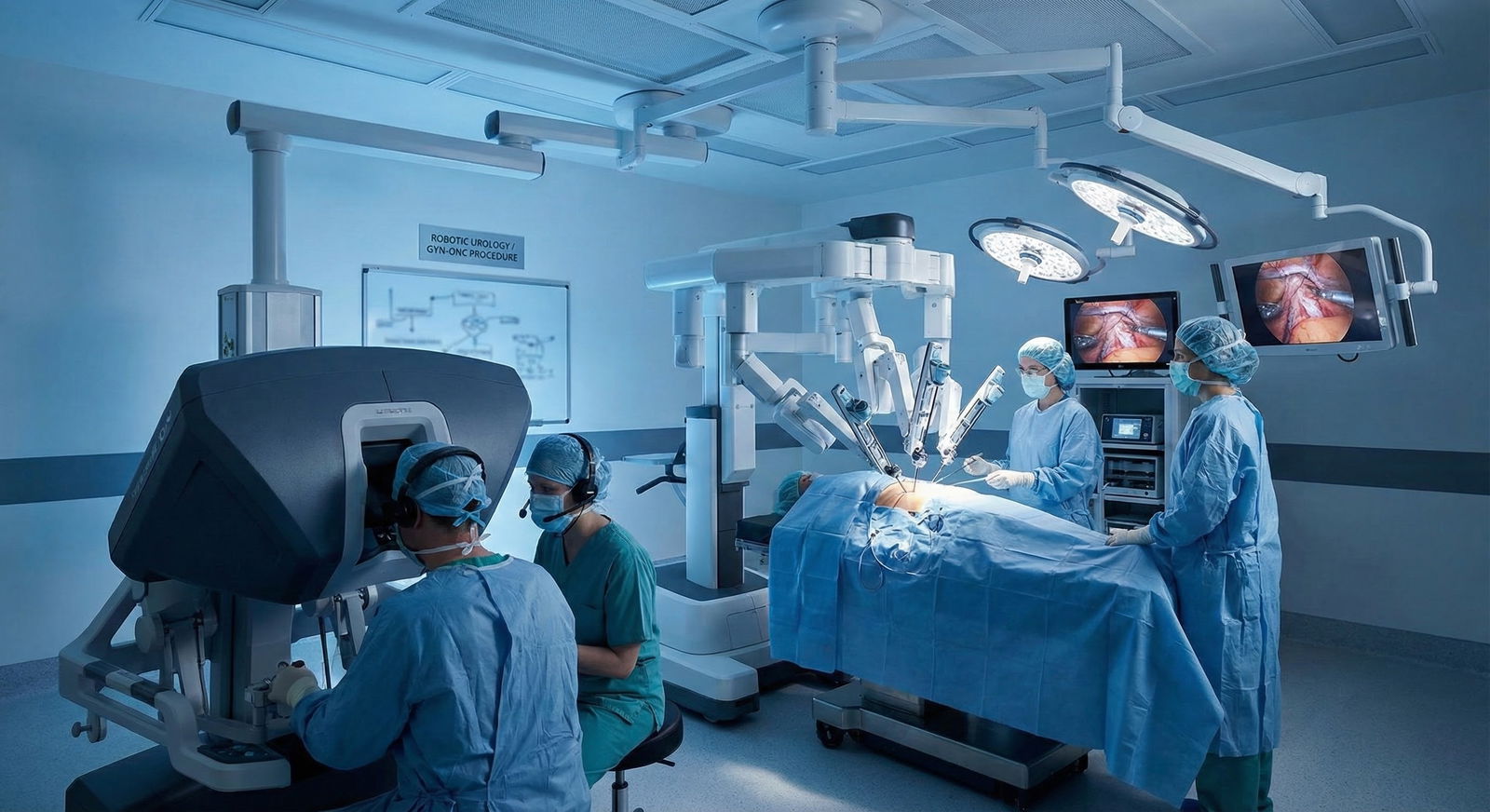
You are scrubbed in on a Friday afternoon in a single-robot hospital. The urologist wants to start a robotic prostatectomy at 1:00 p.m. The gyn-onc team is insisting they have the robot booked for a staging hysterectomy with pelvic and para-aortic lymphadenectomy. Same pelvis. Same robot. Completely different mentality about how to use it.
