The biggest mistake most DO students make is trying to look like watered‑down MDs instead of leaning hard into what actually makes them different: hands, movement, and function.
You want sports, pain, or MSK. Perfect. Osteopathic training, if you use it correctly, is not a handicap. It is a built‑in niche. But you have to build it intentionally, not by accident.
Below is a concrete, step‑by‑step plan for premeds and DO students who want to turn a DO background into a real advantage for:
- Sports medicine (primary care or ortho-related)
- Interventional or non‑interventional pain
- MSK‑heavy specialties (PM&R, physiatry, spine, occupational medicine, etc.)
No fluff. This is what actually moves the needle.
Step 1: Choose the Right Path Early (Premed and Early DO School)
If you are premed or in your first year, you still control the foundation. Do not waste it.
1. Be strategic about where you apply and matriculate
You want your DO degree to feed your niche, not fight it.
- Have strong OMM/OMT faculty who actually practice in sports, pain, or MSK
- Are attached to or affiliated with:
- Sports medicine fellowships
- PM&R departments
- Interventional pain clinics
- Are in regions with:
- Big athletic programs (D1 colleges, professional teams)
- High density of DO sports med / pain docs
Concrete moves:
- When researching schools, look for:
- “Sports medicine” or “PM&R” faculty profiles on the school website
- OMM clinic descriptions – do they mention athletes, concussions, spine, chronic pain, or performance?
- Email one or two faculty before you apply. Short, direct email:
- “I am a premed strongly interested in sports medicine and MSK. I am particularly drawn to how DO training can be leveraged in these areas. Could you share how students at [Your School] get exposure to sports or MSK care?”
If the reply is vague, generic “you’ll have lots of opportunities” language, that is a red flag.
2. Build a sports / MSK orientation as a premed
You do not need to be an ex‑NCAA athlete. You need a pattern of engagement with bodies and movement.
Aim for:
- At least one of:
- Athletic trainer aide or student assistant
- PT/OT aide
- Strength and conditioning coach assistant
- Personal trainer (with actual certification, not Instagram)
- Shadowing:
- At least 1 DO sports medicine physician
- At least 1 DO PM&R or pain physician
- Volunteer work:
- Community sports leagues
- High school athletics (sideline assistant, equipment support, injury screening events)
Why this matters:
- It makes your interest in sports/pain/MSK look real, not last‑minute
- It gives you the vocabulary and lived context to talk about biomechanics, performance, and function
Step 2: Use DO Training as a Tool, Not a Label
Most DO students treat OMM like a required class to survive. That is a waste if you want MSK‑heavy fields.
You are not “a DO.” You are someone with extra, clinically useful MSK skills that other students lack. Behave that way.
1. Commit to being outstanding at MSK/OMM
Do not aim for “passing.” Aim for “this is my thing.”
Concrete plan:
- During OMS‑1 and OMS‑2:
- Sit in the front row for OMM
- Stay after lab and ask the instructor to watch you do 1–2 techniques and critique
- Volunteer to be a model anytime they demonstrate spine, pelvis, or extremity techniques
- Practice regularly:
- Grab 2–3 classmates and run mini‑labs:
- Week 1: cervical exam + 3 HVLA techniques
- Week 2: shoulder exam + 3 soft tissue / muscle energy techniques
- Week 3: lumbar + sacrum evaluation and treatment
- Repeat, and tighten your speed, accuracy, and patient comfort
- Grab 2–3 classmates and run mini‑labs:
You want to be the person everyone asks, “Can you check my back / shoulder / neck real quick?”
2. Tie OMM to sports and pain from day one
Every time you learn a technique, ask: “Where does this show up in real sports or pain practice?”
Examples:
- Counterstrain for the piriformis → apply it to runners and powerlifters with glute or sciatic complaints
- Rib dysfunction techniques → apply them to swimmers, rowers, and overhead athletes
- Lumbar and sacral mechanics → relate to low back pain patterns in golfers, cyclists, and desk workers
Start to build mental templates:
- Mechanism of injury
- Common structural dysfunctions
- High‑yield OMM approaches
- Functional outcomes (ROM, pain, performance)
Your goal is to understand movement and mechanics at a level that feels native, not theoretical.
Step 3: Academic and Exam Strategy – You Still Need the Numbers
You cannot “OMT” your way past weak board scores in competitive fields. You have to clear the floor first.
