chair at a top-20 program.
- They may have zero research output. Or one paper from 1999 in a niche journal.
- They may be outstanding clinicians and mentors but their name means little on a national stage.
Letters here tend to emphasize:
- Work ethic
- Clinical responsibility
- Rapport with patients
- “I would trust this student with my own family.”
These are good letters. They carry weight for:
- Primary care programs
- Community-based residencies
- Regional hospitals that know your school’s history
They carry less automatic weight when:
- Applying to ultra-competitive specialties
- Aiming for big-name university residencies out of region
You can still get there as a DO student. It just takes more deliberate work:
- Away rotations at academic centers
- Step/Level exam performance at the top end
- Extra research effort, often remote or student-driven
4. Evaluation, Shelf Exams, and How You Are Graded
Clinical grades are messy everywhere, but the system you sit in changes the rules.
Academic MD environment
Typical pattern:
- Core clerkships tied to NBME shelf exams.
- Shelf exam = 20–40% of your grade (sometimes more).
- Clinical evaluations from multiple attendings and residents pooled into a composite score.
- Honors / High Pass / Pass tiers with institutional norms.
This model rewards:
- Test takers who can self-study well no matter how chaotic the rotation.
- Students visible to multiple evaluators (you cannot impress just one person and coast).
It punishes:
- Quiet but competent students who do not stand out in big teams.
- Students who struggle with standardized testing despite good clinical instincts.
Community-heavy DO arrangements
You see more variability:
- Some DO schools now use NBME or COMAT shelf exams for all core rotations.
- Others use school-written exams that may be less predictive of national board performance.
- Your clinical grade may hing more on:
- A single preceptor’s evaluation
- Local exams
- Case presentations or logs
Upside:
- A strong relationship with a good preceptor can translate directly into top clinical marks.
- Less test-centric anxiety on a day-to-day basis at sites that are exam-light.
Downside:
- Shelf-like rigor might not be consistent across all sites.
- If you get stuck with a disengaged preceptor, there is nowhere to hide. One bad evaluation can tank a grade.

| Category | Value |
|---|---|
| Shelf/Standardized Exam | 30 |
| Clinical Evaluations | 50 |
| Other (presentations, logs) | 20 |
The bar above represents a rough “average” mix in many systems. Community-heavy DO schools may push exam weight down, academic MD programs often push it up.
5. Specialty Choice and Match Competitiveness
Here is the part everyone cares about but dances around: Does the clinical model limit your options?
Short answer: The model does not decide your destiny. But it changes what you must do to reach certain endpoints.
If you want primary care, hospitalist work, or generalist specialties
Family medicine, internal medicine (categorical), pediatrics, psych, outpatient-focused OB/GYN in regional systems.
Community-heavy DO rotations can actually be an advantage:
- You see exactly the patients you will manage after residency.
- You learn to function with limited resources.
- Program directors in community and primary care programs like students who already live in that world.
Academic MD tracks still help, but the margin is smaller here. What matters more:
- Passing boards comfortably
- Solid letters from clinicians who actually worked with you
- Demonstrated interest in primary care (continuity clinic, community projects, etc.)
If you want highly competitive specialties
Think:
- Dermatology
- Plastic surgery
- Orthopedic surgery
- ENT
- Neurosurgery
- Radiation oncology
- Certain competitive fellowships down the line (GI, cards, heme/onc from a strong internal medicine base)
Academic MD tracks start you closer to the center of the playing field:
- You have in-house departments doing those specialties.
- You can get on projects, show up at conferences, attend specialty didactics.
- You can do home sub-internships where program leadership already knows your face.
As a DO in a community model, the climb is steeper:
You will likely need:
- Early and intentional specialty interest (by early MS2, not late MS3).
- External research collaborations (often at a nearby academic center or remote projects).
- Away rotations at target programs in MS4, where you show you can function in an academic environment.
- USMLE (in addition to COMLEX) with competitive scores if the specialty still heavily weighs it.
Is it possible? Yes. DO graduates match into those fields every year.
But you cannot coast through community rotations, decide late, and expect the system to carry you. It will not.
6. Lifestyle and Logistics: The Stuff Nobody Puts in Brochures
This is the unsexy but very real side.
Community-heavy DO models: geographic chaos is common
The pattern I have seen repeatedly:
- MS3 year:
- You live near Site A for internal medicine for 8 weeks.
- Then you move an hour away for surgery at Hospital B.
- Then another move for OB/GYN, maybe 2–3 hours away.
- MS4:
- You chase audition rotations, sometimes states away.
Costs:
- Rent in multiple locations or long commutes.
- Social isolation when you know no one locally.
- Increased burnout from constant re-orientation: new EMR, new staff, new policies.
Upside:
- You become adaptable. Fast.
- You learn to function in almost any system.
Academic MD tracks: consistency, but institutional pressure
Here:
- You usually stay near one central campus or city.
- Housing, commute, and social life are more stable.
- The main hospital’s EMR, workflows, and culture stay constant.
But:
- Academic centers can be pressure cookers.
- Everyone around you talks about research, fellowships, top residencies.
- Imposter syndrome can hit hard if you are not in the top 10–20% by test scores or evaluations.
Both systems burn people out. They just do it in different ways.