You stand there watching the room turnover and you realize: urology and gyn-onc are operating in the same anatomic sandbox, but they treat the robot like two different instruments. Port placement, patient positioning, who controls the ureter, how much lymph node you “must” take – none of it is standardized across the specialties. And it has consequences: oncologic adequacy, functional outcomes, complications, OR time, cost.
Let me break down where these worlds overlap, where they diverge, and where the future is going.
1. The Shared Playground: What Urology and Gyn-Onc Actually Have in Common
Both specialties use robotic systems (mostly da Vinci platforms right now) for deep pelvic work that would be miserable via open or conventional laparoscopy.
Common denominators:
- Target territory: Confined pelvis, retroperitoneum, pelvic sidewall, obturator fossa, presacral space, para-aortic region.
- Ergonomic need: Narrow working space, sharp angles, and awkward wrist positions that are painful with straight laparoscopic sticks.
- Goals: Maximal oncologic control with minimal blood loss and preservation of function—continence and erections in prostatectomy; bladder, sexual, and bowel function in radical hysterectomy and debulking.
But from the very first move—patient positioning—urology and gyn-onc start diverging.
2. Positioning and Access: Same Pelvis, Different Priorities
Urology: Optimized for Prostate and Bladder Neck Work
Robotic prostatectomy and cystectomy are posture-driven procedures. The prostate is buried behind the pubic symphysis and anterior to the rectum. Access is half the battle.
Typical pattern:
- Position: Steep Trendelenburg (30–40°), legs in low lithotomy, arms tucked.
- Rationale: Gravity clears bowel out of the pelvis. Steep angle makes the deep, narrow male pelvis accessible.
- Risks: Facial and airway edema, raised intraocular pressure, peripheral nerve injuries, compartment issues if you are not careful and the case runs long.
Port strategy is usually:
- A supra- or infra-umbilical camera port.
- Two robotic working ports at or just above the level of the umbilicus, spread wide enough to avoid arm collision when you are working deep.
- An assistant port on the right, between camera and right robotic arm, for suction, clip appliers, and specimen bags.
- Sometimes a fourth robotic arm for retraction of the bladder or seminal vesicles.
Everything is calibrated around perfect angles to the prostate and bladder neck, with less concern initially about extensive upper-abdominal access.
Gyn-Onc: A Wider Field – From Cul-de-Sac to Diaphragm
Gyn-onc is not just “pelvis.” It is pelvis plus para-aortic nodes, omentum, diaphragm, liver surface, and bowel when needed. So the robot setup is built for range.
Common approach:
- Position: Moderate Trendelenburg (20–30°) more often than the extremes urology uses. Lithotomy is standard, but more flexibility in leg height because the primary target is the uterus/ovaries, which are more mobile than a prostate encased in bone.
- Rationale: Enough tilt to clear the bowel, but not so extreme that a 6-hour staging plus debulking causes massive edema.
Port strategies differ:
- Camera port is often supra-umbilical, sometimes even higher for morbidly obese patients so the camera can see pelvis and upper abdomen.
- Robotic arms triangulated laterally, higher and wider than urology would place them, to allow:
- Wide lymphadenectomy along the aorta.
- Omentectomy.
- Pelvic work without re-docking.
Or, if the main work is deep pelvic—say a radical hysterectomy—ports may migrate lower and closer, resembling prostatectomy layouts, but still with more lateral distance to access sidewalls and nodes.
Gyn-onc’s guiding principle: configuration must serve both staging (nodes, omentum) and resection (uterus, adnexa, parametria) without having to reorganize mid-case.