1. For premeds: GPA and MCAT still matter
If you want options:
- Aim for:
- GPA: ≥ 3.5
- MCAT: ideally 508+ (higher is better, obviously)
This is not because DOs are inferior. It is because sports, PM&R, and pain fellowships want evidence you can handle complex patients and procedures. Numbers are a crude proxy.
2. For DO students: Treat COMLEX and USMLE strategically
Pain, PM&R, and sports medicine are increasingly comfortable with DOs, but program directors still like USMLE scores. You have a choice.
If you are serious about keeping as many doors open as possible:
- Strongly consider taking:
- COMLEX Level 1 + 2
- USMLE Step 2 (many now skip Step 1 but Step 2 is still valuable)
Your threshold:
- If you are scoring strong on COMSAEs and NBME practice and can realistically land:
- COMLEX Level 2: 600+
- USMLE Step 2: 240+
you are competitive at a wide range of programs.

| Category | Value |
|---|---|
| Primary Care Sports Med | 235 |
| PM&R | 240 |
| Pain (Anesthesia/PM&R) | 245 |
| Non-Interventional Pain | 230 |
Use this as a sanity check. You do not need a 260, but you also cannot be in free fall academically and expect your “DO niche” to save you.
Step 4: Build a Real Sports / MSK Portfolio During Medical School
This is where most people fail. They “have an interest” but no coherent record of doing anything about it. You will not make that mistake.
1. Create a focused extracurricular spine
I have seen this work repeatedly:
- Join or create:
- A sports medicine or PM&R student interest group
- Volunteer regularly:
- Sideline coverage with local schools or colleges
- Pre‑participation physical days
- Community running events, triathlons, CrossFit competitions
Do not just show up once a year. You want longitudinal involvement.
Then add:
- Leadership:
- Become VP or president of your sports/PM&R interest group
- Start an annual “MSK skills workshop” for other students, co‑run with OMM faculty
Now your CV says: “I did not just like sports. I built structures around it.”
2. Get meaningful sports/MSK‑relevant research
You do not have to publish in NEJM. You need real exposure to clinical questions.
Options:
- Work with:
- DO sports med physicians on concussion, overuse injuries, return‑to‑play protocols
- PM&R faculty on:
- Spasticity management
- Back pain outcomes
- MSK ultrasound
- Pain specialists on injection outcomes, opioid‑sparing protocols, or neuromodulation case series
High‑yield topics:
- OMT in low back pain vs standard care
- Headache and cervical OMT in athletes
- MSK ultrasound diagnosis and guided injection outcomes
- Functional status/return‑to‑play metrics
Your aim:
- At least 1–2 abstracts or posters
- If possible, 1 publication (case report, small retrospective series, or review)
The point is not the impact factor. It is that your narrative has data behind it: you think about these problems rigorously.
Step 5: Make Your DO Skills Visible in Clinical Rotations
Third and fourth year is where you separate yourself from generic “interested in MSK” applicants.
Your job is to become that student everyone remembers as “the DO who actually fixed people’s pain and knew MSK cold.”
1. On family medicine / internal medicine
Do not just be another student doing med recs.
For every clinic day:
- Quietly track patients coming in with:
- Low back pain
- Neck pain
- Shoulder, knee, or hip complaints
- Tension headaches
Then:
- After the normal exam, ask your attending:
- “Would you be open to me doing a quick targeted MSK/OMT evaluation on this patient to see if we can offer some immediate relief?”
If they say yes (most will at least once out of curiosity):
- Perform:
- Focused structural exam
- 1–3 simple, safe techniques:
- Soft tissue, muscle energy, basic articulation
- Document:
- Findings
- Patient’s response (subjective + objective)
Over time:
- You become the person attendings start asking:
- “Can you look at this patient’s neck?”
- “Try some OMT on this guy’s low back and see if it helps.”
Now you are no longer generic. You are high‑value on the team.
2. On PM&R, sports, and ortho electives
This is your proving ground. Your goal on these rotations:
- Be excellent at:
- Gait analysis
- Joint exams (shoulder, knee, hip, spine)
- Basic neuro/MSK localization
- Show:
- You understand biomechanics
- You can integrate OMT into broader treatment, not as a magic trick
Concrete actions:
- Before your elective, review:
- Bates’ MSK exam
- Specialty‑specific resources (e.g., “Netter’s Orthopaedic Clinical Examination,” Braddom’s for PM&R, etc.)
