It’s 1:37 a.m. You’re on YouTube, again, watching another glossy video of a surgeon calmly controlling a massive surgical robot while dramatic music plays in the background. The comment section is all “this is the future,” “surgeons are basically pilots now,” “AI + robotics will replace half of medicine.”
And you’re sitting there thinking:
“I don’t even like cutting.”
“I kind of… love talking to patients?”
Then the spiral starts.
If everything is becoming robotic and procedural and techy, what happens if you don’t pick a procedural field? Are you going to be the “obsolete” doctor? The one doing low-status, low-pay, easily-automated work while your surgery friends post robot console selfies and bank?
Yeah. I know that exact spiral. I’ve watched people go through it on surgery rotations, in late-night group chats, whispering after grand rounds:
“Maybe I should just do urology because… robots?”
“What if hospitalists are replaced by algorithms?”
“Is primary care just going to be triage for AI tools?”
Let me walk through this like someone who is also scared of ending up irrelevant.
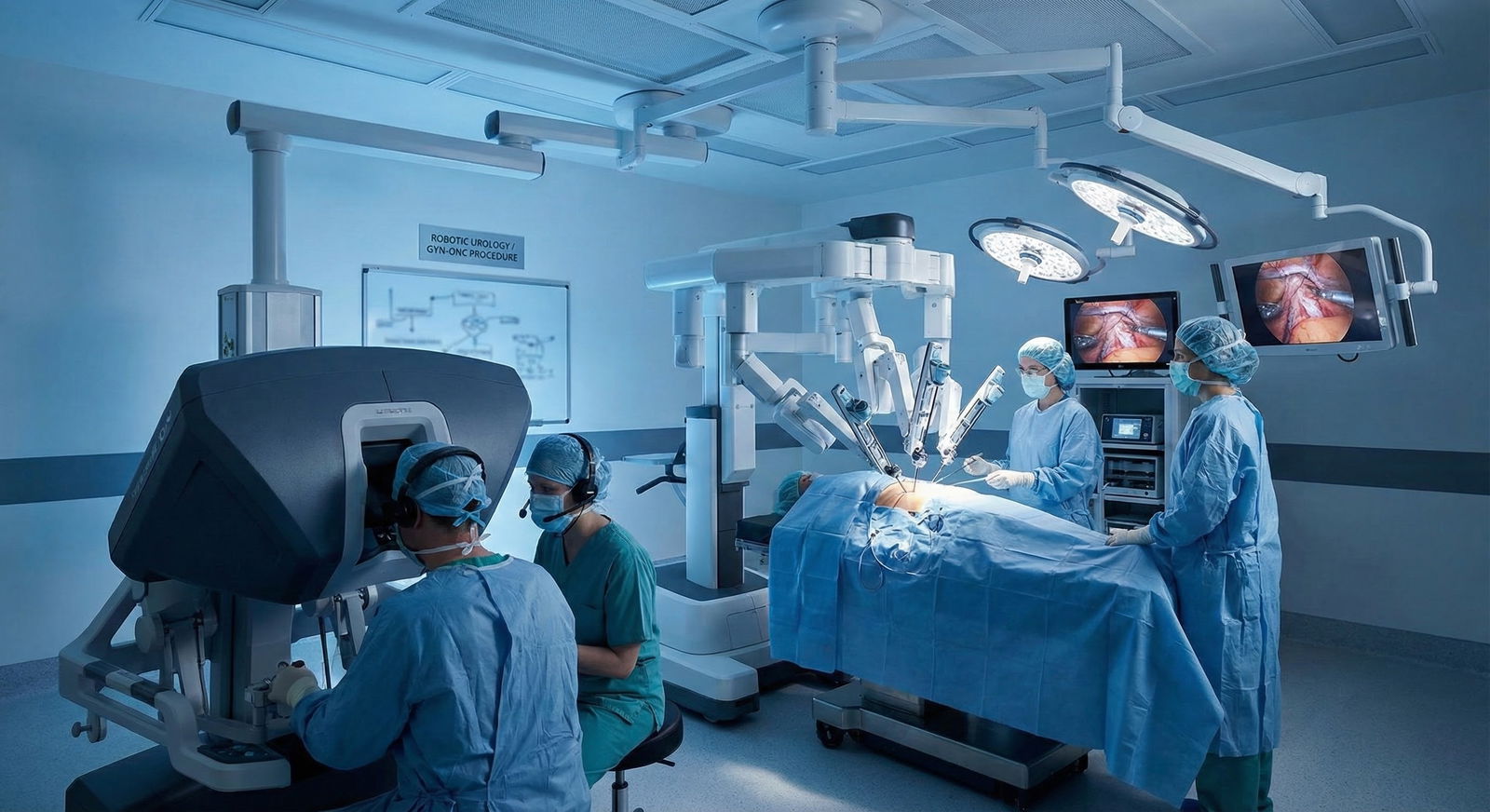
First: What’s Actually Happening With Robots, Not Just Hype
Let’s strip away the marketing videos and admin buzzwords.