| Category | Value |
|---|---|
| Robotic Prostatectomy | 35 |
| Robotic Cystectomy | 30 |
| Radical Hysterectomy | 25 |
| Ovarian Cancer Staging | 20 |
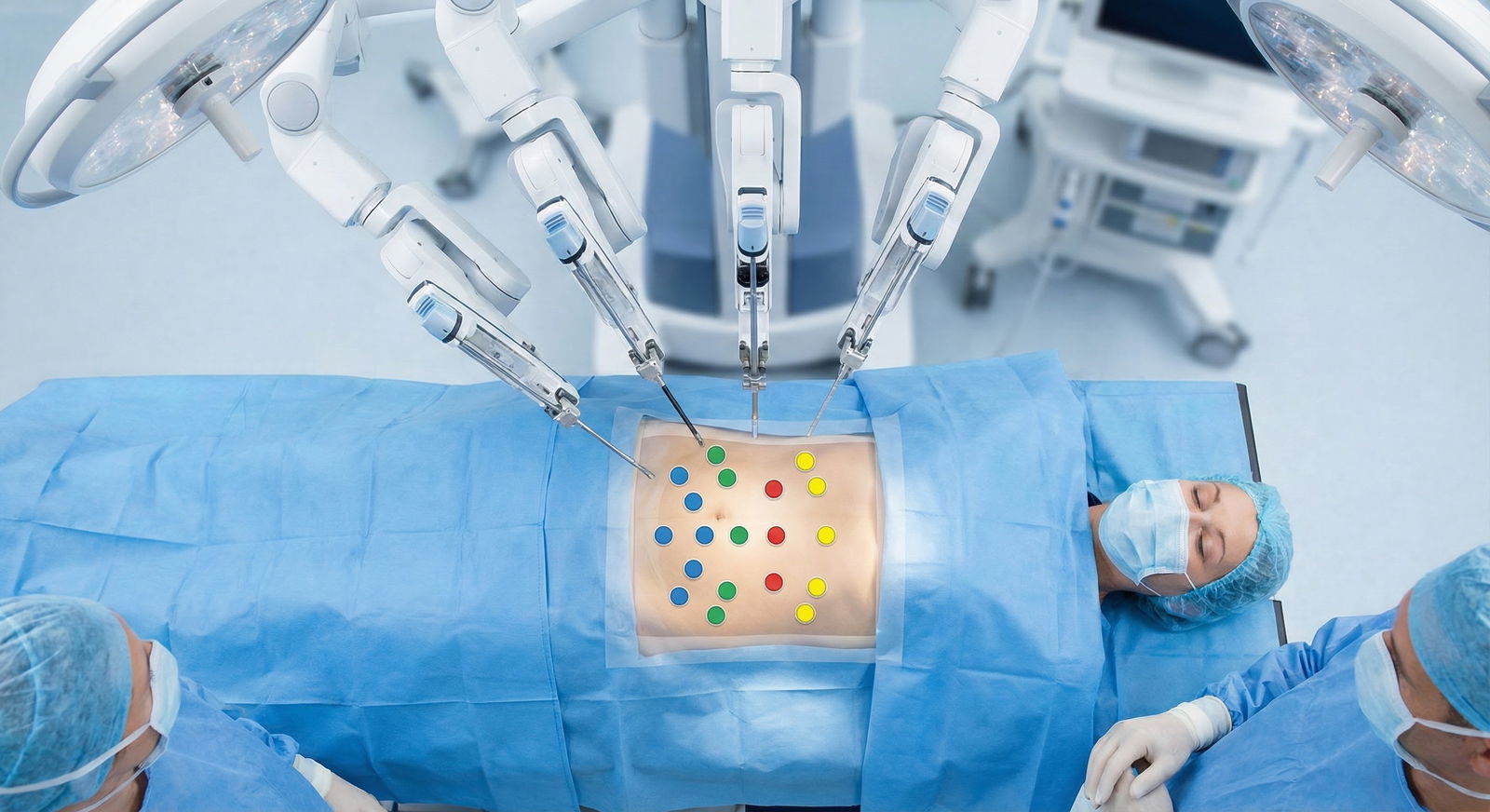
3. Port Placement: Millimeters Matter, and the Two Fields Think Differently
If you have ever tried to run a gyn-onc operation out of a prostatectomy port map, you already know it: it feels wrong.