- Ask on day one:
- “I have strong training in OMT and MSK exam. Where do you see that fitting into what this service does, if at all?”
Then adapt to the attending’s comfort:
- If they are DO and pro‑OMT:
- Offer to do quick OMT before or after injections, or on tricky chronic pain follow‑ups
- If they are non‑DO and skeptical:
- Focus primarily on exam skills, functional assessment, and treatment planning
- Use OMT judiciously, and only after building trust
You want them to leave with: “That student was technically sharp, thoughtful, and added value using their DO training appropriately.”

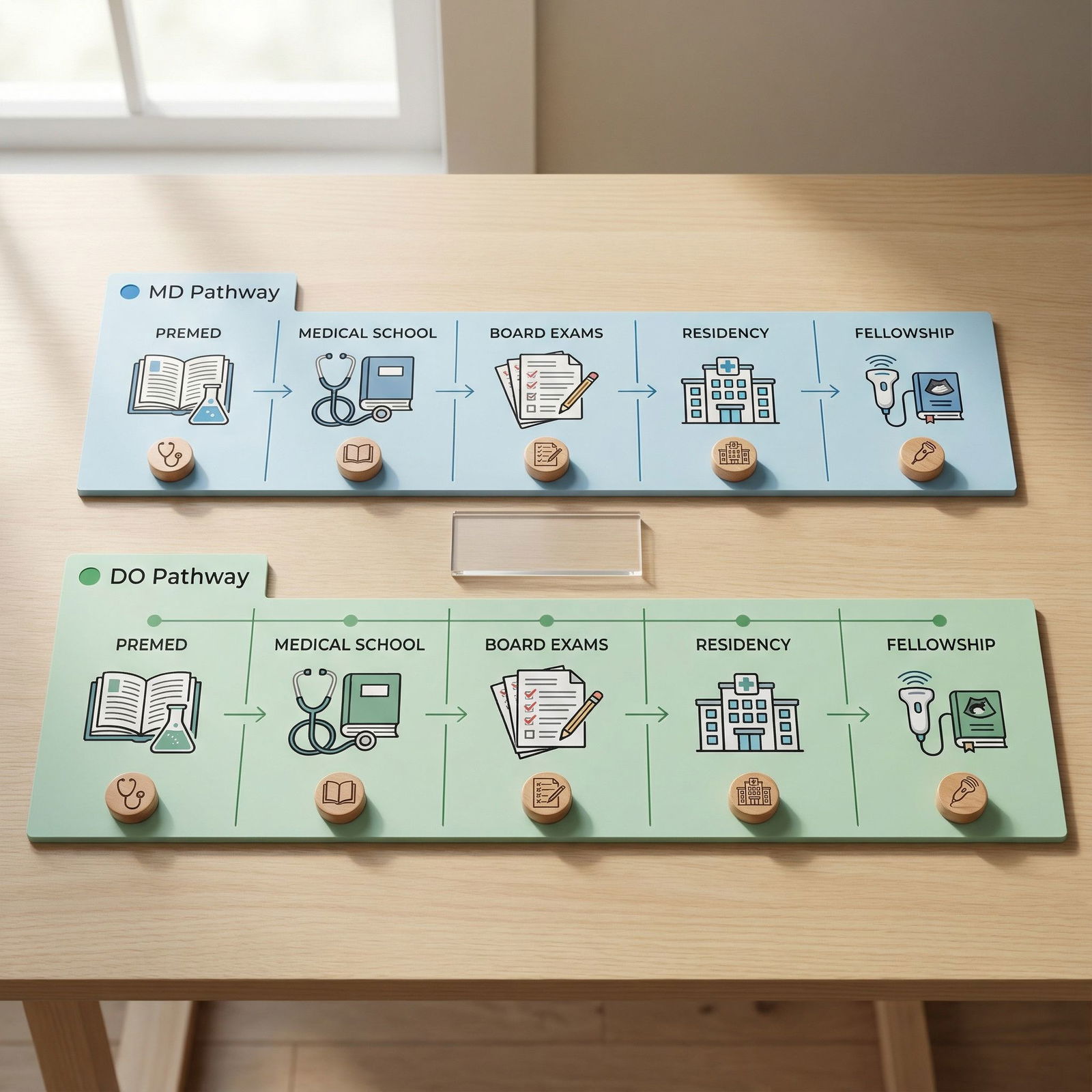
| Step | Description |
|---|---|
| Step 1 | Premed with Sports/MSK Interest |
| Step 2 | Matriculate at MSK-Friendly DO School |
| Step 3 | Excel in OMM and MSK Early |
| Step 4 | Targeted Sports/PMR Research & Activities |
| Step 5 | High-Impact Clinical Rotations |
| Step 6 | Strong MSK-Focused Residency Application |
Step 6: Choose Residencies That Actually Value DOs and MSK Skills
You can have the perfect story and still sabotage yourself by applying to the wrong programs.
