It is September. Your Step 2 CK just came back lower than you hoped. Your friends are bragging about “only applying to 40 programs” while your brain is screaming, “Do I need to apply to 120? 200?” You have five different Reddit threads open, a half-built spreadsheet, and zero actual decisions.
Here is where you are:
You cannot change your score. You can change how you use it.
This is a numbers game and a strategy game. You win it by adjusting:
- How many programs you apply to
- Which tiers you target
- How you use your money and time intelligently, not out of fear
I am going to walk you through that. Step-by-step. No fluff.
1. Get Your Situation on Paper First (Brutally, Not Emotionally)
Before you decide “how many programs,” you need to know what kind of applicant you are. Not how you feel. How you actually look on paper to programs.
Grab a sheet or open a spreadsheet and write down:
Specialty:
- If you are thinking EM, Derm, Ortho, Plastics, or ENT with low boards – different conversation, higher risk.
- If you are applying IM, FM, Peds, Psych, Path, Neuro, PM&R – you have more room to maneuver.
Board scores:
- Step 1: Pass / Fail (if numeric, still matters for some older attendings, but Step 2 rules now)
- Step 2 CK: exact number
Red flags:
- Any Step failures (Step 1, Step 2, COMLEX)
- Any course repeats, LOAs, professionalism issues
School type:
- US MD
- US DO
- Caribbean / International (IMG/FMG)
Extra ammo:
- Research (number of pubs/posters)
- Strong letters (from big names or PDs)
- Home program in that specialty
- Away rotations with strong performance
Now define yourself honestly in one sentence:
- “US MD, Step 2 = 226, no fails, IM, strong home program, some research.”
- “US DO, Step 2 = 215, COMLEX average, applying FM, no fails.”
- “Caribbean IMG, Step 2 = 228, one attempt on Step 1, applying IM, one US rotation.”
That sentence matters. Because “how many programs” is not the same number for all of those.
2. Understand What “Low Boards” Actually Mean by Specialty
You cannot plan if “low” is just a feeling. Anchor it with reality.
| Specialty Type | Typical Matched Step 2 Range | What Counts as 'Low' Here |
|---|---|---|
| Very Competitive (Derm, Ortho, ENT, Plastics, Ortho, Urology) | 250+ | Below ~240 |
| Competitive (EM, Anesth, Gen Surg, Rad, OB/GYN) | 240–250 | Below ~235 |
| Moderate (Neuro, PM&R, Path, Psych) | 235–245 | Below ~230 |
| Less Competitive (IM, FM, Peds) | 225–240 | Below ~220 |
These are ballpark, not commandments. But they frame your risk level.
Combine that with applicant type:
- US MD with 225 in IM = slightly below average, still fine with good strategy.
- US DO with 215 in FM = absolutely matchable, but you need enough applications.
- IMG with 235 in IM = still “lowish” in IM-IMG world; you must go broad.
Now add one more reality check:
Programs care more about:
- Passing on first attempt
- Consistency (not wildly uneven scores)
- Evidence you will pass boards as a resident
So:
- One failure + low Step 2 = high risk.
- No failures + borderline Step 2 = manageable with volume and targeting.
3. The Core Principle: You Are Buying Interview Lotteries
You do not apply to “X programs.” You buy “Y chances” at interviews.
Interviews—not raw application numbers—predict matching.
Let me simplify the math the way PDs and advisors actually think:
- For most core specialties (IM, FM, Peds, Psych, Path, Neuro, PM&R), if you:
- Get 12–15 interviews, your chance of matching is very high.
- Get 8–10, your chance is moderate.
- Get <6, you are in real danger.
With low boards, the lever you control is:
How many lines in the lottery you buy.
So the real question is:
“Given my profile, how many applications do I need to send to likely generate 12–15 interviews?”
That depends on:
- Your hit rate: % of programs that actually invite you
- Your specialty competitiveness
- Your applicant type (US MD vs DO vs IMG)
- Geographic limits (are you willing to go anywhere?)