Right now, robotic surgery is concentrated in a handful of areas: urology, gynecology, some general surgery (hernia, colorectal, bariatrics), thoracic, some ENT, some cardiac. It’s still surgery. With a console and some fancy arms, yes, but still very much a human surgeon making decisions in real time.

| Category | Value |
|---|---|
| Urology | 30 |
| Gynecology | 25 |
| General Surgery | 20 |
| Thoracic/Other | 10 |
| All Other Fields | 15 |
A few key realities that usually get lost in the anxiety:
- Robotic surgery shifts the way surgery is done. It doesn’t convert non-surgical fields into surgical ones.
- The existence of a robot doesn’t create more procedural specialties. It mostly changes how existing surgeons operate.
- Non-procedural specialties are not becoming robotic-surgery-adjacent. Nobody is adding “robotic control” to psychiatry, rheumatology, or ID.
So if you choose internal medicine, pediatrics, psych, neurology, family medicine, heme/onc, etc., the fear isn’t: “Will I be replaced by a robot surgeon?” It’s more vague: “Is all of medicine becoming ‘tech + procedures,’ and will thinking/talking specialties be devalued or automated?”
That’s the actual worry. And it’s more about AI + algorithms than robots.
The Ugly Fear Underneath: “Am I Choosing the ‘Soft’ Side of Medicine?”
Let’s be honest about status. There’s a hierarchy. You’ve seen it.
People ooh and ahh when someone says they’re going into neurosurgery or ortho. No one gasps and claps for, “I’m thinking about outpatient adult psychiatry” or “Probably hospitalist medicine.” On some rotations, you hear the jabs:
“Medicine just writes for consults and calls us when things get real.”
“Psych is just vibes.”
“FM is for people who couldn’t match something competitive.”
It’s garbage, but you’ve heard it. And now layered on top of that is:
“If I’m not in a field where I control machines and do cool procedures, am I signing up for low-status, low-autonomy, eventually-automated work in a future I don’t control?”
Here’s the blunt truth:
Robotic surgery has amplified a problem that was already there: medicine worships procedures and tech, undervalues cognitive and relational work, and pays accordingly. That’s not news. The robot is just a shiny symbol of it.
But “undervalued” is not the same thing as “disappearing.” And a lot of the future problems in healthcare are exactly in the areas non-procedural fields own.
What Robots (and AI) Actually Suck At Right Now
Everyone talks like AI + robots will just smoothly eat all the “thinking” jobs. I’ve seen the supposed “AI doctor” demos that administrators get all starry-eyed over. Then I’ve watched actual clinicians try to use those tools on real, messy patients.
Here’s what AI/robots are terrible at, and where non-procedural fields quietly become indispensable:
- Context chaos: The 72-year-old with heart failure, CKD, mild dementia, depression, no family support, whose medications are a disaster. Robots don’t untangle that. Hospitalists do. Geriatricians do. PCPs do.
- Value-laden decisions: “Should we proceed with surgery?” in a frail, borderline patient is not just a risk calculator output. It’s values, goals, fear, quality of life. That’s human territory.
- Longitudinal judgment: Knowing a patient over years. Recognizing that “she’s just not herself lately” probably means something serious. AI is pattern-matching; you are pattern recognition plus narrative memory.
- Relationship leverage: Psych, palliative, primary care thrive on trust that you build, not calculate. There is no robot update that substitutes for, “I’ve taken care of you for five years and you trust me enough to tell me what you’re really afraid of.”
That “soft” stuff is exactly what no one has managed to productize. Which is why they wrap robots in pastel marketing about “patient-centered technology.” They’re trying to fake what actual humans naturally do.