Your goal is not “any program.” Your goal is the right ecosystem.
1. Pick the right core specialty pipeline
For sports, pain, and MSK, the common routes:
- Primary Care Sports Medicine:
- Family Medicine → Sports Med fellowship
- Internal Medicine or Pediatrics → Sports Med fellowship (less common but possible)
- PM&R:
- PM&R residency → Sports Med or Pain fellowship (or general MSK/spine practice)
- Pain Medicine:
- Anesthesia → Pain fellowship
- PM&R → Pain fellowship
- Neurology → Pain fellowship
- Non‑interventional pain / MSK:
- PM&R
- Occupational medicine
- Some family medicine programs with strong MSK/OMT emphasis
For DOs who want to maximize their niche:
- PM&R and Family Medicine (with sports) are very DO‑friendly and extremely logical fits
- Anesthesia pain is more competitive but still very attainable for strong DO candidates from solid programs
2. Target programs with a track record of DO success
Do not guess. Look at actual resident lists and fellow profiles.
Checklist:
- Go to program websites:
- Look at current residents
- Count how many DOs, especially in senior classes
- Scan faculty:
- How many DO attendings, especially in sports, spine, or pain roles?
- Look at their fellowship placements:
- Do they place residents into sports and pain with some regularity?
If a program has:
- Zero DOs in the last 5 years
- No DO faculty You are not “breaking barriers.” You are volunteering to be their experiment. That is a bad bet.

| Category | Value |
|---|---|
| Community Family Med with Sports Focus | 70 |
| University-Affiliated PM&R | 50 |
| University Anesthesia | 20 |
| Elite Academic PM&R | 35 |
You want to live as far left on that chart as your numbers and goals reasonably allow.
Step 7: Sell Your DO Background the Right Way in Applications
You are not apologizing for being a DO. You are positioning it as a deliberate asset.
1. Personal statement: make the DO angle explicit but not cheesy
Bad version:
- “As a DO, I believe in holistic care.”
No one cares. Everyone says that.
Better structure:
- Brief clinical story:
- A patient with chronic shoulder pain who had seen multiple providers, improved only when you combined:
- Detailed MSK exam
- Functional rehab plan
- OMT for scapular mechanics
- A patient with chronic shoulder pain who had seen multiple providers, improved only when you combined:
- What you did:
- How your DO training let you see the structural problem differently
- How that shaped your career goal:
- To work at the intersection of sports performance, pain control, and function
- What you want from residency:
- A program where you can:
- Refine advanced MSK exam
- Integrate procedures (injections, ultrasound, etc.)
- Use manual skills within evidence‑based care
- A program where you can:
Focus on outcomes and skills, not slogans about “mind, body, spirit.”
2. Letters of recommendation that actually mention your DO niche
Tell your letter writers what to emphasize:
- Your MSK exam skills:
- “One of the best physical exam students I have trained in the last five years.”
- Your OMT integration:
- “Frequently used OMT appropriately to relieve pain and improve function in clinic.”
- Your consistency:
- “Took the initiative to develop and lead MSK workshops for junior students.”
Give them a one‑page summary of:
- 3–4 patient stories that show your MSK/OMT value
- Research or projects you did with them
- Your target fields (sports, PM&R, pain)
Do not assume they remember everything. Make it easy for them to write the right letter.
Step 8: Develop Procedural and Ultrasound Skills Early
Sports, pain, and MSK are not just about hands. They are also about needles and imaging.
You can start building that profile even as a student.
1. Musculoskeletal ultrasound as a differentiator
Ultrasound is huge in:
- Sports medicine
- PM&R
- Pain clinics
- Interventional spine practices
Concrete steps:
- Attend:
- Any free or low‑cost MSK ultrasound workshops offered by:
- Your school
- Local PM&R departments
- National meetings (AAPM&R, AMSSM student tracks, etc.)