4. Concrete Ranges: How Many Programs to Apply to (By Category)
Here is what you came for. Numbers. I will assume low boards, but no catastrophic transcript issues.
A. Internal Medicine (Categorical)
US MD, Step 2 < 225, no fails
- If no big red flags:
- Target: 40–60 programs
- If Step 2 close to 210–215 or mild concerns:
- Target: 60–80
- If no big red flags:
US DO, Step 2 < 225, no fails
- Community-heavy, geographically flexible:
- Target: 60–90
- If regional only or poor clinical comments:
- Target: 80–100
- Community-heavy, geographically flexible:
IMG with Step 2 < 235 or any attempt
- Willing to go anywhere, include smaller community programs:
- Target: 120–160
- Strong US clinical experience + some research may allow:
- Target: 100–140
- Willing to go anywhere, include smaller community programs:
B. Family Medicine
US MD, Step 2 < 220
- Generally safe if you are flexible geographically:
- Target: 25–40
- If Step 2 near 205–210 or academic issues:
- Target: 40–60
- Generally safe if you are flexible geographically:
US DO, Step 2 < 220
- Target: 40–60, sometimes 60–80 if multiple concerns.
IMG, Step 2 < 230
- Target: 80–120, broad geographic spread.
C. Pediatrics
- US MD, Step 2 < 220
- Target: 40–60
- US DO
- Target: 50–70
- IMG
- Target: 90–130
D. Psychiatry, Neurology, PM&R, Pathology
These fluctuate by region. But with low boards:
US MD
- Psych / Neuro / PM&R: 40–60
- Path: 30–50 (but watch for programs with recent cutoffs)
US DO
- Psych / Neuro / PM&R: 50–70
- Path: 40–60
IMG
- Psych / Neuro / PM&R: 80–120
- Path: 60–100
E. Surgery / OB / EM / Anesthesia with Low Scores
With genuinely low Step 2, these become high-risk unless you have serious compensating strengths (home program support, strong aways, research, known to PDs).
Rough starting points:
- US MD, low Step 2 (< 230)
- Gen Surg / OB / EM / Anesthesia: 60–90
- US DO
- 80–120, depending on region and support
- IMG
- Often not realistic to match categorical without exceptional factors. At that point, you need individualized advising, not generic numbers.
5. Calculate Your Number, Not a Generic One
Let us make this less abstract. Estimate your own “hit rate” based on risk level.
Use this rule-of-thumb for low-board applicants:
- Relatively low risk (just slightly under average):
- Expect 8–15% of programs you apply to might offer interviews.
- Moderate risk (clear low boards, but no fails):
- Expect 5–10%.
- Higher risk (low boards + attempts or IMG):
- Expect 2–6%.

| Category | Value |
|---|---|
| Low Risk | 12 |
| Moderate Risk | 7 |
| High Risk | 4 |
Now do simple math:
- Goal: 12 interviews
- If you think you are:
- Low risk (12% hit): 12 / 0.12 ≈ 100 programs
- Moderate risk (7% hit): 12 / 0.07 ≈ 170 programs
- High risk (4% hit): 12 / 0.04 ≈ 300 programs (for IMGs in competitive areas, that is not absurd)
But that is the upper bound. Most core US MD / DO low-board applicants will not need 170+.
You tailor:
- Pick your goal number of interviews: 12–15.
- Be honest about risk tier.
- Use the math above to sanity-check your plan.
- Then adjust down if:
- You have a strong home program likely to rank you.
- You have multiple aways where PDs explicitly said “we will rank you.”
- You have unique strengths (publications, advanced degree, local ties).