So What Happens to Non-Procedural People in a High-Tech World?
Let me answer the darkest version of your question.
“What if I choose a non-procedural field, then 10–15 years from now:
- surgeons are all hyper-glorified,
- AI writes notes and diagnoses,
- admin squeezes cognitive specialties harder,
- and my day is ‘supervised AI + paperwork cleanup’? Did I screw up?”
That fear is not completely insane. Parts of it are already happening in slow motion.
I’ve seen:
- Hospitalists being handed algorithm-driven sepsis alerts like they’re gospel, then blamed when the alert is wrong.
- Outpatient docs told, “The AI will draft your note,” but then they spend just as long fixing nonsense.
- Psychiatrists getting pressure to use rating scales and automated screeners as if they’re definitive.
But there’s a critical pattern: when tools first show up, everyone treats them like magic. Then cracks appear. Then someone has to clean up.
The cleanup is always done by human clinicians. And the ones who understand both the patient and the tech end up with power.
If you go into a non-procedural field, your future isn’t:
- “doing nothing while robots rule.” It’s much more likely:
- “doing your same core work, but with new tools that are sometimes useful, sometimes stupid, and often make your work more necessary because the system over-trusts them.”
The people who are most crushed aren’t “non-procedural” people. They’re the ones who don’t understand what their actual irreducible value is and try to compete with machines at what machines do better.
You are not going to out-speed a diagnostic algorithm at running a differential in 0.3 seconds. You will outclass it at:
- framing the problem,
- spotting when it’s wrong,
- balancing tradeoffs,
- and actually talking to the person attached to the data.
That’s… medicine.
Don’t Romanticize Robots and Demonize Non-Procedural Work
I’ve watched med students think robotic surgeons are basically sci‑fi heroes. Then they rotate with them and see the other side:
- Endless credentialing hoops.
- System pressure to use the robot even when maybe it’s not necessary, because, billing.
- Extra time in the OR for straightforward cases that could be faster laparoscopically.
- Long cases, physical strain, and surprisingly monotonous parts.
Meanwhile, the supposedly “unsexy” non-procedural folks are:
- running rapid family meetings that completely change goals of care,
- stabilizing complex decompensations on the floor,
- managing polypharmacy better than any decision support tool,
- catching subtle early signs of deterioration before the vital signs flag.
It’s not glamorous, but it’s where people’s lives actually pivot.
You won’t see TikToks about “hospitalist saved this patient by changing the entire plan based on a 5-minute conversation.” But you will see that exact scenario 100 times in real life if you go into internal medicine.
Comparing Paths: Procedural vs Non-Procedural in a Robotic Era
Let’s put some structure to the chaos in your head.
| Aspect | Procedural (e.g., surgery) | Non-Procedural (e.g., IM, Psych) |
|---|---|---|
| Tech Trend | More robotics, devices, image guidance | More AI support, decision aids, remote monitoring |
| Core Value | Technical skill + intra-op decision-making | Complex judgment + longitudinal relationships |
| Automation Risk | Some technical components may be assisted/augmented, but human oversight required | Administrative and rote tasks at risk; core cognitive/relational work harder to replace |
| Lifestyle | Front-loaded training, physically demanding, call-heavy | Variable; more options for outpatient, telehealth, portfolio careers |
| Future Leverage | Those who master tech + policy will lead robotics programs | Those who own care coordination + narrative + system thinking will shape models of care |
Neither column says “becomes useless.” They both say: changes. Shifts. Demands adaptation.
The real decision isn’t: “Do I bet on robots or not?”
It’s: “What kind of hard do I want? What kind of irreplaceable do I want to become?”
Where Non-Procedural Fields Quietly Win in the Future
If I strip away your fear and just look at the system, the cracks forming in healthcare are glaring:
- Aging populations with multi-morbidity.
- Mental health crises.
- Chronic disease dominating cost and suffering.
- Fragmented care where no one actually knows the whole patient.
- Burnout from schedule-by-spreadsheet medicine.
Those aren’t “robot problems.” They’re human coordination, motivation, meaning, and judgment problems.
Who’s actually best positioned there?
Not the robot-console people. Not the imaging-only folks.