- Any free or low‑cost MSK ultrasound workshops offered by:
- Practice:
- Shoulder landmarks
- Knee joint spaces
- Achilles and plantar fascia
- Basic nerve and tendon tracking
You do not need to be an expert. You just need to walk into residency having:
- Held a probe
- Understood basic sono‑anatomy
- Demonstrated interest in image‑guided procedures
2. Basic procedure exposure
On rotations:
- Ask to observe and assist with:
- Joint injections
- Trigger point injections
- Nerve blocks (if in pain/anesthesia rotations)
- Always connect your OMT and MSK exam findings to:
- Needle target choice
- Rehab recommendations
- Follow‑up evaluation
You are training your brain to think procedurally, not just structurally.

Step 9: Use Conferences and Networking as Force Multipliers
If you stay hidden at your home institution, your DO niche has limited reach. You need to be visible where decisions are made.
1. Attend targeted meetings
High‑yield conferences for DO students interested in MSK fields:
- AMSSM (American Medical Society for Sports Medicine)
- AAPM&R (physiatry)
- NASS (North American Spine Society) – more advanced but very MSK/pain heavy
- AAPM or ASRA for pain (especially as a senior student or resident)
- AOA or specialty‑specific DO meetings with sports/pain/OMT tracks
Your priorities at these:
- Present something (poster > nothing)
- Introduce yourself to:
- Fellowship directors
- Program directors from places you might apply
- DO faculty in your target niche
Have a 20‑second story ready:
- Who you are
- That you are a DO
- Your interest in sports/pain/MSK
- How you are using your OMT and MSK training actively in clinic and research
2. Follow up like an adult
After the conference:
- Send a short email:
- “Thank you for taking a moment to talk to me at AMSSM. I appreciated your perspective on [X]. I am a DO student with a strong focus on sports and MSK, and I hope to rotate or apply to your program in the coming year.”
Save these contacts. This is how people remember you later when your application crosses their desk.

| Step | Description |
|---|---|
| Step 1 | Attend MSK/Sports/Pain Conference |
| Step 2 | Present Poster or Abstract |
| Step 3 | Meet Faculty & Program Directors |
| Step 4 | Follow-Up Emails |
| Step 5 | Sub-I or Away Rotation Opportunities |
| Step 6 | Stronger Residency/Fellowship Application |
Step 10: Avoid the Common DO Traps in Sports, Pain, and MSK
Let me be blunt. These are the ways DO students sabotage themselves.
Treating OMT as a separate religion instead of a clinical tool
- You want your attendings to see:
- Good MSK exam
- Good clinical reasoning
- OMT as one piece of a broader plan
- Not: “This student wants to do magic hands on everyone.”
- You want your attendings to see:
Using “holistic” as a replacement for real expertise
- Every applicant claims to be holistic.
- You stand out by:
- Knowing which maneuvers stress the supraspinatus vs the labrum
- Adjusting rehab plans to the actual sport demands
- Understanding opioid risk stratification and multimodal pain control
Ignoring basic competitiveness
- You cannot:
- Score in the bottom quartile
- Have weak letters
- No research, no leadership
and expect “I do OMT” to save you. It will not.
- You cannot:
Choosing residencies that do not understand or value DO training
- If the leadership is openly dismissive of OMT or DOs, do not martyr yourself.
- Go where your skill set is considered an asset, not a curiosity.
Failing to build a coherent story
- Your application should read like:
- “Since premed, this person has been pulled toward sports/pain/MSK”
- “They used their DO training to deepen that focus.”
- Not:
- “They suddenly discovered sports medicine 6 months before ERAS opened.”
- Your application should read like:
The Bottom Line: How to Actually Turn DO into a MSK Niche
If you remember nothing else:
Make MSK your craft, not a talking point.
Become objectively excellent at MSK exam, biomechanics, and basic OMT. Build that reputation among classmates and attendings.Align every stage of your training with sports/pain/MSK.
From premed activities to research, rotations, conferences, and residency choice, build a visible, coherent record that you live in this space.Sell your DO background as a concrete advantage, not a slogan.
Show, case by case, how your manual skills and structural thinking improved real patients’ pain and function. Numbers get you in the door; your DO‑shaped MSK skill set is what makes you memorable.
Do this right and you are not “the DO applicant trying to keep up.”
You are the MSK person programs fight to recruit.




