Urology Port Nuances
For robotic prostatectomy (da Vinci Xi as example):
- Camera: 2–3 cm above the umbilicus, midline.
- Right/left robotic arms: 8–10 cm lateral to camera, slightly caudal, to allow downward approach into the pelvis.
- Third arm: often on the patient’s left, more cranial, used to retract bladder or Denonvilliers’ fascia.
- Assistant port: on the right, between camera and right robotic arm.
Priorities:
- Direct, unobstructed line to:
- Bladder neck.
- Prostatic apex.
- Dorsal venous complex.
- Minimized external arm collision while working deep with crossed instrument paths.
- Ability to swing from anterior (retzius space) to posterior (Denonvilliers plane) perspectives without re-docking.
The mental model: “Everything orbits the prostate.” You optimize ergonomics for one fixed target.
Gyn-Onc Port Nuances
For a total hysterectomy with pelvic and para-aortic lymphadenectomy:
- Camera: Usually midline, often 3–5 cm above the umbilicus, higher if BMI is elevated.
- Robotic arms:
- Ports fanned out across the upper abdomen, often at or above the level of the umbilicus, so you can reach para-aortic nodes around the IMA and above.
- Generous lateral spacing to clear the rib cage and allow reach to the diaphragm or splenic flexure if needed.
- Assistant port: Often low and lateral, for suction, staplers, introduction of specimen bags, and suture passing.
The mental model in gyn-onc: “I may need to go anywhere from cul-de-sac to diaphragm.” Ports are set for global reach, not just a single, deep fixed target.
You see the difference in how much re-docking each field tolerates. Urology hates re-docking. Gyn-onc will accept some repositioning if it means they can clear nodes from pelvis to renal veins.
4. Dissection Strategy: Oncologic Plan vs Functional Plan
Both groups care about cancer control and function. They weight the trade-offs differently.
Urology: Nerve-Sparing and Function Front and Center
Robotic prostatectomy is obsession-level focused on:
- Erectile function.
- Urinary continence.
The robot is used to peel tissue away from critical structures under magnification and with articulating wrists.
Distinct moves:
- Intra-fascial or inter-fascial nerve-sparing:
- Working right on the prostate capsule (intra-fascial) or just outside it (inter-fascial).
- Using the robotic wrist to roll the prostatic fascia while preserving neurovascular bundles hugging the prostate at about 5 and 7 o’clock positions.
- Dorsal venous complex control:
- Some surgeons stitch it first with a figure-of-eight suture before division.
- Others carefully divide with bipolar and then oversew, taking advantage of magnified robotic view to prevent major bleeding.
- Bladder neck preservation:
- Careful dissection to preserve as much circular bladder neck muscle as possible, improving early continence.
The urethrovesical anastomosis is micromanaged with wristed instruments: symmetric bites, no tension, often a running two-suture technique starting posteriorly (Rocco stitch or equivalent) to re-approximate posterior musculofascial plate.
Oncologic priorities are non-negotiable, but urologists are constantly pushing for maximal nerve-sparing unless margin risk is too high. The robot is their tool to “cut closer” safely.
Gyn-Onc: Parametrium, Nodes, and Margins Rule the Day
Gyn-onc uses the robot to safely expand the boundaries of radical surgery—especially when reaching into tight corners like the paravesical/pararectal spaces, obturator fossae, and upper para-aortic region.
Distinct moves:
- Parametrial clearance in radical hysterectomy:
- Skeletonizing the uterine artery at its origin from the internal iliac.
- Dissecting the ureter from the medial leaf of the broad ligament (the famous “ureteric tunnel”) sharply with excellent robotic visualization.
- Taking uterosacral and cardinal ligaments progressively further laterally, depending on the radicality class (e.g., type C resection).
Here the balance tilts toward lateral clearance and margin, sometimes at the expense of radical nerve-sparing. There is more discussion now about uterine nerve-sparing techniques, but it is not as entrenched nor as parametrically codified as prostate nerve-sparing.
- Nodal dissection:
- Pelvic nodes: Over external and internal iliac vessels and in the obturator fossa, exposing obturator nerve and preserving it while clearing fatty nodal tissue.