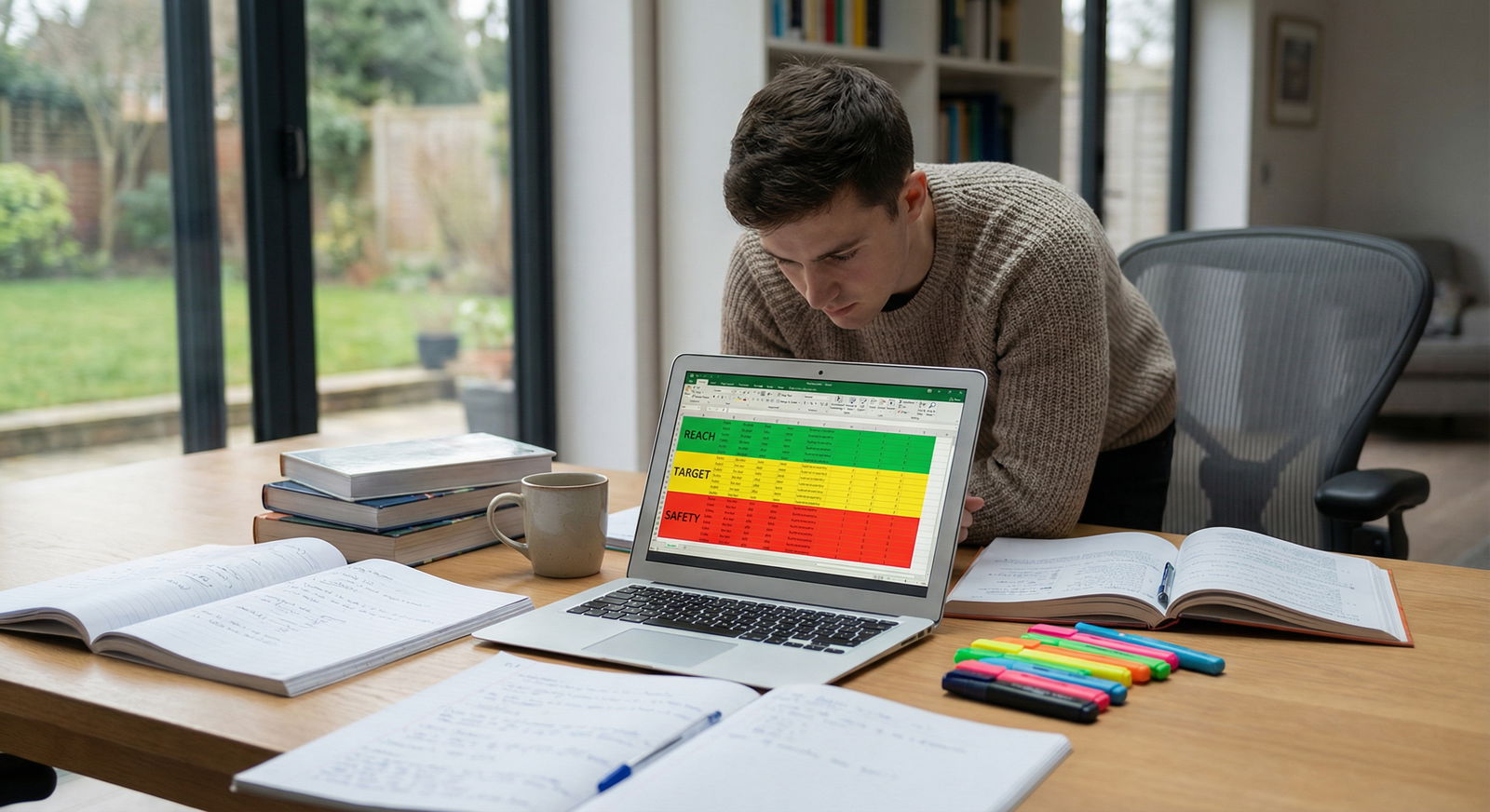
6. Stop Panicking: Use Tiers, Not Spray-and-Pray
Blindly applying to 150 programs is not strategy. It is anxiety with a credit card.
You need three tiers:
- Reach programs – slightly to clearly above your stats.
- Target programs – realistically within your range.
- Safety programs – tend to rank applicants like you reliably.
A reasonable distribution for low-board applicants:
- 20–30% reach
- 50–60% target
- 20–30% safety
If you only change one thing from how most people do this, do this:
Increase the safety slice, not the reach.