It’s:
- primary care,
- hospital medicine,
- psychiatry,
- geriatrics,
- palliative care,
- heme/onc,
- complex care pediatrics,
- ID,
- and even seemingly “niche” things like allergy/immunology or rheumatology, where the whole job is persistent, nuanced management.
AI might help you:
- risk-stratify,
- suggest diagnoses,
- flag concerning labs earlier,
- predict readmissions.
But someone still has to:
- negotiate with the patient who doesn’t want to be admitted again,
- manage the family who’s in denial,
- sort out whether the AI’s suggestion actually fits this person’s story,
- own the outcome.
That person is very likely in a non-procedural field.
Money, Status, and the “Will I Regret This?” Question
I’d be lying if I said money and status don’t matter. They do. Being underpaid and dismissed by your own institution sucks. Watching procedural colleagues pull in double your income for fewer years of training can feel brutal.
Will robotic surgery widen that gap? Maybe in certain places, yes. Hospitals market the hell out of robotics and surgeons who can do high-margin cases will remain extremely valuable.
But non-procedural fields aren’t just sitting there static either. There’s:
- Growing recognition that preventive and chronic care is financially crucial because admissions are expensive.
- More value-based care models that pay for keeping people out of the OR and the ICU.
- Telehealth and hybrid models that give cognitive specialties more flexibility, more patient reach, and in some setups, better compensation.
Is it perfect? No. Is it still unfair? Very often, yes. Could that make you regret not going procedural if you’re very money-driven? Possibly.
But I’ve seen something else repeatedly:
People who dragged themselves into a procedural field they didn’t love—for the status, the perceived future “safety,” the tech appeal—turn out miserable. Burned out, resentful, and sometimes trapped because they can’t imagine starting over.
Regret cuts both ways.
You can regret chasing what looks flashy just as much as you can regret not doing it.
Practical Ways to Future-Proof a Non-Procedural Career
If you do choose a non-procedural field and you’re still thinking, “Okay, but how do I not get steamrolled by tech and robots and admin insanity?” there are concrete things you can do.
You can:
- Learn enough about AI/tech to be dangerous. Not “become a data scientist,” but understand what tools can and can’t do, so you can call BS and help shape how they’re used.
- Position yourself where cognitive work is central: complex inpatient medicine, consultative subspecialties, serious mental illness, geriatrics, palliative—anywhere nuance is nonstop.
- Build skills robots will never have: conflict mediation, serious illness conversations, motivational interviewing, culturally grounded care. Those are future currency.
- Get involved in quality improvement, policy, or informatics within your field, so you’re on the side designing workflows, not just suffering under them.
You don’t have to do all of that now. Just… don’t go into a non-procedural specialty planning to be a human checklist that an algorithm could replace. Lean into the chaos and the human parts.

The Bottom Line: Are You Screwed If You Don’t Choose a Robotic Field?
No.
You’re not “missing the future” by choosing a non-procedural specialty. You’re choosing a different front line of the future.
Robots will reshape surgery. AI will reshape every specialty. But they don’t flip the basic truth that medicine is about:
- making sense of messy humans,
- helping them make decisions under uncertainty,
- and stepping in when things fall apart.
That’s non-procedural medicine’s home turf.
If your gut lights up more for:
- complex stories than for anatomy diagrams,
- family meetings more than console time,
- slowly unraveling a patient’s life and disease over years rather than one decisive moment in the OR,
then hiding from that because robots look cool is a terrible long-term trade.
Will non-procedural fields have to fight harder for recognition, fair pay, and sane working conditions? Yes. They already do. But they’re also where a lot of the most irreplaceably human work will live.
So no, you’re not betraying the “future of medicine” by choosing a non-procedural path in a robotic surgery era.
You’re just betting that, in the end, medicine will still need people who actually know patients, not just operate on them.
Key points to walk away with
- Robotic surgery changes how surgeons operate; it doesn’t erase the need for non-procedural specialties—if anything, it makes complex medical, mental health, and longitudinal care more central.
- AI and tech will eat paperwork and pattern-matching before they touch deep judgment, relationship, and values-based decision-making. That’s the core of non-procedural work—if you lean into it.
- Choosing a specialty you actually fit, even if it’s “non-robotic” and less flashy, is a better long-term bet than forcing yourself into a procedural field just because it looks like the future.


