- Para-aortic nodes: Rolling peritoneum off the aorta and IVC, exposing renal veins, sparing the ureters and autonomic chain while stripping nodal tissue.
This is where the robot shines for gyn-onc: high-precision lymphadenectomy in tight vascular corridors. It is not about a 3 mm difference in nerve traction; it is about full, safe exposure of aorta, IVC, lumbar veins, and sympathetic chain under magnification.
Bowel, bladder, and sexual function are relevant, but the driving question is: “Have we done an adequate staging and resection with safe vascular control?”
5. Ureter Handling: Co-Owned Real Estate, Different Cultures
The ureter is where urology and gyn-onc collide conceptually.
Urology’s Relationship with the Ureter
In robotic prostatectomy:
- The ureter is background. It is not usually manipulated.
- In cystectomy, ureter handling is focused on:
- Ensuring negative ureteral margins.
- Preparing for urinary diversion (ileal conduit, neobladder) with:
- Adequate length.
- Preserved blood supply.
- Ureteroneocystostomy or ureteroenteric anastomosis is usually done with standard 4-0 or 5-0 sutures under robotic magnification.
Urologists are comfortable dissecting ureters free, trimming them, reimplanting them, or even reconfiguring them. They think of the ureter as something they can cut and reconstruct.
Gyn-Onc’s Relationship with the Ureter
In gyn-onc operations:
- The ureter is a structure to be unroofed, mobilized, and protected—especially where it runs under the uterine artery (“water under the bridge”).
- Routine maneuvers:
- Opening the peritoneum lateral to the infundibulopelvic (IP) ligament.
- Identifying the ureter along the medial leaf of the broad ligament.
- Dissecting it free of parametrial tissues to allow a wide radical resection.
Gyn-onc surgeons are exquisitely aware of where the ureter lives in relation to uterine vessels and parametria, but many are less eager to cut and reimplant it unless oncologically required. The ureter is something to be peeled away from tumor, not re-plumbed.
This difference affects technique:
- Urology spends more time on distal ureter and bladder or conduit tension-free anastomosis.
- Gyn-onc spends more time in the ureteric tunnel, intimately freeing ureter from dense parametrial tissue, often in radiated or inflamed fields.
The robot’s fine wrist articulation is invaluable to both, but in very different choreography.
6. Reconstruction: Anastomoses, Vaults, and Diversions
Once the specimen is out, the reconstruction phase exposes another philosophical split.
Urology: Anastomosis as the Make-or-Break Step
Robotic platforms were basically made for the urethrovesical anastomosis.
Robotic prostatectomy:
- Typical approach: two running 3-0 monofilament sutures (e.g., barbed or non-barbed), starting at 6 o’clock posteriorly, meeting at 12 o’clock anterior.
- Goals: watertight seal, mucosa-to-mucosa apposition, minimal tension.
- Fine wrist movements and 3D depth perception are crucial.
Bladder reconstruction/diversion:
- Neobladder or ileal conduit: bowel suturing, ureteroenteric anastomoses.
- Many centers now do fully intracorporeal urinary diversions, where the robot handles all suturing: ileal segment isolation, bowel anastomosis, and ureteral implantation.
Every millimeter of tension, angulation, or mucosal inversion matters. The robot gives the granularity to fix that.
Gyn-Onc: Vault, Bowel, and Support
In gyn-onc:
Vaginal cuff closure:
- Robotic closure with barbed sutures, often 0 or 2-0 monofilament, full-thickness bites.
- Attention to cuff angle to prevent dehiscence, especially after prior radiation or in high-risk patients.
Pelvic support:
- In selected cases, robotic sacrocolpopexy or vault suspension can be combined with oncologic surgery, though more common in benign or prophylactic contexts.
- Use of Y-mesh to attach vaginal apex to sacral promontory, requiring precise needle passage near the midline vessels and presacral nerves.
Bowel anastomosis in cytoreductive procedures:
- Depending on institutional culture, some gyn-onc teams perform intracorporeal stapled and sutured bowel anastomoses robotically; others still prefer a small laparotomy.