How to Tier Quickly (Without Wasting Three Days on Freida)
- Use:
- FREIDA
- Residency Explorer
- Program websites
- Look at:
- Their reported average Step 2 (or Step 1 historically)
- % of IMGs / DOs they take
- Reputation (basic sense: university vs community vs rural community)
Then do this:
- Reach = programs where you are clearly below their typical numbers or where they rarely take your applicant type.
- Target = programs where you are near their average or they regularly interview your applicant type and range.
- Safety = programs that:
- Have historically matched multiple applicants like you (same school/type and range), and
- Are community or less competitive geographic locations.
If you are an IMG or low-score DO, safety often means:
- Community-heavy
- Non-coastal
- Historically IMG/DO-friendly
- Newer programs (but not brand-new this cycle if you can avoid it)
7. Don’t Let Money and Time Kill Your Strategy
Applications cost real money. But anxiety-based overapplication is a giant, common mistake.
A. Know Your Cost Curve
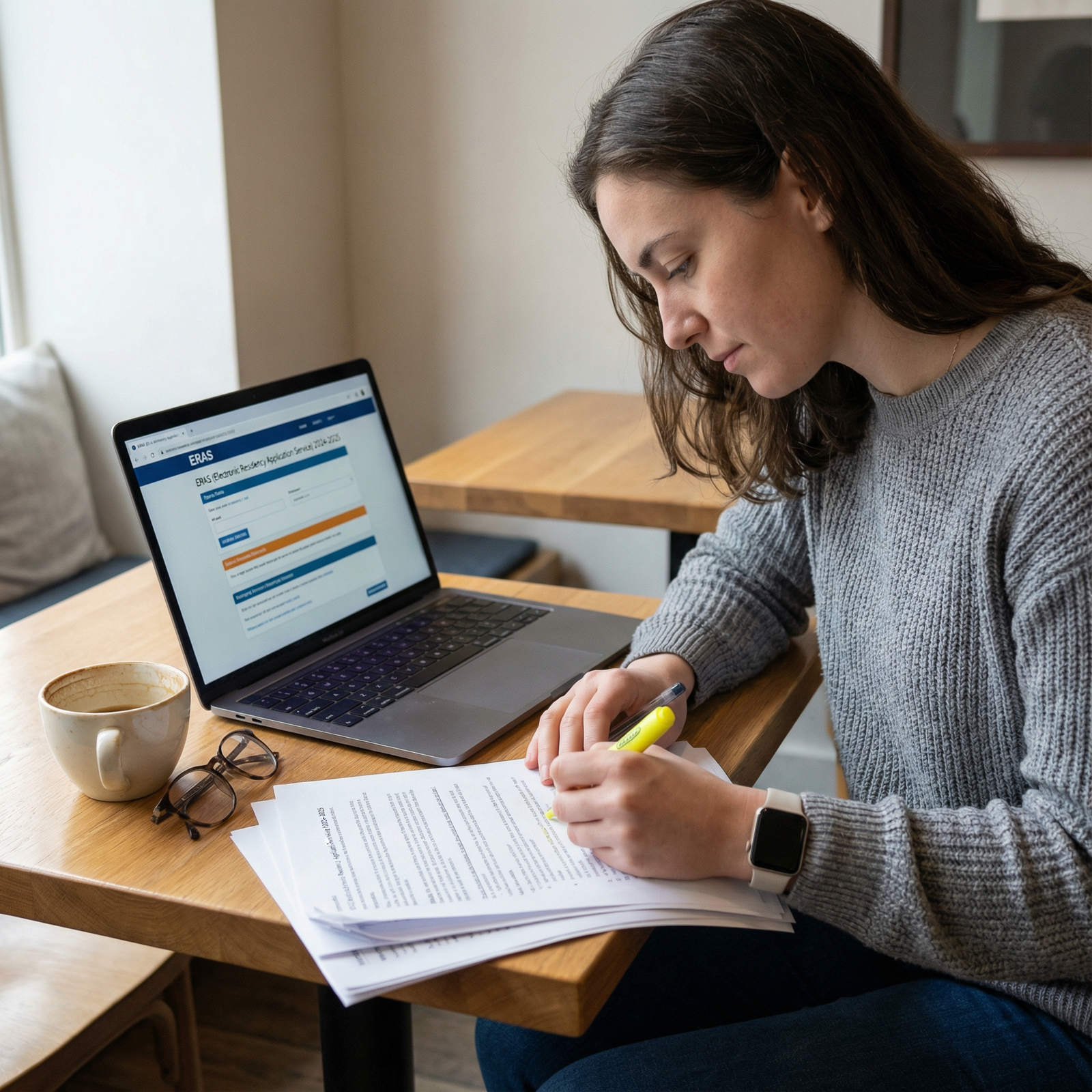
ERAS charges by number of programs per specialty. It ramps up fast.