7. How to Decide: Matching Model to Your Reality
You are premed or early med school. You need a decision framework, not platitudes.
Ask yourself:
Do you strongly prefer a stable, centralized environment, or are you open to moving around?
- If the idea of relocating every 2–3 months makes you miserable, a heavily decentralized community model will wear you down.
Are you already leaning toward a highly competitive specialty?
- If yes, an academic MD environment (or a DO school with robust academic partnerships and strong match history in those fields) will make your life easier.
- If you go DO community-heavy, you will need a specific plan in year 1–2.
How self-directed are you academically?
- In community models, there may be fewer structured didactics. You are responsible for making sure your fund of knowledge keeps pace.
- In academic tracks, you still self-study, but the system gives you more formal teaching.
How much do you value “name recognition”?
- Big-name academic hospitals help open certain doors. That is just reality.
- Community training with excellent evaluations can still carry you far, especially within a region and in primary-care heavy fields.

| Step | Description |
|---|---|
| Step 1 | Start: Choosing Training Model |
| Step 2 | Prioritize Academic MD or DO with strong academic partners |
| Step 3 | Prefer centralized academic or hybrid model |
| Step 4 | Community-heavy DO or distributed track acceptable |
| Step 5 | Plan for research + away rotations |
| Step 6 | Plan for self-directed study + mobility |
| Step 7 | Competitive Specialty Interest? |
| Step 8 | Need Geographic Stability? |
8. Strategic Moves If You End Up in Each Model
You do not always get to choose. Sometimes the acceptance you have is the acceptance you take. Then the question becomes: How do you play the hand you were dealt?
If you are in a community-heavy DO model
You should:
- Aggressively track your rotation assignments early.
- Push for the highest-volume, most engaged preceptors. Your classmates will know who they are.
- Build a specific plan for standardized exams.
- Use UWorld / AMBOSS / NBME or COMAT-style resources systematically.
- Do not assume local exams reflect national standards.
- Identify at least one regional academic center.
- Try to do:
- An elective there
- Research with someone there
- A sub-I if you are targeting their programs
- Try to do:
- Over-communicate your goals to mentors.
- “I am considering cardiology; I know it is fellowship-level, but I want to match a strong IM program. What can I do now?”
If you are in an academic MD track
You should:
- Actually use the academic features.
- Attend conferences, even when not required.
- Meet faculty in your fields of interest before MS3.
- Do not disappear in big teams.
- Take ownership of your patients.
- Volunteer for presentations.
- Ask for feedback and act on it.
- Avoid the “prestige trap.”
- Matching into a solid, mid-tier program where you will be supported is better than chasing a name that will burn you out.
FAQ (Exactly 6 Questions)
Is a community-heavy DO clinical model automatically worse than an academic MD track?
No. It is different, not automatically worse. Community models excel at real-world, hands-on exposure and early independence. Academic tracks excel at structured teaching, complex pathology, and networking. For some goals (primary care, regional practice), a strong community DO environment can be ideal. For ultra-competitive specialties, the academic MD track starts you closer to the center of the action.Can a DO student from a community-heavy rotation system match into competitive specialties?
Yes, but it requires deliberate planning and above-average performance. You will likely need strong COMLEX and usually USMLE scores, targeted away rotations at academic centers, and research that shows you can function in an academic environment. You cannot rely solely on local community rotations to signal competitiveness for dermatology, neurosurgery, plastics, or similar specialties.Do academic MD tracks always provide better teaching than community DO rotations?
Not always. I have seen community preceptors who out-teach many academic attendings because they love education and are not stretched across research and admin duties. However, academic MD tracks offer more consistent institutional teaching (lectures, conferences, structured curricula). The variability is greater in community settings; you can have incredible or disappointingly minimal teaching depending on the site and preceptor.How much do letters of recommendation differ between these models?
In academic MD environments, letters often come from faculty with national reputations and can compare you directly to peer groups that program directors recognize. In community-heavy DO systems, letters may focus more on clinical performance, professionalism, and work ethic, but the writer’s name may carry less national weight. Strong content helps in both, but for competitive specialties at top-tier programs, who is writing the letter starts to matter more.Will rotating at a big-name academic hospital guarantee a better match?
No. It improves your exposure, networking, and potential letters, but you still need strong exam performance, solid clinical evaluations, and a coherent application story. I have seen students at big-name institutions underperform and match into mediocre fits, and DO students from community systems outwork everyone and land excellent positions. The environment offers opportunity; it does not replace performance.If I care about lifestyle and stability, which clinical model is usually easier?
In general, an academic MD track with a centralized hospital system is more stable. You are usually in one city, with one main EMR, one core set of policies. Community-heavy DO models frequently require moving between sites, new systems, and new teams every few months. Some people thrive on that variety; others find it exhausting. If constant relocation stresses you out, that should factor heavily into your decision.
Key takeaways:
- Community-heavy DO and academic MD clinical tracks shape how you learn, who mentors you, and what doors open easily versus what you must force open yourself.
- Neither model decides your ceiling, but each one changes the cost and strategy of reaching it—especially for competitive specialties.
- If you are smart, you will choose (or adapt to) a model with your actual goals, study style, and tolerance for instability in mind, not just the letters after your name.




