Reconstruction in gyn-onc is more varied: vault, bowel, ureter, and sometimes vascular repairs, all potentially robotic. What is common is the use of the robot for deep suturing in awkward angles, especially in the pelvis.

| Category | Value |
|---|---|
| Radical Prostatectomy | 90 |
| Radical Cystectomy | 40 |
| Radical Hysterectomy | 60 |
| Endometrial Cancer Staging | 70 |
| Ovarian Debulking | 30 |
(Values here are illustrative “relative adoption” percentages, not exact epidemiologic data.)
7. Complications and Learning Curves: Different Potholes on the Same Road
Robotics introduces its own complication profile, and the specialties run into different walls.
Urology: Leaks, Strictures, and Nerve Injuries
Typical problem areas:
Anastomotic leaks and strictures:
- Small technical errors during urethrovesical suturing show up later as leaks, prolonged catheter dependence, or bladder neck contractures.
- Robotic finesse reduces risk but does not eliminate it; the learning curve is real (often 50–100 prostatectomies until complication rates plateau).
Erectile dysfunction and incontinence:
- Outcomes depend heavily on:
- Quality of nerve-sparing.
- Blood loss and operative trauma.
- Preservation of sphincter complex.
- Robotic surgery gives the tools, but surgeon judgment about oncologic vs functional trade-off is decisive.
- Outcomes depend heavily on:
Gyn-Onc: Ureteric and Bowel Injury, Vault Issues
Common pitfalls:
Ureteric injuries:
- Thermal or transection injuries during parametrial resection or IP ligament ligation.
- Robotic energy devices allow finer control, but they also can cause delayed strictures if overused near the ureter.
Bowel injuries:
- Especially in reoperative or radiated pelvises during adhesiolysis and debulking.
- The loss of haptic feedback in robotics requires very deliberate visual judgment.
Vault dehiscence:
- Risk increased in postmenopausal, radiated, or immunosuppressed patients; technique and suture choice at cuff closure matter.
The robotic learning curve for gyn-onc can be longer and more heterogeneous because the procedures are less standardized than a prostatectomy. Endometrial staging, radical hysterectomy, ovarian debulking—each has different technical demands.
8. Training and Culture: Who Owns the Robot?
Walk into a mixed OR schedule and you will see one thing quickly: each specialty has territorial instincts around “their” robot.
Urology Training Mindset
- Many urology residents now log a high volume of robotic prostatectomies and partial nephrectomies during residency.
- Fellowships add cystectomy and intracorporeal diversion for those in academic or high-volume centers.
- The teaching is fairly formulaic:
- Standard steps.
- Defined planes.
- Clear metrics: margin rate, continence, potency, blood loss.
Prostatectomy is almost algorithmic at this point in high-volume programs. That can be an advantage for consistency, but it can ossify technique innovation.
Gyn-Onc Training Mindset
- Gyn-onc fellows see a much broader variety of pathology:
- Early endometrial cancer staging.
- Complex ovarian tumor debulking.
- Radical hysterectomy in distorted pelvis (large fibroids, prior surgeries).
- Robotic exposure varies widely between programs:
- Some do nearly all endometrial cancers robotically.
- Others still split between open and minimally invasive, depending on BMI, stage, and surgeon preference.
The downside: less standardization. The upside: gyn-onc surgeons become comfortable using the robot as a general pelvic and abdominal tool, not just a “prostate machine.”
You also see culture differences in comfort with robotic upper-abdominal work: gyn-onc is often more willing to run the robot right up to the diaphragm for stripping or nodal work, while most urologists rarely need to go above the kidney hilum.
9. Future Directions: Where Robotics in These Fields Is Actually Headed
This is supposed to be about the future of healthcare, so let’s get blunt about what is actually coming vs what is marketing.
Platform Evolution and Competition
For both urology and gyn-onc:
- Multiport competitors to da Vinci (Hugo, Versius, others) are entering, pushing:
- Smaller footprints.
- Modular arms.
- Lower per-case costs (eventually).