| Category | Value |
|---|---|
| 10 | 99 |
| 20 | 219 |
| 40 | 579 |
| 60 | 939 |
| 80 | 1299 |
| 100 | 1659 |
(These are approximate, not exact. But the trend is real: the more you add, the more each additional program costs.)
You must decide:
- “Is adding 20 more programs (~$300+) likely to net me one more interview?”
- If yes, and you can afford it, maybe worth it.
- If your list is already 120 IM programs as a US MD with a 222 Step 2, those extra 20 may do nothing.
B. Hard Budget, Smart Choices
Do this:
- Decide a max total spend on ERAS before you add a single program.
- Work backward:
- If you want to apply to two specialties, split that budget from the start.
- Force ranking:
- Sort programs by priority (fit + likelihood) and apply top-down.
- If you hit budget at 80 programs, you stop. Not negotiable.
8. Build Your Program List in 3 Passes (Fast and Logical)
Here is a simple 3-pass method that prevents chaos.
Pass 1 – The Obvious Core List (30–50 Programs)
Add:
- Every program in your home region that:
- Has your specialty.
- Does not have explicit score cutoffs way above yours.
- Any program:
- Where you did a rotation.
- Where you know faculty.
- Where your school historically sends grads with similar stats.
Pass 2 – Safety / “Workhorse” Programs
Now, intentionally load your list with safety and solid community programs.
Criteria:
- IMGs/DOs in prior classes (if you are one).
- Average Step 2 not far above yours.
- Non-coastal, midwestern, southern, or rural areas often fall here.
This should be another 30–70 programs depending on your risk level and specialty.
Pass 3 – Reach and “Why Not” Programs (But Controlled)
Sprinkle in 20–30% reach programs:
- A few academic centers.
- A few programs in ideal cities where you have personal ties (partner job, family).
If you find yourself adding 40 reach and 10 safety, you are backwards. Fix it.

| Step | Description |
|---|---|
| Step 1 | Start |
| Step 2 | Pass 1 - Core list |
| Step 3 | Pass 2 - Safety and workhorse |
| Step 4 | Check total count and budget |
| Step 5 | Pass 3 - Controlled reach |
| Step 6 | Final review and submit |
9. How to Adjust Program Count After You Feel Panic Rising
You will hit this stage:
You built a list. You still feel like you did “too few.” Your brain whispers, “Everyone else is applying to 150+.”
Here is the protocol.
Step 1 – Reality Check Against Your Profile
Ask:
- What is my applicant type and specialty?
- Based on your profile, compare to ranges earlier.
- If you:
- Are US MD, lowish boards, in IM/FM/Peds/Psych, and already at 60–80 programs – throwing it to 140 is probably fear, not strategy.
Step 2 – Add Intelligently, Not Blindly
If you truly undershot:
- Add safety-first, not reach.
- Add in geographic areas you have not touched (Midwest, South, rural).
Good adds:
- Community hospitals
- University-affiliated community programs
- Programs with history of taking your applicant type
Bad adds:
- Famous university names you would love but that almost never take someone with your stats.