- Single-port systems:
- Already used in some centers for single-port prostatectomy via a transvesical or perineal approach.
- Potential future in gyn-onc for selected benign or prophylactic cases, less likely for full-on debulking.
Technical nuance: different arm designs will force each specialty to rethink port strategy. Urology’s finely tuned port maps for the Xi will not port directly (no pun intended) to new systems. Same for gyn-onc’s wide, upper-abdominal staging setups.
Image-Guided and Data-Enhanced Surgery
Both urology and gyn-onc are ripe for more integration of imaging and data:
Augmented reality overlays:
- In prostatectomy, fusing pre-op MRI to robotic view to show extracapsular extension and neurovascular bundle location.
- In gyn-onc, mapping sentinel nodes or para-aortic nodal clusters, or highlighting ureter paths in distorted anatomy.
Fluorescence-guided surgery:
- Indocyanine green (ICG) is already used for:
- Sentinel node mapping in endometrial and cervical cancer.
- Assessing bowel perfusion.
- Future iterations: tumor-specific fluorophores to highlight microscopic disease in peritoneal surfaces or lymphatic chains.
- Indocyanine green (ICG) is already used for:
These tools shift the conversation from “surgeon’s eye only” to “surgeon plus quantified visual cues,” which especially helps in fields like gyn-onc where anatomy is distorted by tumor bulk.
Automation and “Digital Assistance”
Do not buy the hype about full autonomy soon, but partial automation is coming:
For urology:
- Semi-automated needle driving during urethrovesical anastomosis based on ideal geometry.
- AI-suggested planes for nerve-sparing based on real-time video plus preoperative MRI inputs.
For gyn-onc:
- Tool use suggestions during para-aortic lymphadenectomy (e.g., warning if proximity to major vessels or ureter is too close).
- Automated clip application for vessel control with safety interlocks.
The big difference: urology’s operations are more standardized and thus easier to “parameterize” for automation. Gyn-onc’s variability makes it harder but also more in need of intelligent guidance.
Cross-Pollination Between Fields
The smart future is not each specialty in a silo. It is:
Gyn-onc borrowing:
- Urology’s extreme precision nerve-sparing mentality for pelvic autonomic preservation in radical hysterectomy.
- Systematic anastomotic techniques for high-risk ureteric reimplantation.
Urology borrowing:
- Gyn-onc’s comfort with wide retroperitoneal dissection, para-aortic work, and upper-abdominal disease evaluation.
- Fluorescence sentinel node mapping strategies and staging philosophies.
You already see this in mixed tumor boards and in surgeons who trained in one field and then gained heavy experience in the other (e.g., pelvic exenterations done jointly by urology and gyn-onc with colorectal).
If institutions are serious about future-proofing, they will stop treating the robot as property of a single service and start training across specialties with shared pelvic labs and simulation.

10. Where This Leaves You
If you are training or practicing in either field and you treat the robot as “we already know how to use it,” you are missing the point. The technical nuances between urology and gyn-onc are not trivial quirks; they are different philosophies of how to approach the same anatomic territory.
Key takeaways:
Port placement and positioning are not cosmetic differences. Urology optimizes for a fixed deep target (prostate/bladder neck). Gyn-onc optimizes for a broad field from pelvis to upper abdomen. Both have to understand the other’s logic if they want to push complex combined cases.
Dissection priorities diverge. Urology uses the robot to squeeze maximal function out of tight margins—nerve-sparing, perfect anastomosis. Gyn-onc uses it to safely widen radical resections and lymphadenectomies in unforgiving anatomic corridors. The future is cross-pollinating these strengths rather than ignoring them.
Robotic platforms will get smarter, but surgeon judgment will still decide the trade-offs between oncologic radicality and functional preservation. AI, AR, and new robots will just amplify whatever philosophy you already bring to the console—so it had better be thoughtful, not tribal.
If you stand in that Friday OR watching urology and gyn-onc fight over the robot, remember: the real future is not who controls the machine. It is who understands the full spectrum of what it can do in the pelvis, across specialties, and uses it accordingly.


