- Highly desirable city programs that are essentially reaches.
Step 3 – Stop Once Your Risk-Adjusted Number Is Hit
Once you are inside the reasonable band for your applicant type, stop.
There is a point where each incremental application has almost zero chance of turning into an interview. At that point, your time is better spent:
- Tightening your personal statement
- Polishing your experiences
- Asking letter writers to update or strengthen content
- Targeted emails to PDs or PCs in late October/early November if interviews are slow
10. Special Cases: Dual Applying and Backup Plans
If your scores are truly low for your chosen specialty, dual applying can be smart. It can also backfire if you split too much attention.
Here is the rule:
- Your primary specialty still gets the majority of applications.
- Your backup specialty gets enough to be viable, not symbolic.
Example:
- US MD, low boards, wants EM but borderline → EM + IM
- EM: 40–60
- IM: 40–60
- DO, low boards, wants OB → OB + FM
- OB: 40–60
- FM: 30–40
Do not apply to ten programs in a backup specialty and pretend that is safety. If the backup is needed, you will need a legitimate interview count there too.

11. What To Do If Interviews Are Not Coming
You applied. It is late October. Your email is quiet. This is the part where people really start panicking and want to add 40 more programs randomly.
Here is a calmer protocol.
A. Check Your Numbers
- How many applications did you send?
- How many interview invitations have you received?
Then:
- If you are under 5 interviews by mid-November, consider:
- Adding more safety programs if budget allows.
- Focusing on programs that:
- Just started or are newer.
- Have a higher percentage of your applicant type.
B. Targeted Communication
For programs you already applied to:
- Send a concise, respectful email to the program coordinator or PD:
- Reaffirm interest.
- Highlight one or two specific things that make you a fit.
- If you have an update (Step 2 score improved, new publication, strong rotation eval), include it.
No begging. No paragraphs about how you “just want a chance.” Professional, brief, specific.
C. Avoid Desperation Moves
Things that rarely help:
- Mass-emailing every PD with generic “I’m very interested” lines.
- Adding 30 more reach programs late in the season.
- Rewriting your personal statement 5 times instead of sending targeted updates.
12. Mental Reset: Low Board Scores Are a Problem, Not a Verdict
I have watched plenty of applicants with “bad” scores match because they treated the score as:
- A risk factor to manage
- Not a character judgment
- Not a reason to roll over and accept any plan someone else suggests
The people who get burned are the ones who:
- Under-apply out of pride (“I do not want to apply to community programs”).
- Over-apply blindly, then under-prepare for interviews.
- Ignore safety programs and hope prestige will magically ignore their stats.
Your job is not to feel good about the number. It is to make ruthless, calm decisions with it.
Key Takeaways
- Define your actual risk profile (specialty + scores + applicant type), then pick a realistic target range for total applications.
- Build a tiered list with a heavy dose of safety and target programs; control reach programs so they do not crowd out your realistic options.
- Set a budget, apply strategically, and only adjust numbers upward in a controlled, safety-focused way rather than panicking and spraying more applications at long-shot programs.
FAQ
1. I am a US MD with Step 2 in the low 220s applying to IM. Do I really need more than 80 programs?
Probably not, if you build the list correctly. If you cover a broad geographic spread, include a healthy number of community and university-affiliated community programs, and you have no major red flags, 60–80 is usually sufficient. What matters more is the composition of those programs—enough safety and realistic targets—rather than inflating to 120 applications filled with reaches.
2. I am an IMG with a 230 applying to IM. People are telling me to apply to 250+ programs. Is that overkill?
It can be, but not always. If you have strong US clinical experience, no exam failures, and solid letters, you can usually aim in the 140–180 range if you are geographically flexible and heavily weight IMG-friendly programs. Going above 200 is sometimes justified if you have attempts or weak clinical exposure, but for many IMGs at 230 with a clean record, 250+ is more fear than strategy. The key is focusing on the right types of programs, not just inflating the count.






















